![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
20 Cards in this Set
- Front
- Back
|
describe the differential diagnosis between red-flag back pain, disc prolapse, and non-specific low back pain |
low back pain - lumbosaccral, buttocks and thighs - usually self limiting and short lived - presentation 20-55 years
disc prolapse - unilateral leg pain worse than back pain, radiating to feet and toes - straight leg raise reproduces leg pain - numbness and parasthesia in area associated with effected nerve root - knee and ankle reflexes may be affected
red flag - presentation under 25 or onset over 50 - non-mechanical pain - thoracic pain - widespread neurological symptoms - unwell, weight loss - structural deformity - reduced anal tone - urinary retention - history of cancer, steroid use
|
|
|
what is cauda equina syndrome?
symptoms? |
a serious neurological condition in which damage to the nerve roots below the conus medullaris results in acute loss of function of the lumbar plexus
saddle anaesthesia reduced anal tone urinary retention erectile dysfunction |
|
|
tell me a little about where the spinal cord lives, who are the people in its barrio? |
it is located within the spinal column - created by the foramina of the stacked vertebrae
all three meninges cover the spinal cord and spinal nerves up until the point they leave via the intervertebral foramen
denticulate ligaments project from the pia mater to the inner surface of the dura mater, and suspend the spinal cord in the middle of its dural sheath
CSF in subarachnoid space
cushion of fat and connective tissue in epidural space (between dura matter and internal wall of vertebral canal
vertebral ligaments also provide support
|
|
|
describe the spinal cord, its shape and length and so on... |
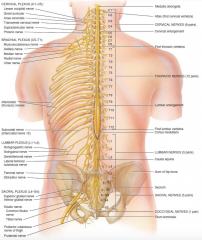
roughly oval in shape
in adults it extends from medulla oblongata to the superior border of L2 (infants to L3-L4)
cervical enlargement (C4-T1) lumbar enlargement (T9-T12)
spinal cord terminates as conus medullaris (L1-L2) arising from which in the filum terminale - an extension of the pia mater that fuses with the arachnoid and dura mater and actors the spinal cord to the coccyx
within the spinal cord there is no obvious segmentation but spinal nerves are named for the segment in which they are located
two bundles of axons (roots) connect each spinal nerve to the spinal cord via smaller bundles - rootlets
lumber, sacral and coccygeal nerves run along the filum terminale and exit the the spinal column lower than they exit the spinal cord - making up the cauda equina
|
|
|
draw and label a cross section of the spinal cord |
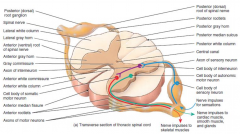
white matter - primarily myelinated axons
grey matter - dendrites and cell bodies of neurons, unmyelinated axons and neuroglia
central canal contains CSF and is continuous with the fourth ventricle in the medulla oblongata
|
|
|
what is contained in the different horns of the grey matter in the spinal cord? |
dorsal grey horn contains cell bodies and axons of interneurons as well as axons of incoming sensory neurons
ventral grey horns contain somatic motor nuclei fro contraction of skeletal muscle
lateral grey horns contain autonomic motor nuclei - clusters of cell bodies regulating the activity of cardiac and smooth muscle and glands |
|
|
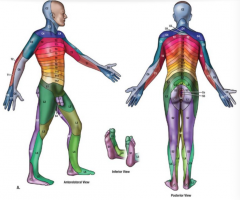
dermatome map |
|
|
|
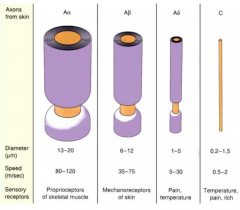
classification of nerve fibres table |
|
|
|
myotomes |
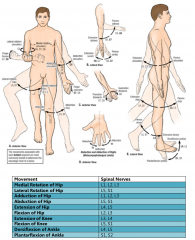
|
|
|
describe the physiological effects of low back pain |
- mostly non specific - no identifiable, specific spinal pathology
- pain usually varies with time and physical activity
- often referred to mid buttocks and thigh
- morning stiffness/pain is common
- pain may be aggravated by certain positions, activity or inactivity
- pain probably due to physiological dysfunction
|
|
|
define pain |
pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage |
|
|
tell me a wee bit about nociceptor fibres |
nociceptors are free nerve endings, whose cell bodies are located in DRG (body and trigeminal ganglia (face)
they are activated hen the stimulus reaches noxious threshold and respond progressively to the intensity of the stimulus, continuous stimulation can decrease the threshold
pricking pain - Aδ fibres - well localised, rapidly appreciated, often transient, sensation is tolerable, important in reflex
burning pain - C fibres - difficult to localise, can transmit intolerable pain, often provokes ANS response
nociceptors use the following neurotransmitters (produced tin the cell bodies in DRG) - glutamate - substance P - calcitonin G-related peptide (CGRP)
they are activated by - thermal activation - mechanical activation - chemical activation |
|
|
what happens with tissue injury? |
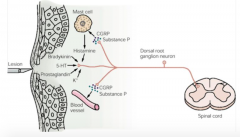
tissue injury causes release of - bradykinin - serotonin - PGs - K+ which stimulate C fibres, which release - CGRP - substance P which stimulate mast cells to release histamine and cause dilation of blood vessels, also causing plasma extravasation, oedema and further release of bradykinin - a sort of positive feedback
- the above processes lower the activation threshold of nociceptors leading to hyperalgesia and allodynia
|
|
|
what's hyperalgesia and allodynia? |
hyperalgesia is the heightening of a normal pain response
allodynia is when a normally non-painful stimulus is perceived as painful
|
|
|
describe the CNS pathway of pain perception |
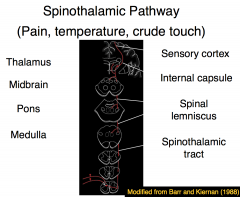
from local site, via DRG, to synapse with second order neurone in dorsal horn of grey matter
axon joins the spinothalamic tract in the anterolateral funiculus (pain, temp, crude touch), via the spinal lemniscus and internal capsule to synapse with third order neuron in the thalamus
third order nucleus then to the sensory cortex which elicits the sensation of pain |
|
|
explain the gate control theory |
- APs along C fibres excite projection neurones and inhibit inhibitory neurons (that normally tonically inhibit projection neurons)
- rubbing the skin, or electrical stimulation of peripheral nerves sets up APs in larger diameter Aα or Aβ fibres
- the inflow of these fibres activate inhibitory interneurons thereby suppressing transmission of activity in the C fibres
(these larger fibres can also illicit a pain response via stimulation of pain fibres in the spinal cord - wee bit complicated but it explains the positive arm towards the projection neuron in the below diagram) |
|
|
explain the descending modulation of nociceptive input |
- seretogenic and noradrogenic projections descend from the periaqueductal grey area of the pons and the raphe of the medulla
activity in nociceptor circuits is reduced by - direct inhibition of projection neurones - activation of enkephalin-containing interneurons (enkephalin reduces the amplitude of the EPSPs set up at the synaptic terminals between the axons of nociceptive neurons and the projection neuron)describe |
|
|
describe the management of low back pain |
- assessment (not X-ray unless red flag) - consider psychosocial issues - NOT bed rest as treatment - stay as active as possible - manipulation, physiotherapy, rehab if necessary - analgesia |
|
|
role of
GP physiotherapist osteopath chiropractor hospital specialist
in management of back pain |
GP - diagnostic triage, referral, advice, information, encouragement and support to return to normal activity
physiotherapist - build up supporting muscles, passive modalities to assist in pain management, TENS, provide pain relief and help to return to normal activities
osteopath - a system of diagnosis and treatment based in the theory that many diseases are associated with MSK system - involves palpation, manipulation and massage
chiropractor - based on the theory that all disorders can be traced to incorrect alignment of bones with consequent malfunctioning of nerves and muscles throughout the body - involves manipulation, mainly of vertebrae
hospital specialist - further evaluates and manages the underlying problem causing the back pain |
|
|
factors that contribute to the development and maintenance of chronic pain and disability
prevention? |
red flags - risk factors for developing persistent chronic pain and long-term disability
yellow flags are psycho-social barriers to recovery, including * belief that pain is harmful and severely disabling* fear avoidance behaviours and reduced activity * sickness behaviours such as extended rest * social withdrawal * low mood, depression, anxiety, stress * dissatisfaction at work * financial problems * overprotective family, or lack or support * inappropriate expectation of treatment - expectation of passive treatment * analgesia * early detection of psychosocial barriers * advice and education * discharge patient - not reinforce sickness role |

