![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
26 Cards in this Set
- Front
- Back
|
What are the types of pain? |
Acute Due to trauma ornoxious stimuli and/or Due to injury,disease process or abnormal function of muscle and viscera Chronic May be due to nociception, but Psychological andbehavioural factors play a major role Cancer Pain |
|
|
What is the pain pathway? |
Three neuron Pathway: First neuron: site of injury - dorsalroot ganglion (cell body of 1st order neurons) –spinal cord. Fast myelinated for pulling away (A delta fibers) slow unmyelinated dull long lasting pain (C fibers) Second order: Spinal cord to thalamus (spinothalamic tract) Third Order: Thalamus to Somatosensory area oneand two in post central gyrus of parietal cortex |
|
|
what is the role of the following receptors:
|
|
|
|
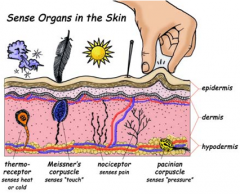
What are the types of nociceptors? What allogens can effect nociceptors? |
Most pain receptors (nociceptors) arefree nerve endings which sense heat, mechanical and chemical tissue damage. There are many types of these1.Mechanoreceptors:Respond to pinprick and pinch 2.Silent nociceptors: Respond only in presence of inflammation 3.Polymodal mechanoheat nociceptors : Mostprevalent and respond to excessive pressure, extremes of heat >42 <18 0C and Allogens or painproducing substances. Allogens include: bradykinin,histamine, serotonin, H, K and Prostaglandins etc. |
|
|
At which part of the three neuron pathway do the following medications work? NSAIDs Nerve block Opioids Epidural block Spinal block Paracetamol |
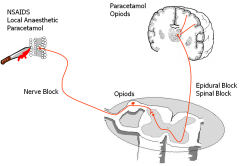
|
|
|
What are the transmitters of the spinal cord? |
Sensory events in spinal cord inputtingto brain.Transmitters are endogenous opiods, noradrenaline and 5HT Drugs which have an effect on thesetransmitters such as anti depressants (amitryptyline), clonidine (alpha2 agonist), opioids can help pain through central effects onthe brain but also by altering descending pathways to spinal cord Tramadol enhances inhibitorydescending pathways via its effects on NA (alpha-2) and 5HT |
|
|
Which of the following statements are correct:
|
|
|
|
What is the mechanism of paracetamol? What is it good at? poor at? How can it be administered? |
Inhibits prostaglandin production Central action – COX 3 Dose = 10-20mg/kg up to 1g Repeat 4 times a day (max 4g/day) Good opioid sparing effect if givenregularly Good antipyretic Poor anti-inflammatory IV/PO/PR |
|
|
What is the mechanism of NSAIDs? |
Cyclo-oxygenaseinhibitors Blocksprostaglandin and thromboxane production Prostaglandinspotentiate action of bradykinin & other polypeptides at pain receptors |
|
|
What is COX-1 and what NSAIDs inhibit it? What are the side effects? What is COX-2 and what NSAIDs inhibit it? |
COX1 constitutive isoenzyme responsible for homeostatic mechanisms(bronchial , renal , and gastric mucosa) e.g. Ibuprofen, diclofenac Sideeffects: Bronchospasm, GI effects, renal, platelets COX2 inducible form in response to inflammation e.g. parecoxib, celecoxib Selective COX 2 inhibitors with fewer side effects-cXPz |
|
|
What are the weak opioids? Strong opioids? |
Weak opioids Codeine, dihydrocodeine (weak) Tramadol Strong Opiods Morphine Oxycodone Fentanyl |
|
|
What is the mechanism of tramadol? |
mureceptor agonist Increasesinhibitory descending activity (5HT & noradrenaline) PO /IM / IV 50 – 100mg/ 4-6 hourly Notcontrolled drug Lowerincidence of some side effects |
|
|
What is the mechanism of strong opioids? What pain fibres are they effective against? |
IV opioids forsevere pain e.g. morphine, diamorphine, oxycodone StrongOP3 receptor agonists Canbe given po / im / transcutaneous/spinal / epidural PCAS(patient controlled analgesia system) Effectivefor C-fibre pain Lesseffective for Aδ-fibre pain |
|
|
What are the important side effects of morphine? |
Respiratory depression:Tidal Volume ↑, Respiratory Rate ↓: Overall MV ↓ Hypotension:Sympathetic tone ↓, vagal tone ↑, histamine release Euphoria, decreasedconscious level Constipation Tolerance anddependence |
|
|
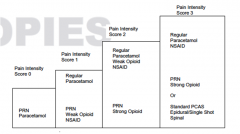
What is the analgesic ladder? |
|
|
|
40 year old man whohad repair of a 2 inch laceration on skin on forearm under local anaesthesia Where is he onanalgesic ladder? Pain Score : 0 What would youprescribe? |
Paracetamol 1gm 6 hourly PRN |
|
|
40 year old man whohad repair MUA of wrist for fracture radius under GA. Where is he onanalgesic ladder? Pain Score : 1 What would youprescribe? |
Paracetamol 1gm 6 hourly Regular Dihydrocodeine 30 mg 6 hourly PRN |
|
|
40 year old man whohad an emergency laparotomy for perforated diverticulum under GA Where is he onanalgesic ladder? Pain Score : 3 What would youprescribe? |
Paracetamol 1gm 6 hourly Regular Iburpofen 400 mg/ diclofenac 50 mg ▪8 hourly regular if tolerates MorphinePCAS/Epidural catheter |
|
|
40 year old man whohad open reduction and internal fixation of wrist for fracture radius under GA. Where is he onanalgesic ladder? Pain Score : 2 What would youprescribe? |
Paracetamol 1gm 6 hourly Regular Iburpofen 400 mg/ diclofenac 50 mg 8 hourly:Regular Dihydrocodeine 30 mg 6 hourly Morphine 10mg PO 2hourly PRN |
|
|
Mr G47 yr old3 days post emergencylaparotomy for perf diverticulumOtherwise doing wellbut still in a lot of pain What are you going to do?Why bother? |
72 hours postop ABCDE ok butuncomfortable Tolerating oralfluids Epidural workingpoorly You write up regular Paracetamol & NSAIDs Give the pain team acall Suggest removingepidural catheter and trial of oral dihydrocodeine Consider morphinePCAS if that fails |
|
|
What is chronic pain? What are the characteristics and give examples |
Persistent and intractablepain lasting more than 3 months Oftenneuropathic in origin 2characteristic types of pain Sharp,shooting Burning Examples Nerveroot compression, pancreatitis, ischaemic pain |
|
|
What is neural plasticity? Allodynia? |
Pain experienced beyond area of original injury (neural plasticity) Allodynia – light touch feels unpleasant |
|
|
What are the management strategies of chronic pain? |
Multidisciplinary Anaesthetist (coordinates) Pain nurses, psychologist,physiotherapist, pharmacist Patientmustunderstand there is no cure¡ Treatmentisaimed at symptom control & minimizing lifestyle restrictions |
|
|
What drugs are used fro chronic pain? |
Conventionalanalgesics Antidepressantse.g. amitriptyline Antiepileptics: Phenytoin, carbamazepine,sodium valproate Gabapentin Clonidine –alpha 2 agonist¡Ketamine Corticosteroids Capsaicin: C fibres, depletes substance P |
|
|
What are the most common co-morbidities with pain? |
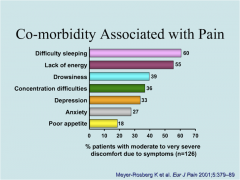
|
|
|
True or False about chronic pain:
|
|

