![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
48 Cards in this Set
- Front
- Back

Autorhythmic cell action potential
|

**There is no resting membrane potential
If "funny channels" open; permeable to Na+ and K+ • Na+ influx exceeds K+ efflux (= slow depolarization) Initial depolarization causes T-type (transient) Ca²+ channels to open Further depolarization causes L-type (long lasting) Ca²+ channels to open (= rapid depolarization) Depolarization causes K+ channels to open; K+ exits cell • Repolarization of cell to −60mV; K+ channels close |
|
|
Electrical Activity in a Pacemaker Cell
|

Orange: spontaneous depolarization
• K+ exiting; Na+ entering cell Yellow: later spontaneous depolarization • Ca+ entering Green: rapid depolarization • Ca²+ entering Pink: depolarization • K+ existing |
|
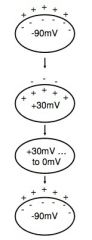
Contractile cell action potential
|
**Resting membrane potential (-90mV); depolarizes only when stimulated
• Stimulus opens voltage-gated Na+ channels • Rapid inflow of Na+ into cell • Action potential peak at +30mV • Na+ gates close quickly • Delayed opening of V-G Ca²+ channels • EC Ca²+ enters & binds to ligand-gated Ca²+ channels on sarcoplasmic reticulum • 2nd wave of Ca²+ binds to troponin → contraction • K+ channels open; K+ exits cell • Ca²+ channels close; Ca²+ transported back into SR • Repolarization |
|
|
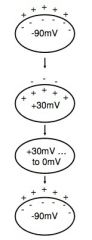
AP of Contractile Cell
|
0) V-G Na+ channels open (when stimulated)
1) Action potential peaks, slight depolarization, V-G sodium channels close 2) V-G channels Ca²+ open; EC Ca²+ enters & binds to ligand-gated channels on SR, 2nd Ca²+ wave → contraction 3) K+ channels open, K+ exits cell, Ca²+ channels close, Ca²+ returns to SR 4) Repolarization |
|
|
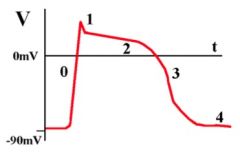
Electrical activity of heart is recorded by _____.
|
electrocardiogram (ECG)
|
|
|
P wave
|
corresponds to atrial depolarization
|
|
|
QRS complex
|
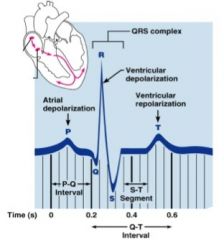
corresponds to ventricular depolarization
|
|
|
T wave
|
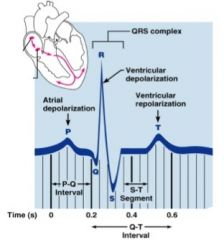
corresponds to ventricular repolarization
|
|
|
Atrial repolarization is masked by larger ________.
|
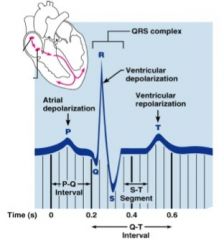
QRS complex
|
|
|
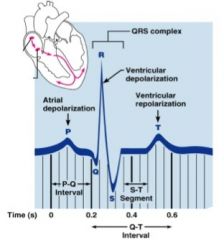
Heart Excitation Related to ECG
|
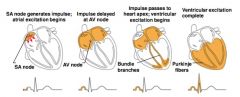
SA node generates impulse; atrial excitation begins
----- Impulse delayed at AV node ----- Impulse passes to heart apex; ventricular excitation begins ----- Ventricular excitation complete |
|
|
Cardiac Cycle
|
all the events associated with a single heartbeat (w/ respect to L Ventricle)
|
|
|
systole
|
contraction of heart muscle
|
|
|
diastole
|
relaxation of heart muscle
|
|
|
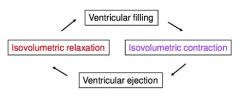
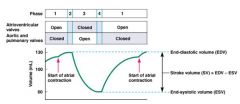
What are the four phases of the cardiac cycle?
|

1) ventricular filling (mid-late) diastole
2) isovolumetric contraction (beginning of systole) 3) ventricular ejection: (mid-late systole) 4) isovolumetric relaxation (beginning of diastole) |
|
|
What occurs during ventricular filling?
|
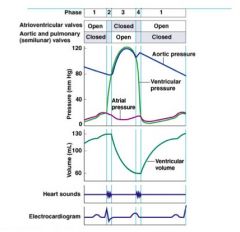
• low pressure in ventricles
• AV valves open • ventricles passively fill with blood At the end of phase one… • atria depolarize (P wave), then… • atria contract → remaining blood enters ventricles |
|
|
What occurs during isovolumetric contraction?
|
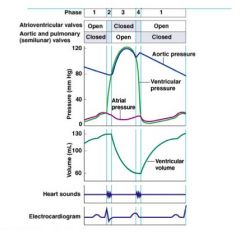
• ventricle depolarize (QRS)
• ventricles begin to contract ∙ ↑ ventricular pressure ∙ closes AV valves ("Lub" - 1st heart sound) • semilunar valves remain closed = isovolumetric Contraction (constant volume in ventricles) |
|
|
What occurs during ventricular ejection?
|
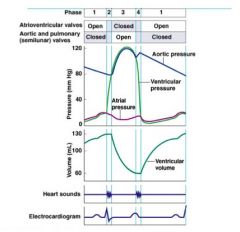
• ↑ ventricles to maximal pressure
∙ forces semilunar valves open • blood ejected into great vessels ∙ ↓ ventricular volume |
|
|
What occurs during isovolumetric relaxation?
|
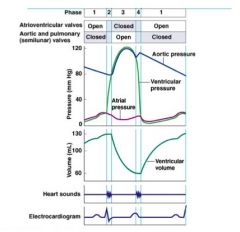
• low pressure in ventricles
• SL valves open ("Dup" - 2nd heart sound) • AV valves still closed ...until... 1) Ventricular filling • ventricular pressure drops below atrial pressure → forces AV valves open ∙ ventricular filling |
|
|
What is the Dicrotic notch?
|
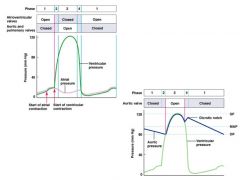
rise in the BP in aorta: blood encounters resistance and starts to flow back to ventricle
|
|
|
Blood moves from one place to another because of a _______
|
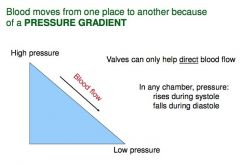
Pressure Gradient
|
|
|
isovolumetric contraction
|
all valves closed, ventricles contracting
volumes of ventricles remain constant & at HIGHEST End diastolic volume |
|
|
isovolumetric relaxation
|
all valves closed, ventricles relaxing
volumes of ventricles remain constant & at LOWEST End systolic volume |
|
|
End diastolic volume
|
amount of blood collected in a ventricle during diastole
|
|
|
End systolic volume
|
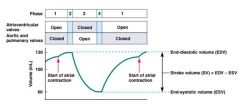
amount of blood collected in a ventricle during systole
|
|
|
Stoke Volume =
|
End diastolic volume - End systolic volume
SV = EDV - ESV |
|
|
Cardiac Output (CO)
|
volume of blood pumped by one ventricle in 1 minute (ml/min or L/min)
CO = HR x SV |
|
|
Heart Rate (HR)
|
heart beats/minute
CO = HR x SV |
|
|
Stroke Volume (SV)
|
amount of blood ejected per beat (ml/beat)
at rest 80ml/beat x 75 beats/min = 6000ml/min Therefore our entire blood supply is circulated in 1 minute |
|
|
CO is the total blow flow to ________ of the body
|
CO is the total blood flow to all tissues of the body (systemic circuit); increased demand for O₂ and nutrients must be met by increased CO
|
|
|
Basic heart rate is set by _____; ________ modifies it
|
Basic heart rate is set by intrinsic conduction system; extrinsic modifies it
|
|
|
Extrinsic control of the heart is controlled by:
|
endocrine system and nervous system
|
|
|
Endocrine system
|
influences heart rate & force of contraction via several hormones
e.g. epinephrine, acetylcholine & thyroxine |
|
|
Nervous System
|
influences heart rate and force primarily via cardiac centers of medulla oblongata
|
|
|
What are the two cardiac centers of the medulla oblongata?
|

Cardioacceleratory center and Cardioinhibitory center
|
|
|
Cardioacceleratory Center
|
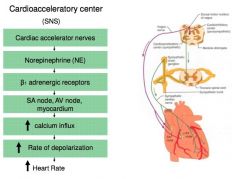
Sympathetic Nervous System (SNS)
Increases heart rate |
|
|
Cardioinhibitory Center
|
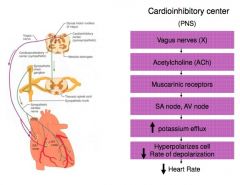
Parasympathetic Nervous System (PNS)
Decreases heart rate |
|
|
Under resting conditions the PNS and SNS sends signals to _______
|
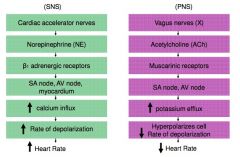
the heart
|
|
|
Given the following information:
• Both SNS and PNS sends signals to SA node • Without nervous system influence → SA node fires at 100 bpm • Resting heart rate = 70-80 bpm • If vagus nerves are severed → heart rate increases to 100 bpm What is the dominant influence of the resting heart rate? PNS? SNS? |
PNS is greater because heart rate is less than the natural, spontaneous depolarization of SA node → called Vagal Tone
|
|
|
What are the three main factors that influences stroke volume?
|
1) Preload
2) Contractility 3) Afterload |
|
|
What is Preload?
|
amount ventricles are stretched by contained blood
Preload - how much the ventricle is stretched before contracting ~ how much blood is in the ventricle before systole (EDV) ↑ EDV = ↑ Preload The more the ventricle is stretched - the more force it generates |
|
|
EDV (preload) is affected by:
|
1) Venous return - amount of blood returning to heart & filling ventricles
Note: an increase in CO = increase in VR 2) Filling time - duration of ventricular diastole Note: an increase in HR = decrease in filling time |
|
|
What is the Frank-Starling Law of the Heart
|
heart can pump any additional blood it receives per cardiac cycle (more in = more out)
↑ EDV = ↑ SV Preload (degree of stretch) is critical factor controlling SV |
|
|
What is contractility?
|
cardiac cell contractile force due to factors other than EDV
Contractility - how hard ventricles is squeezing, regardless of how it is stretched Directly proportional to Ca²+ levels within myocardial cell ↑ Contractility = ↑ SV and ↓ ESV Contractility increases when: • Cardioacceleratory activity increases • Plasma epinephrine levels increases • Plasma thyroxine levels increases Contractility decreases when: • Drugs such as calcium channels blockers increase |
|
|
Contractility increases when:
|
• Cardioacceleratory activity increases
• Plasma epinephrine levels increases • Plasma thyroxine levels increases |
|
|
Contractility decreases when:
|
• Drugs such as calcium channels blockers increase
|
|
|
What is afterload?
|
back pressure exerted by blood in large arteries leaving the heart
Afterload - refers to pressure that must be overcome by the ventricles in order for SL valves to open and blood to be ejected Any factor that increases resistance (and thus pressure) in the arterial circulation will increase after load Major problems with increase in after load results from chronic hypertension - heart attempt to compensate - leads to heart failure ↑ Afterload = ↓ SV Afterload increases with vasoconstriction (reduction in vessel diameter) Afterload decreases with vasodilation (increase in vessel diameter) |
|
|
What is the PR interval?
|
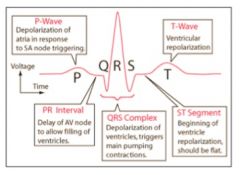
Delay of AV node to allow filling of ventricles
|
|
|
What is the ST Segment?
|
Beginning of ventricle to depolarization. Should be flat
|

