![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
124 Cards in this Set
- Front
- Back
|
An 18 yo with Fontan Circulation undergoing exploratory laparotomy. On ICU vent, sats 70%. Which ventilator parameter would you INCREASE to improve his sats?
A. Bilevel pressure B. Expiratory time C. Inspiratory time D. Peak inspiratory pressure E. PEEP |
B. Expiratory time
|
|
|
A 7 kg Infant with tetralogy of Fallot, post BT-shunt. Definitive repair at later date. Paralysed and vetilated. sats 85% baseline, now 70%, best treatment:
A. Increase FiO2 from 50 - 100% B. Esmolol 70 mcg C. Phenylephrine 35 mcg D. Morphine 1 mg E. 1/2 NS with 2.5% dex 70 mls |
C. Phenylephrine 35 mcg
Increase systematic resistance to reverse right to left shunt. |
|
|
Von Hippel-Lindau disease is associated with:
A. increased risk of malignant hyperthermia B. meningiomas C. peripheral neuropathy D. pheochromocytomas E. poor dentition |
D. pheochromocytomas
"Management of anesthesia in patients with von Hippel-Lindau disease must consider the possible presence of pheochromocytomas" (Stoelting) |
|
|
70 year old post TKJR. On sub-cut heparin. Develops clinical DVT and platelets 40. Management
A. Enoxaparin B. Fondaparinux C. Heparin by infusion D. Lepirudin E. Warfarin |
D. Lepirudin
(use a direct thrombin inhibitor) |
|
|
Hypercalcaemia:
A. Chvostek's sign B. C. D. E. Short QT |
E. Short QT
|
|
|
Drug eluting stent 6 months old. On aspirin and prasugrel 10mg. Elective lap cholecystectomy for biliary colic.
A. Do case while taking both. B. Do case while stopping both. C. Stop Prasugrel for 7 days, keep taking aspirin. D. Stop Prasugrel for some other different time E. Postpone for 6 months |
E. Postpone for 6 months
|
|
|
For a person newly diagnosed as MH susceptible, which is true?
A. ? B. Can have had an uneventful 'triggering' anaesthetic C. Recommended to use an anaesthetic machine which has not had volatiles through it D. ? E. There have been case reports of MH occurring up to 48 h post op |
B. Can have had an uneventful 'triggering' anaesthetic
CAECCP Malignant Hyperthermia On average, patients found to be susceptible to MH have had three previous uneventful general anaesthetics. |
|
|
ABG pH 7.12, PO2 100, PCO2 65, HCO3 20.3, BE -10. Consistent with?
A. Chronic renal failure B. Malignant hyperthermia C. Diabetic ketoacidosis D. End-stage respiratory failure E. Ethylene glycol toxicity |
B. Malignant hyperthermia
|
|
|
Cocaine overdose. What is false? (rpt Q)
A. Euphoria B. ? C. ? D. ? E. Miosis |
E. Miosis
A. true E. Cocaine is a stimulant causing mydriasis (dilatation) |
|
|
Maximum dose (with low risk of toxicity) of lignocaine (with adrenaline 1:100000) for liposuction with tumescence technique
A. 3 mg/kg B. 7 mg/kg C. 15 mg/kg D. 25 mg/kg E. 35 mg/kg |
E. 35 mg/kg
|
|
|
Compared to lignocaine, bupivacaine is
A. Twice as potent B. Three times as potent C. Four times as potent D. Five times as potent E. Same potency |
C. Four times as potent
http://www.icuadelaide.com.au/files/primary/pharmacology/local_anaesthetics.pdf |
|
|
Patient having aneurysm surgery, running on Propofol / remifentanil / NMDR. Depth of anaesthesia monitoring (Entropy). MAP 70 , HR 70/min, State entropy 50, Response entropy 70. What do you do?
A. B. Metaraminol C. Check TOF D. Nothing E. Increase TCI |
C. Check TOF
SE is depth of anaesthesia RE measures the temporalis muscle activity. This suggest paralysis is wearing off |
|
|
Paralysed with atracurium. TOF is 1(25%). You give a dose of 0.1 mg/kg mivacurium to close the abdomen. When will you be back to TOF 1(25%)?
A. 5 min B. 10 min C. 30 min D. 60 min E. 90 min |
?B. 10 min
Clinical duration is ~15 min Miller 7th ed p 877 |
|
|
Plenum Vaporiser
A.? something with fresh gas flows B. Relies on a constant flow of pressurised gas C. Out of circle D. Not temperature compensated E. volatile injected into fresh gas flow? |
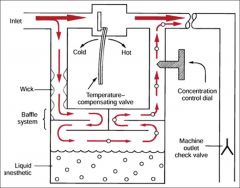
B. Relies on a constant flow of pressurised gas B. Upstream gas source required to push fresh gas through the vapouriser (opposite to draw-over) CEACCP 2011 Understanding vaporizers: Plenum vaporizers are high resistance, unidirectional, agent-specific, variable bypass vaporizers designed to be used outside the breathing system. |
|
|
Interscalene block, patient hiccups...where do you redirect your needle?
A. Anterior B. Posterior C. Caudal D. Cranial E. Superficial |
B. Posterior
Too anterior = phrenic nerve |
|
|
What is the SVR in a patient with MAP 100mmHg, CVP 5, PCWP 15, CO 5L/min?
A. ?0.8 B. ?3 C. 520 D. 1280 E. 1520 dynes.sec/cm-5 |
E. 1520 dynes.sec/cm-5
(80 to convert units) |
|
|
Accidentally cannulate carotid artery with 5 lumen 7 Fr CVC preop for a semi urgent CABG. Most appropriate next response is to
A. Get vascular surgeon to repair it and continue with surgery and heparin B. Leave it in. Do CABG. Pull it out post op. C. Pull it out, compress. Delay surgery for 24hrs D. Pull it out compress. Continue with surgery + heparin. E. Pull it out. Compress. Continue with surgery no heparin |
A. Get vascular surgeon to repair it and continue with surgery and heparin
or B?? Need to continue with urgent CABG. Need heparin. Compression unlikely to stop bleeding once fully heparinised. |
|
|
Stellate ganglion
A. Anterior to scalenus anterior B. ? C. ? D. ? E. ? |
A. Anterior to scalenus anterior
|
|
|
The median nerve
A. can be blocked at the elbow immediately medial to the brachial artery B. can be blocked at the wrist between palmaris longus and flexor carpi ulnaris C. can be blocked at the wrist medial to flexor carpi ulnaris D. is formed from the lateral, medial, and posterior cords of the brachial plexus E. provides sensation to the ulna half of the palm |
A. can be blocked at the elbow immediately medial to the brachial artery
B. No, between PL and FC radialis C. No, this is ulnar D. Only lateral and medial cords E. Radial half |
|
|
Patient for total knee replacement under spinal anaesthetic. Continous femoral nerve catheter put in for post op pain relief. Good analgesia and range of motion 18hrs post op. 24hrs post op, patchy decreased sensation in leg and unable flex knee. What is the cause?
A. Compression neurapraxia due to tourniquet B. DVT C. Muscle ischaemia D. Damage to femoral nerve E. Spinal cord damage |
A. Compression neuropraxia
|
|
|
A 75yo male with moderate aortic stenosis (valve area 1.1cm2). Gets mild dyspnoea on exertion but otherwise asymptomatic. needs hip replacement.
A. Continue with surgery B. Beta block then continue C. Get myocardial perfusion scan D. Postpone surgery awaiting AVR E. Postpone surgery awaiting balloon valvotomy |
?C. Get myocardial perfusion scan
NYHA class II. Hip replacement is intermediate risk surgery. He is symptomatic (mildly) so depends on other cardiac risk factors?? OHA: - symptomatic patients for elective non-cardiac surgery should have AVR first - asymptomatic for major elective surgery with major fluid shifts with gradients > 50mmHg should have AVR considered prior to surgery - asymptomatic for int/minor surgery do well if managed carefully |
|
|
Patient for fempop angioplasty, history of CCF. Also has diabetes on oral hypoglycaemics, controlled hypertension and atrial fibrillation at rate of 80bpm .
A. Medium risk surgery, medium risk patient B. Medium risk surgery, high risk patient C. High risk surgery low risk patient D. High risk surgery, medium risk patient E. High risk surgery, high risk patient. |
D. High risk surgery, medium risk patient
AHA |
|
|
23. Best Approach for a Sub-Tenon's block?
A. inferonasal b. inferotemporal c. medial canthus d. superior nasal e. superior temporal |
A. inferonasal
|
|
|
Baby with TracheoOesophageal Fistula found by bubbling saliva and nasogastric tube coiling on xray. Best immediate management?
A. Bag and mask ventilate B. Intubate and ventilate C. position head up, insert suction catheter in oesophagus (or to stomach?) D. Place prone, head down to allow contents to drain E. Insert gastrostomy |
C. position head up, insert suction catheter in oesophagus (or to stomach?)
|
|
|
A 60yo Man with anterior mediastinal mass, during induction for mediastinoscopy....lose cardiac output, decreased saturations, drop in ETCO2. Management
A. Adrenaline B. CPR C. CPB D. Place prone |
D
Ans D Management of the patient with a large anterior mediastinal mass: recurring myths Curr Opin Anaesthesiol 20:1-3 2007 Should try wake up the patient. D. Place prone Intraoperative life-threatening airway compression has usually responded to one of two therapies: |
|
|
Post thyroidectomy patient, patient in PACU for 30 minutes. Develops respiratory distress. Most likely cause?
A. Hypercalcemia from taking parathyroids B. Bilateral laryngeal nerve palsies C. bleeding and haematoma D. Tracheomalacia E. |
C. bleeding and haematoma |
|
|
27. Best way to prevent hypothermia in patient undergoing a general anaesthetic
A. Prewarming of patient B. C. D. Warm IV fluids |
A. Prewarming of patient
|
|
|
MAIN indication for biventricular pacing is
A. complete heart block B. congestive cardiac failure C. VF D. |
B. Congestive cardiac failure
|
|
|
Desflurane TEC6 vaporiser, unable to turn dial on. This is NOT because
A. vapouriser is tilted B. Hotter than 39C C. On battery power D. Interlock not engaged, or not seated properly E. other vapouriser is already on |
B. Hotter than 39C
TEC 6 will not work: - on battery power - if tilted >10 degrees - if interlock not engaged - if another vapouriser is on
|
|
|
Desflurane vaporiser, heated because of
A. High SVP B. High boiling poing C. Low SVP D. High MAC E. Low MAC |
A. High SVP
|
|
|
Myotome of C6-7 (Repeat Question)
A. Wrist flexion and extension B. Finger flexion and extension C. Elbow D. Shoulder E. |
A. Wrist flexion and extension
|
|
|
Most common cause of maternal cardiac arrest
A. PE B. AFE C. Haemorrhage D. Preeclampsia E. cardiomyopathy |
A. PE
|
|
|
Most likely change on CTG with anaesthesia for non-obstetric surgery at 32 wks
A. Loss of beat to beat variability B. No change C. Late decels D. Variable Deccels E. uterine contractions |
A. Loss of beat to beat variability
Evidence based practice of anaesthesiology (Fleischer)under conditions of very light sedation most narcotics and general anaesthetics decrease or obliterate long and short term FHR variability , hence one is left monitoring changes in baseline FHR. |
|
|
What is NOT associated with ulcerative colitis?
A. Cirrhosis B. Psoriasis C. Arthritis D. E. |
A. Cirrhosis
Harrison's: Psoriasis affects 5–10% of patients with IBD; may get PSC leading to biliary cirrhosis Ulcerative colitis may cause long-term problems such as arthritis, inflammation of the eye, liver disease (fatty liver, hepatitis, cirrhosis, and primary sclerosing cholangitis), osteoporosis, skin rashes, anaemia and kidney stones. |
|
|
What's the most appropriate mode for neuromuscular monitoring during aneurysm clipping?
A. TOFC B. TOFratio C. Post tetanic count |
C. Post tetanic count
|
|
|
What's the area burnt in man? Half of left upper arm, all of left leg and anterior abdomen
A. 27% B. 32% C. 42% D. E. |
A. 27%
Based on the 'rule of nines', the estimated burn surface area would be as follows: |
|
|
Torsades, what's not useful?
A. Amiodarone B. Isoprenaline C. Magnesium D. ? E. ? |
A. Amiodarone
|
|
|
Treatment for long QTc (OR what does NOT increase the QT interval)
A. Magnesium B. ? C. ? D. ? |
A. Magnesium
|
|
|
39. HOCM, VF arrest on induction, what's the first priority in management?
A. defibrillate B. amiodarone C. Intubate and ventilate D. Pre-cordial thump E. adrenaline |
A. defibrillate
|
|
|
40. Pregnant woman presents with narrow complex tachycardia HR 190, stable BP 100/60. No response to vagal manoevures. Management?
A. adenosine 6mg B. DCR C. amiodarone D. Atenolol E. ? |
A. adenosine 6mg
|
|
|
The intercostobrachial nerve:
A. Arises from T2 trunk B. Is usually blocked in brachial plexus block C. Supplies antecubital fossa D. can be damaged by torniquet E. Arises from inferior trunk |
D. can be damaged by torniquet
"tickle nerve" supplies axilla and originates from 2nd intercostal nerve |
|
|
42. Post dural puincture headache (PDPH) -(thoracic epidural) of "low pressure type". Features NOT consistent
A. Headache immediately after procedure B. Frontal headache only C. Starts 24hrs post D. Auditory symptoms E. Neck stiffness |
A. Headache immediately after procedure
|
|
|
Labour epidurals increase maternal and foetal temperature. This results in neonatal
A. Increased sepsis B. Increased investigations for sepsis C. increased non shivering thermogenesis D. Increased need for resuscitation E. Cerebral palsy |
B. Increased investigations for sepsis
|
|
|
Maternal cardiac arrest. In making the diagnosis of amniotic fluid embolism, large amount of PMNs surrounding foetal squamous cells are
A. Pathonomonic B. Supportive C. Only found at postmortem D. Irrelevant E. Incidental |
B. Supportive
|
|
|
Jehovah's witness patient refusing blood products. The ethical principle you are honouring if you continue with elective hip operation
A. Autonomy B. Non-maleficience C. Justice D. Paternalism |
A. Autonomy
|
|
|
An 86yo with severe dementia and multiple medical problems. Surgeons want to operate for faecal peritonitis/bowel perforation, and believe he will die without the surgery. Your decision NOT proceed with surgery is supported by which ethical principle?
A. Dignity B. Competence C. Non-maleficience D. Paternalism E. Futility |
C. Non-maleficience
(Futility is not an ethical principle?) Bioethical principles: autonomy, beneficence, non-malificence, and justice |
|
|
47. Inserted DLT. FOB down tracheal lumen. What feature is most helpful in identifying Left vs Right main bronchus
A. Trachealis muscle B. "there are 3 lobes in right lung" C. LMB longer than right D. Angle of RMB vs left E. Three segments of RUL |
A. Trachealis If down tracheal lumen, trachealis muscle is seen posterior so L and R are easy to identify. If down bronchial lumen, can look for RUL trifurcation and know that in R main bronchus |
|
|
48. You are performing a bronchoscopy, but are unsure of your location. Then you see trifurcation of bronchi. Most likely location is:
A. Right upper lobe B. Right Middle Lobe C. Right lower lobe D. Left lower lobe E. Lingula |
A. Right upper lobe
|
|
|
Elimination Half life of tirofiban
A. 2hrs B. 8hrs C. 12hrs D. 24hrs E. 15 minutes |
A. 2hrs
|
|
|
50. POISE trial showed
A. Increase CVA B. Anaphylaxis C. renal failure D. Increased AMI |
A. Increase CVA
POISE trial = perioperative use of beta blockers |
|
|
51. Why is codeine not used in paeds
A. Poor taste B. High inter-individual pharmacokinetic variability C. Not licensed for <10yo D. not as effective as adult when given in ?weight adjusted dose? |
B. High inter-individual pharmacokinetic variability
Variations in CYP2D6 function affect how much codeine is converted to morphine, and therefore how effective it is, but also how "sensitive" patients are to codeine. |
|
|
52. Patient on table for phaeochromocytoma with GA and epidural insitu. Pt on phenoxybenzamine and metoprolol preop, high dose nitroprusside and phentolamine. BP still high ?250/-. Next step
A. IV hydralazine B. IV Magnesium C. Propofol D. Epidural lignocaine bolus E. Esmolol |
B. IV Magnesium
Phenoxybenzamine is an irreversible, non-selective alpha blocker and can result in tachycardia due to a2 blockade. A beta-blocker is then used to prevent tachycardia. Options for intraop HD control: - phentolamine - SNP - GTN - Mg sulphate - increase volatile - CCB - beta-blocker (esmolol, labetalol) - antiarrhythmics (lidocaine, amiodarone) |
|
|
53. 25 yo primip 38/40 gestation with beta thalassemia trait for epidural. BP 140/95, mild proteinuria. Best test before you will put in epidural
A. Coagulation screen B. Hb C. Platelet count D. skin bleeding time E. |
C. Platelet count
Thalassemia trait - incorrect synthesis of Hb causing anaemia - is a red herring. No effect on clotting/epidural placement. Need to rule out thrombocytopaenia with pre-eclampsia. |
|
|
54. Pregnant lady 39/40 with BP185/115 , 4+proteinuria, clonus. IDC placed, 10mLs of dark coloured urine only for the last few hours. Initial management
A. 500mL Crystalloid bolus B. IV hydralazine C. IV Magnesium D. insert epidural |
B. IV hydralazine
Severe pre-eclampsia needs urgent BP lowering, some IV fluids (~200-250ml) need to be given, then clonus needs IV magnesium to prevent seizures. IV fluids need to match output (with careful IV fluid challenge) to prevent pulmonary oedema. Epidural only once platelet count established. Oliguria should be treated with careful IV fluid challenge. The BJA CEACCP article (see below) states that a bolus of 250ml crystalloid should be given, but if no improvement (in urine output) a CVC should be inserted before any further fluid given. Then be guided by CVP and urine output. |
|
|
The BEST agent to decrease gastric volume AND increase gastric pH before semi-urgent procedure
A. Omeprazole B. Cimetidine C. Ranitidine D. Sodium citrate E. ? |
C. Ranitidine
|
|
|
56. Most common congenital heart disease (repeat)
A. VSD B. PDA C. ASD D. TOF E. Transposition great arteries |
A. VSD
ACYANOTIC defects: VSD=35% ASD=9% PDA=8% Pulm. stenosis=8% Aortic stenosis=6% Coarctation=6% Atrioventricular septal defect=3% CYANOTIC defects: Tetralogy=5% Transposition=4% Ref: Stoelting's Anesthesia & Co-Existing Disease - 5th edn; p.44 |
|
|
57. Well and active 4 year old having tonsils and adenoids out. The patient has a continuous murmur, disappears on lying down. Most likely to be:
A. Venous hum B. PDA C. VSD |
A. Venous hum
|
|
|
Acetylcholine receptors are down regulated in
A. Guillain-Barre syndrome B. Organophosphate poisoning C. Spinal cord injury D. Stroke E. Prolonged NMBD use |
B. Organophosphate poisoning
A - Effectively a denervation injury which causes UP-regulation. B - Organophosphate poisoning causes increases in miniature-end-plate potential (MEPP), and thus can cause DOWN-regulation of ACh receptors. Apparently continuous exposure to organophosphates can cause degeneration of pre-junctional and post-junctional structures. C - Denervation causes UP-regulation. D - Denervation causes UP-regulation. E - Prolonged NMBD use can cause UP-regulation of ACh receptors. REFS: Miller (7th edn) - p.358 |
|
|
58. Myaesthenia gravis - all options are features predicting need for post op ventilation EXCEPT
A. Prolonged disease B. High dose Rx C. Previous respiratory crisis D. Increased sensitivity to NMBDs E. bulbar dysfunction |
D. Increased sensitivity to NMBDs
CEPD risk factors for IPPV postop (thymectomy) are: 1/ FVC<2.9L 2/ Concommitant COAD 3/ Acute fulminant crisis or respiratory involvement (grade 3) 4/ Myaesthenic crisis (grade 4) OHA adds: 5/ Duration of disease >6yrs 6/ Pyridostigmine dose >750mg/d 7/ Major body cavity surgery 8/ Bulbar palsy that is predictive of intra and postop airway protection.
Reference: CEPD Reviews 2002 p88- and OHA 246- |
|
|
59. Diagnositic utility of BNP best in:
A. SOB post pneumonectomy B. Confusion post CABG |
?A. SOB post pneumonectomy
BNP used to distringuish between respiratory and cardiac causes of dyspnoea. B-type natriuretic peptide (BNP) can effectively identify congestive heart failure in the emergency room setting but, despite increasing use, its diagnostic utility has not been validated in the intensive care unit (ICU). |
|
|
60. Innervation of larynx
A. internal branch of superior laryngeal nerve B. external branch of superior laryngeal nerve C. D. E. Cuff compression of recurrent laryngeal nerve against thryoid can cause palsy |
E. Cuff compression of recurrent laryngeal nerve against thryoid can cause palsy External branch SLN: cricothyroid muscle (tenses vocal cords for phonation) RLN: motor to all other muscles of larynx and sensory to below glottis NB. Posterior cricoarytenoid muscles abduct vocal cords to allow respiration. |
|
|
61.Which is not a branch of the mandibular nerve
A. Auriculotemporal B. Great auricular C. Lingual D. Masseteric E. Buccal |
B. Great auricular
Branches of mandibular nerve: a. from main trunk (before the division): - efferent nerves for the medial pterygoid, tensor tympani, and tensor veli palatini muscles - meningeal branch (a sensory nerve) b. from the anterior division - masseteric nerve(motor) - deep temporal nerves, anterior and posterior (motor) - buccal nerve (sensory) - lateral pterygoid nerve (motor) c. from the posterior division - auriculotemporal nerve (sensory) - lingual nerve (sensory) - inferior alveolar nerve
|
|
|
62. Reason not to operate liver injury
A. Haemodynamically stable B. Low grade injury on CT C. ? |
Haemodynamically stable
|
|
|
64. Most distant anatomy seen on grade III laryngoscopy
A. soft palate B. hard palate C. epiglottis D. arytenoid cartillage E. opening to larynx? |
C. epiglottis
|
|
|
65. Trauma pt, Head Injury with GCS 5, high ICPs, best management for ortho procedure
A. Propofol/fentanyl B. Propofol / nitrous C. Other options with volatiles |
A. Propofol/fentanyl
|
|
|
66. Person with acute intermittent porphyria given ?something and triggered a seizure, what not to use
A. Morphine B. Phenytoin |
No correct answer.
(Morphine is safe but no use for a seizure) Drugs considered safe to use in convulsing porphyriacs include: midazolam, diazepam, propofol, gabapentin and magnesium.
|
|
|
67. Regarding anticholinesterases:
A. pyridostigmine has slow onset of effect B. physostigmine does not rely on renal metabolism/excretion C. neostigmine cannot reverse centrally acting cholinergics D. edrophonium is less reliable in reversal? |
C. neostigmine cannot reverse centrally acting cholinergics
|
|
|
68. question about multiple sclerosis
A. exacerbated with heat |
A. exacerbated with heat
|
|
|
69. Question about signs seen in sarin poisoning:
A. mm fasciculation B. dry skin |
A. mm fasciculation
Sarin organophosphate |
|
|
70. Nerve to block for painful meralgia parasthetica
A. lateral femoral cutaneous nerve B. femoral nerve |
A. lateral femoral cutaneous nerve
Meralgia paraesthetica: chronic neurological disorder involves a single nerve, namely the lateral cutaneous nerve of thigh. |
|
|
71. Paternal uncle has MH, pregnant lady, how best to test for MH?
A. muscle biopsy on pregnant lady B. negative muscle biopsy of her father C. genetic testing of pregnant lady |
B. negative muscle biopsy of her father
A. Not advised to test in pregnancy B. 1st order relative of proband, should test C. No use if father is negative |
|
|
72. The nerve supplying area of skin between greater trochanter and iliac crest:
A. subcostal nerve B. ilioinguinal nerve C. genitofemoral nerve D. femoral nerve E. lat cutaneous femoral nerve |
A. subcostal nerve
|
|
|
73. Hydroxyethylstarch with intermediate volume replacement/ duration(rpt):
A. 6% HES 130/0.4 |
Ans A
|
|
|
74. Pyloric stenosis
A. alkaline then acid urine B. ? C. ? |
A. alkaline then acidic urine
Initially aim to correct alkalosis. Then switches to preserving volume (activation of RAAS) and retention of Na in exchange for H+. |
|
|
75. Which can deliver minute ventilation of greater than 5L/min using a 14 G cannula used for needle cricothyroidotomy
A. jet ventilation using pressure 400kPa B. oxygen flush button on anaesthetic machine C. oxygen tubing on oxygen port on anaesthetic machine at 12L/min D. E. none of the above |
A. jet ventilation using pressure 400kPa
|
|
|
76. Congenital diaphragmatic hernia
A. "there is hyperplasia of pulmonary arterioles" B. |
A. "there is hyperplasia of pulmonary arterioles"
|
|
|
77. Young man in trauma, hypotensive ?BP70/40. CXR widened mediastinum. FAST strongly positive. Best way to assess the widened mediastinum is:
A. intraop TOE B. TTE |
A. intraop TOE
Transthoracic echocardiography (TTE) is easily available and the ascending aorta and aortic arch can be visualised well. In obese or chest trauma patients, image quality may be inadequate due to poor echo windows. Transoesophageal echocardiography (TOE) has become more popular as experience and availability increase. It is useful perioperatively in the haemodynamically unstable patient. TOE images the entire thoracic aorta except for the most distal ascending aorta and a part of the arch obscured by the trachea or right main bronchus. Echocardiography can be used with high accuracy for decision-making in acute dissection. |
|
|
78. IV paracetamol
A. late plasma levels around the same as oral B. highly protein bound C. ?30%? renally excreted D. VD 10L/kg |
A. late plasma levels around the same as oral
|
|
|
79. Head trauma patient with unilateral dilated pupil, what's the diagnosis ?
A.Global injury B.Optic nerve injury C.Horners syndrome D.Transtentorial herniation E..... |
D.Transtentorial herniation
|
|
|
80. Question about CO2 Laser. Does not cause deep tissue damage because
a. High Frequency b. Penumbra effect c. ? Dissipation of energy d e. |
c. ? Dissipation of energy
Characteristics of the CO2 laser and its uses: The radiant energy produced by the CO2 laser is strongly absorbed by pure, homogeneous water and by all biologic tissues high in water content. The extinction length of this wavelength is about 0.03mm in water and in soft tissue. |
|
|
81. Patient with diastolic dysfunction. Is it caused by:
a. Restrictive cardiomyopathy b. Dilated cardiomyopathy c. d. e. |
a. Restrictive cardiomyopathy
|
|
|
82. Supine hypotension syndrome (due to aortocaval compression):
a. High SVR b. Tachycardia |
A and B
Sharma S. Shock and Pregnancy. eMedicine.com. URL: http://www.emedicine.com/med/topic3285.htm |
|
|
83. Non-normally distributed pain scores. What is the best way to describe spread of data?
A. Inter-quartile range B. Standard deviation C. Standard error of the mean D. ? E. ? |
A. Inter-quartile range
|
|
|
84. What term means the number of people who are correctly identified as not having a disease:
A. Sensitivity B. Specificity C. Positive predictive value D. Negative predictive value |
B. Specificity
|
|
|
85.If a test is negative, what proportion will not have the disease:
A. Sensitivity B. Specificity C. Positive Predictive Value D. Negative Predictive Value |
D. Negative Predictive Value
|
|
|
86. Cryoprecipitate: insufficient (rpt)
A. F9 B. F13 |
A. F9
Cryoprecipitate is prepared from plasma and contains fibrinogen, von Willebrand factor, factor VIII, factor XIII and fibronectin. Cryoprecipitate is the only adequate fibrinogen concentrate available for intravenous use. |
|
|
Most likely to result in myocardial infarction (rpt):
A. intraop myocardial ischaemia B. post op myocardial ischaemia |
B. post op myocardial ischaemia
From Landesberg G: The Pathophysiology of peri-op MI: the facts and perspectives. J Cardiothoracic and Vac Anaes 2003: 17(1): 90-100 |
|
|
88. Awake patient with diabetes insipidus
A. Euvolaemic B. C. D. E. urinary Na <20 |
A. Euvolaemic
DI caused by insufficient vasopressin. |
|
|
Indication for percutaneous closure of ASD
a. Primun < 3cm b. Primun > 3cm c. Secundum < 3 cm d. Secundum > 3cm e. sinus venosus ASD |
c. Secundum < 3 cm
|
|
|
90. Timing of worst coagulopathy after liver transplant
a. 1-2 days b. 3-4 days c. 5-6 days |
a. 1-2 days ??
Oh manual: would do coag tds for first day |
|
|
91. ASA grading was introduced to
A. predict intraop anaesthetic risk B. Predict intraop surgical and anaesthetic risk C. Standardise the physical status classification of patients D. Predict periop anaesthetic risk E. Predict periop anaesthetic and surgical risk |
C. Standardise the physical status classification of patients
|
|
|
92. Pulsus paradoxus is: (the Q was something like - severe asthmatic - when take BP you would find)
A. Reduced BP on inspiration unlike normal (ie normally increased on insp) B. Reduced BP on inspiration exaggerated from normal C. Reduced BP on expiration unlike normal D. Reduced BP on expiration exaggerated from normal E. ? |
B. Reduced BP on inspiration exaggerated from normal
|
|
|
92. Respiratory function in quadriplegics is improved by
A. abdominal distension B. an increase in chest wall spasticity C. interscalene nerve block D. the upright position E. unilateral compliance reduction |
B. an increase in chest wall spasticity
|
|
|
93. An INCORRECT statement regarding the autonomic nervous system is that
A. autonomic dysfunction is a predictor for worse long term survival after myocardial infarction B. heart rate responses are primarily mediated through the sympathetic nervous system C. inhalation anaesthetics all impair autonomic reflex responses D. autonomic dysfunction is a predictor for haemodynamic instability following anaesthetic induction E. low heart rate variability is associated with worse cardiac outcomes following non-cardiac surgery |
B. heart rate responses are primarily mediated through the sympathetic nervous system
Heart rate is intrinsically 100bpm. This is then modified by the parasympathetic system |
|
|
94. Correct statements regarding expiratory-inspiratory flow-volume loops include all of the following EXCEPT
A. in obstructive disease the expiratory curve has a scooped out or concave appearance B. in restrictive disease expiratory flows are usually decreased in relation to lung volume C. in restrictive disease the expiratory curve has a convex appearance D. the expiratory curve is largely effort independent E. the inspiratory curve is effort dependent |
C. in restrictive disease the expiratory curve has a convex appearance
|
|
|
95. Carbon dioxide is the most common gas used for insufflation for laparoscopy because it
A. is cheap and readily available B. is slow to be absorbed from the peritoneum and thus safer C. is not as dangerous as some other gases if inadvertently given intravenously D. provides the best surgical conditions for vision and diathermy E. will not produce any problems with gas emboli as it dissolves rapidly in blood |
C. is not as dangerous as some other gases if inadvertently given intravenously
|
|
|
Following a cadaveric renal transplant under general anaesthesia, your patient's plasma K+ increases to 6.0 mmol/L in recovery after being 5.0 mmol/L pre and intra-operatively. This patient requires
A. an intravenous infusion of CaCl2 (10 mls over 20 minutes) B. arterial blood gases to ascertain the acid/base status C. potassium exchange resins rectally D. sodium bicarbonate infusion (50- 100 mEq over 5- 10 minutes) E. urgent haemodialysis |
B. arterial blood gases to ascertain the acid/base status
|
|
|
97. Carcinoid syndrome - finding on examining heart:
A. Fine inspiratory crepitations B. Systolic murmur at apex C. Systolic murmur at left sternal edge D. Murmur at apex with opening snap E. Pericardial rub |
C. Systolic murmur at left sternal edge
RHF associated with liver mets releasing factors (which are inactivated by the lungs so they don't affect left heart). They cause fibrosis of valves and can cause stenosis or regurgitation. |
|
|
98. Histamine release in anaphylaxis does NOT cause:
A. Tachycardia B. Myocardial depression C. Coronary artery vasodilatation D. Prolonged PR interval E. Decreased impulse conduction] |
B. Myocardial depression
H1 via PLC Coronary constriction Bronchoconstriction Slow AV node Release of prostacyclin H2 via cAMP Inotropy Coronary dilation Bronchodilation Tachyarrhythmia Increase PR Ventricular irritability Decrease VF threshold Shift in pacemaker rate CNS stimulation Increase H+ secretion by parietal cells Both H1&2 increase capillary leakage |
|
|
99. Pre-ganglionic sympathetic fibres pass to the
A. otic ganglion B. carotid body C. ciliary ganglion D. coeliac ganglion E. all of the above |
D. coeliac ganglion
|
|
|
100. Branches of the mandibular nerve do NOT include the
A. auriculotemporal nerve B. long buccal nerve C. lingual nerve D. great auricular nerve E. chorda tympani nerve |
D. great auricular nerve, AND
E. chorda tympani nerve
|
|
|
101. In a trial, 75 patients with an uncommon, newly described complication and 50 matched patients without this complication are selected for comparison of their exposure to a new drug. The results show:
Complication present absent Exposed to new drug 50 25 |

A. the relative risk of this complication with drug exposure CANNOT be determined
This is a case-control study.
Odds of disease in exposed = 50/25 = 2 Odds of disease in non-exposed = 25/25 = 1 OR = Odds in exposed / odds in non = 2 |
|
|
102. BP measurement - overestimates with:
A. big (wide) cuff B. skinny arm C. severely peripherally vasoconstricted D. atherosclerosis E. slow cuff deflation |
D. atherosclerosis
|
|
|
103. A device that detects a 10mA difference in active and neutral leads and causes turning off of the circuit within 40 ms. this is a :
A. Class 1 device B. Equipotential earthing C. LIM D. Residual Current Device E. Fuse |
D. Residual Current Device
|
|
|
104. Post-transfusion hepatitis in Australia is associated with
A. jaundice in over 50% of patients B. development of chronic disease in less than 10% of patients C. hepatitis B in the majority of patients D. the presence of antigen or antibody to hepatitis C E. elevation of serum alkaline phosphatase |
C. hepatitis B in the majority of patients
|
|
|
105. In a patient requiring FFP where the patient’s blood group is unknown, it is ideal to give FFP of group
A. A B. B C. AB D. O E. Blood group of FFP in this situation does not matter |
C. AB
|
|
|
106. Features of the transurethral resection of the prostate (TURP) syndrome include all of the following EXCEPT
A. agitation B. angina C. bradycardia D. nausea E. tinnitus |
E. tinnitus
|
|
|
107. The most frequently reported clinical sign in malignant hyperpyrexia is
A. arrhythmia B. cyanosis C. sweating D. tachycardia E. rigidity |
D. tachycardia
|
|
|
Which of the following is not an absolute contra-indication for MRI?
A. cochlear implant B. heart valve prosthesis C. ICD D. pacemaker E. intracranial clips |
B. heart valve prosthesis
|
|
|
109. Reverse splitting of the second heart sound occurs with:
A. LBBB B. Pulmonary hypertension C. Acute pulmonary embolus D. ASD E. Severe MR |
A. LBBB
|
|
|
110. Atrial fibrillation:
A. Cardioversion results in longer life expectency than rate control B. Need to stay on warfarin following cardioversion C. Pt with HR <80 generally do not require anticoagulation D. |
B. Need to stay on warfarin following cardioversion
|
|
|
111. Scoliosis surgery. What is incorrect
A. one third of the blood loss occurs postoperatively B. major blood loss is frequently accompanied by a consumptive coagulopathy C. surgery will halt progression of the restrictive lung deficit D. the major neurological deficits that occur are usually due to damage to the posterior columns of the spinal cord E. the use of aprotinin reduces blood loss |
usually due to damage to the posterior columns of the spinal cord
(Anaesthesia for correction of scoliosis in children) |
|
|
112. About transient neurological syndrome:
A. Comprises pain localised to the back B. Diagnosis is confirmed by typical finding on neurological examination C. Associated with consistent abnormalities on magnetic resonance imaging and electrophysiological studies (EPS) D. associated with long term deficits in 5% of cases E. May occur with lignocaine, bupivacaine, prilocaine and procaine. |
E. May occur with lignocaine, bupivacaine, prilocaine and procaine.
|
|
|
113. Epidural infection...
Serious post operative epidural infection A. Is rarely due to staphylococcal species B. Is associated with epidural catheter disconnection C. Occurs with an incidence in the range of 1-2 per 10,000 D. Is usually reported in obstetric cases E. Mandates surgical drainage if an abscess is present |
C. Occurs with an incidence in the range of 1-2 per 10,000
A. The commonest microorganisms found in spinal infection are bacteria (90% cases), particularly Staphylococcus aureus. B. ?? C. OHA p1103 states risk of abscess 0.01-0.05% ie 1-5 in 10,000 D. Much lower rate in obstetric patients BJA Review article Epidural abscess 2006 E. CEACCP "Although there may be a place for conservative management with antibiotics alone in carefully selected patients without neurological signs, this would be unusual and require careful monitoring. " CEACCP Epidural drug delivery 2007 OHA p1103 http://bja.oxfordjournals.org/content/96/3/292.full.pdf |
|
|
Regarding epidural abscess which is wrong:
A. diagnosis is dependent on triad of back pain, fever and paralysis B. occurs at a rate of 1:1000-3000 C. Worse outcomes if advanced age D. Usually gram positive cocci E. Expectant management may be appropriate |
A. diagnosis is dependent on triad of back pain, fever and paralysis
B. Rate is 1-5:10,000 OHA p 1103 C. Probably correct as epidurals generally used for you,fit parturients, or older patients with comorbidities undergoing major surgery. A. False. Only 13% of patients with epidural abscess present with the classical triad of fever, back pain, and neurological change. Back pain is the initial symptom in 75% cases; therefore, one in four patients has no back pain. Fever occurs in only 66% of cases. C. BJA Review article on Epidural abscess 2006: "doubling of likelihood of poor outcome for each decade of age" http://bja.oxfordjournals.org/content/96/3/292.full.pdf D. Usually staph, then strep E. CEACCP "Although there may be a place for conservative management with antibiotics alone in carefully selected patients without neurological signs, this would be unusual and require careful monitoring. " http://bja.oxfordjournals.org/content/96/3/292.full.pdf CEACCP Epidural drug delivery 2007 |
|
|
114. Difference between cardiac protected and body protected area
A. Equipotential earthing B. isolation transformer C. line isolation monitor D. Max leakage current to patient limit 500 microamperes E. Residual current device |
A. Equipotential earthing
|
|
|
115. Which hormone is not released during surgery?
A. Cortisol B. Glucagon C. TSH D. Growth hormone E. Catecholamines |
C. TSH
|
|
|
116. Asystolic aortic arch repair. The best method for cerebral protection is:
A. anterograde perfusion via coronary vessel B. retrograde perfusion via jugular vein C. thiopentone IV D. hypothermia to 20 degrees celcius |
D. hypothermia to 20 degrees celcius
though new treatment is combination of deep/intermediate hypothermic arrest plus ?anterograde perfusion |
|
|
117. Specificity most closely means
A. chance of a positive test in people with the disease B. chance of a negative test in people without disease C. chance of... |
B. chance of a negative test in people without disease
|
|
|
118. Negative predictive value most closely means
A. chance of a positive test in people with the disease B. chance of a negative test in people without disease C. chance of a person who tested negative truly not having the disease |
C. chance of a person who tested negative truly not having the disease
NPV = TN / (TN+TP) |
|
|
119. Performing a bronchoscopy. The best way to orient the scope is:
A. angle of the bronchus B. length of the bronchus c. RUL trifurcation |
c. RUL trifurcation |
|
|
121. Paediatric VF arrest. Which is true?
A. if resistant to defibrillation should give amiodarone 5mg/kg B. C. commonly associated with respiratory arrest D. is the most common form of arrest in this patient group E. should defibrillate with 5J/kg |
A. if resistant to defibrillation should give amiodarone 5mg/kg
ARC The most common arrest scenario in children is bradycardia proceeding to asystole (a response to severe hypoxia and acidosis.) |
|
|
Intercostobrachial nerve
A. Is often damaged by torniquet B. supplies sensation to cubital fossa C. is blocked by interscalene brachial plexus block D. ? E. ? |
A. Is often damaged by torniquet
|
|
|
123. OLV hypoxaemia. After 100% O2 and FOB next step is: (rpt)
A. CPAP 5cm top lung B. CPAP 10cm top lung C. PEEP 5cm bottom lung D. CPAP 5cm top + PEEP 5cm bottom |
C then A
C. Miller A. CEACCP |

