![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
29 Cards in this Set
- Front
- Back
|
What is vital capacity?
|
Volume of gas expired when going from TLC to RV.
|
|
|
Spirometry can measure _____.
|
Vital Capacity
|
|
|
Spriometry cannot measure _______.
What tests must be used instead? |
Spirometry cannot measure volumes dependent on gases within the lungs, ex: RV, FRC, TLC. Need dilution tests or body plethysmography.
|
|
|
How does dilution testing work?
|
Inhale inert gas (helium), diluted by gas in lungs, measure concentration of expired gas--reflects initial volume of gas in lungs.
|
|
|
Why is body plethysmography a more accurate reflection of intrathoracic gas?
|
Doesn't depend on ready communication of all peripheral air spaces with bronchial tree
|
|
|
What is the midexpiratory flow rate?
|
Rate of airflow during middle one-half of expiration (b/t 25 and 75% of volume expired during FVC).
|
|
|
What factor most effects diffusing capacity?
Other factors? |
Number of alveolar-capillary units (SA available for gas exchange)
Other factors: volume of blood (Hgb), thickness of capillary membrane |
|
|
What pulmonary conditions decrease DLCO?
|
Emphysema, interstitial lung dz, pulm vasc dz
|
|
|
What pulmonary conditions exhibit a normal DLCO?
|
Asthma, chronic bronchitis--only airways affected, not parenchyma
|
|
|
What pulmonary conditions exhibit an increased DLCO?
|
Asthma, pulmonary hemorrhage, polycythemia, left-to-right shunt
|
|
|
Normal range for FEV1/VC?
What does this value mean? |
Normal FEV1/VC = 0.7 or greater
An individual without lung dz should, during firxt second of max exhalation, be able to exhale at least 70% of total volume exhaled. Decreases with age. |
|
|
Obstructive vs Restrictive Patterns:
General Expected PFT Values (lung volumes, expiratory force, diffusion capacity) |
Obstructive:
-airflow obstruction, diminished expiratory flow -Asthma, chronic bronchitis, emphysema, bronchiolitis, bronchiectasis -Low FEV1/FVC, Low MMFR -High RV, RV/TLC ratio (air trapping due to closure of airways) -DLCO inc'd in emphysema, perserved in asthma/bronchitis Restrictive: -interstitial dz -dec'd lung vols, no airflow obstruction, preserved expiratory flow -MMFR, FEV1/FVC preserved -Low DLCO |
|
|
What lab value would be affected by increased chest wall stiffness or expiratory muscle weakness?
|
High RV
|
|
|
Other causes of obstruction.
|
goiter, vocal cord paralysis, tracheal stenosis/tumors, foreign body
|
|
|
Other causes of restriction.
|
post polio syndrome, obesity, CHF, Cobb angle >100 degrees
|
|
|
What is a bronchodilator response? When is it significant?
|
Degree to which FEV1 improves w/inhaled bronchodilator.
Documents reversible airflow obstruction. Significant if FEV1 increases by 12%. |
|
|
Emphysema vs Chronic Bronchitis:
PFT values |
Emphysema:
-FEV1/FVC <70% -TLC inc'd -Inc'd compliance -DLCO dec'd Chronic Bronchitis: -FEV1/FVC <70% -TLC normall -Normal compliance -DLCO normal |
|
|
If suspicious of an obstructive process, but PFTs are normal, what is your next step?
|
bronchoprovocation--methacholine or histamine inhaled in increasing concentrations, test stopped until FEV1 drops by >20% or max concentration inhaled.
r/o asthma is negative |
|
|
Parenchymal vs Chest Wall Restriction:
PFT Values |
Parenchymal:
FEV1/FVC>80% TLC<80% DLCO decreased Chest Wall Restriction: FEV1/FVC>80%, TLC<80%, DLCO normal |
|
|
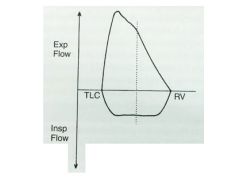
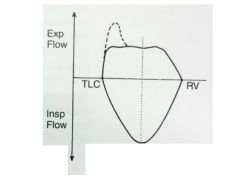
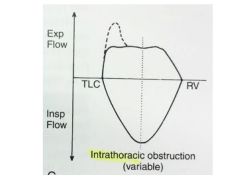
In this disease process category, flow rates at a given volume appear scooped-out or cove-like.
|
Obstructive lung disease
|
|
|
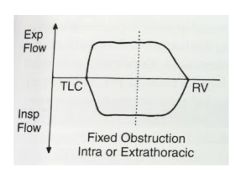
What defines a fixed obstructive lesion?
|
Irreversible lesion
Changes in pleural pressure do not affect degree of obstruction Limitation in peak airflow seen in both expiration/inspiration (plateau) |
|
|
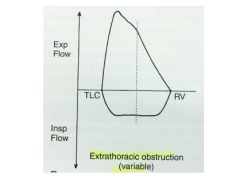
What defines a variable obstructive lesion?
|
Amount of obstruction determined by location of lesion and by alterations in pleural and airway pressure.
|
|
|
Cutoffs for Obstructive Pulmonary Disease Classification.
Mild Moderate Severe Very Severe |
Mild: FEV1: 80%
Mod: FEV1: 50-80% Sev: FEV1: 30-50% Very Severe: FEV1: <30% |
|
|
A PImax under ___% indicates ____ muscle weakness.
|
PImax under 60%-->inspiratory muscle weakness
|
|
|
A PEmax under ____% indicates ____ muscle weakness.
|
PEmax under 60%-->expiratory muscle weakness
|
|
|
Example of intrathoracic and extrathoracic obstruction.
|
Intrathoracic = within thorax, ex: lower tracheal tumor
Extrathoracic = outside of thorax, ex: vocal cord paralysis |
|
|
|
|
|
|
|
|
|

