![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
58 Cards in this Set
- Front
- Back
|
Common fractures and dislocations usually apply to which areas?
|
limbs
shoulder girdle pelvic girdle |
|
|
The golden rule is if in doubt:
|
X-ray
|
|
|
A fracture usually causes deformity but may cause nothing more than
|
local tenderness over the bone
(e.g. scaphoid fracture, impacted fractured neck of femur). |
|
|
The classic signs of fracture are:
|
—pain
—tenderness —loss of function —deformity —swelling/bruising —crepitus |
|
|
x-ray views of the upper limb should include:
|
joints proximal or distal to the injury
x-rays in both AP & lateral planes |
|
|
If an X-ray is reported as normal but a fracture is strongly suspected, one option is to ...
|
splint the affected limb for 10 days & repeat the X-ray
|
|
|
Displaced fractures are reduced so that
|
bone ends are placed in alignment & immobilised until union occurs
|
|
|
Fractures should be monitored radiologically for
|
loss of position (particularly in the first 1-2 weeks after reduction)
|
|
|
Bone union is assessed clinically by
|
reduced pain at the fracture site and reduced fracture mobility
|
|
|
Bone union is assessed radiologically by
|
X-ray features such as trabecular continuity across the fracture site and bridging callus
|
|
|
Non-union is caused by factors such as
|
inadequate immobilisation
excessive distraction loss of healing callus infection avascular necrosis |
|
|
A common problem with immobilisation in plaster casts and slings is
|
stiffness of joints
ie. must be moved as early as possible, if the fracture is stable |
|
|
Define dislocation.
|
complete disruption of one bone relative to another at a joint
|
|
|
Define subluxation.
|
partial displacement such that the joint surfaces are still in partial contact
|
|
|
Define sprain.
|
partial disruption of a ligament or joint capsule
|
|
|
Associated soft-tissue injuries to consider:
|
neuropraxia to adjacent nerves
vascular injuries muscle compartment syndromes |
|
|
Define stress fracture.
|
incomplete fracture resulting from repeated small episodes of trauma, which individually not be sufficient to damage the bone
|
|
|
Stress fractures (esp. foot) are most likely to result from
|
sport, ballet, gymnastics and aerobics
Their incidence rises sharply at times of increased activity. |
|
|
Typical stress fractures (with their usual cause) include:
|
—navicular (sprinting sports, football)
—metatarsal neck (running, walking, basketball, jumping) —base of fifth metatarsal (dancing) —femur—neck or shaft (distance running) —ulna (weight-lifting) —distal radial and ulnar epiphyses (gymnastics) —talus (running) —proximal tibia (running, football) —medial tibia (running, football) —distal phalanges (guitar playing) —cervical spinous process (gardening) —lumbar vertebrae—pars interarticularis (fast bowling) —spiral humerus (throwing sports) —rib fractures—1st (weight-lifting) —rib fractures—8th (tennis) |
|
|
The key strategy of most reduction manoeuvres is
|
traction (especially for dislocations)
may be supplemented with translation/leverage |
|
|
Red flags for fractures
|
Supracondylar fracture in children
Elbow fractures in children, especially lateral humeral condyle ‘Trampoline’ injuries in children Scaphoid fracture Scapholunate dislocation Skull fractures, especially temporal Talar dome fractures All intra-articular fractures Avascular heads of humerus and femur |
|
|
Define arthroplasty
|
total joint replacement
(most last 10-15 years) |
|
|
Define arthrodesis
|
joint fusion with removal of articular surfaces
|
|
|
Define osteotomy
|
cutting bone to realign joint surfaces
|
|
|
Examination of fractured extremities?
|
1. Inspect
2. Neuro (movement, sensation) 3. Vascular (pulses, capillary refill) |
|
|
Which x-rays should be obtained if fracture is suspected?
|
2 views
AND x-rays of the joint above & below |
|
|
How are fractures described?
|
1. Skin status (open/closed)
2. Bone (thirds: proximal, middle, distal) 3. Pattern 4. Alignment (displacement, angulation, rotation) |
|
|
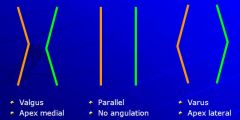
How is bone alignment described?
|
Displacement (anterior/posterior/medial/lateral)
Angulation (varus/valgus) Rotation (internal/external) *relative to the proximal bone |
|
|
How would you describe the angulation of bone?
|
|
|
|
knock knees =
|
genu valgus
|
|
|
bowlegged =
|
genu varum / varus
|
|
|
What are the major orthopedic emergencies?
|
- open fractures
- vascular injury - neuro compromise - infection (osteomyelitis/septic arthritis) - hip dislocation - exsanguinating pelvic fracture |
|
|
What is the main risk in an open fracture?
|
infection
|
|
|
Which fracture has the highest mortality?
|
pelvic fracture
|
|
|
What factors determine the extent of injury?
|
- age
- direction - magnitude |
|
|
what is the susceptible point for a fracture in a child?
|
growth plate
|
|
|
what is the susceptible point for a fracture in an adolescent?
|
ligaments
|
|
|
what is the susceptible point for a fracture in the elderly?
|
metaphysis
|
|
|
What are the indications for open reduction?
|
NO CAST
Nonunion Open fracture Compromise of blood supply Articular malalignment Salter-Harris grade 3/4 Trauma patients needing early ambulation |
|
|
What are the steps in the initial treatment of an open fracture?
|
1. antibiotic prophylaxis (G+ve ± anerobic)
2. surgical debridement 3. tetanus vaccine 4. wound lavage with high pressure sterile irrigation (<6 hours postincident) 5. open reduction & stabilisation |
|
|
What structures are at risk in a humerus #
|
radial nerve
brachial artery |
|
|
Mx if both forearm bones are broken
|
ORIF
|
|
|
Mx of femur #
|
intramedullary rod placement
OR traction for 4-6 weeks (previously) |
|
|
What is the main concern post tibial fractures?
|
compartment syndrome
|
|
|
What is suggested by pain in the anatomic snuffbox?
|
scaphoid #
|
|
|
What is the most common cause of a pathologic fracture in adults?
|
osteoporosis
|
|
|
What is acute compartment syndrome?
|
↑ pressure leading to ischemic necrosis
|
|
|
How is compartment syndrome diagnosed?
|
Clinically! (6 "Ps")
Pain with passive movement (early, severe, deep, constant, poorly localized, out of proportion, not relieved by even morphine) Pallor (cyanosis) Paresthesia (followed by anaesthesia as a late sign) Pressure (firm, swollen, prolonged capillary refill) Paralysis (late) Pulselessness (rare) ± measurement of intracompartmental pressures |
|
|
When should fasciotomy for compartment syndrome be performed?
|
>30-40 mmHg difference between intracompartmental pressure and diastolic BP
|
|
|
Causes of compartment syndrome
|
fracture
vascular compromise reperfusion injury compressive dressings (can occur after any MSK injury) |
|
|
common causes of forearm compartment syndrome
|
supracondylar humerus #
radius/ulna # injury to brachial artery crush injury |
|
|
Complications of compartment syndrome?
|
ischemic necrosis → nerve damage → rhabdomyolysis → myoglobinuria → renal failure
Volkmann's contracture |
|
|
Volkmann's contracture
|
permanent flexion contracture of the hand at the wrist, resulting in a claw-like deformity of the hand & fingers
|
|
|
What is the most common site of compartment syndrome?
|
calf
(4 compartments: anterior, superficial/deep posterior, lateral) |
|
|
In what conditions would you monitor for the development of compartment syndrome?
|
arterial/venous disruption
electrical burns proximal/midshaft tibial # supracondylar elbow fractures in children |
|
|
Can a patient have compartment syndrome with a palpable / Doppler detected distal pulse?
|
YES
|
|
|
What is the definitive treatment of compartment syndrome?
|
fasciotomy within 4 hours (6-8 hours max)
|
|
|
What is the initial treatment of compartment syndrome in an orthopedic patient?
|
loosen tight clothes/dressings
split casts place extremity at heart level |

