![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
239 Cards in this Set
- Front
- Back
|
What are the formed elements that make up blood? ***
|
- erythrocytes (RBCs) - which carry gases to/from cells from lungs
- leukocytes (WBC) - which assist with immune defense - platelets - (a.k.a. thrombocytes) - which are cell fragments which stimulate formation of clots--hemostasis (blood is a connective tissue consisting of these formed elements and proteins dissolved in a fluid matrix==cells, matrix, and fibers) |
|
|
What are the functions of blood? ***
|
- transport - gases, nutrients, hormones, wastes, cells
- ion regulation - transports ions around body; ensures proper ion concentrations in tissues (pH regulation) - prevention of fluid loss through injury - regulation of body temperature - carries heat to/from areas - protection - clotting, immune cells and proteins (transport, regulation X3, and protection) - blood is the primary nutrient distributor |
|
|
What are the four major plasma proteins and what are their functions? ***
|
1) albumin (produced by liver)
-- most abundant plasma protein (60%) -- maintains osmolarity of blood (concentration of solutes in solution) 2) globulins -- immunoglobulins (gammaglobulins) - involved in immune defense -- transport globulins - (alpha and beta globulins) - ----- hormone-binding proteins (e.g., TH and sex steroids) ----- metalloproteins - bind to metals (e.g., ferritin stores excess iron) ----- apolipoproteins - carry lipids as lipoproteins (VLDLs, LDLs, HDLs) 3) fibrinogen -- can be stimulated to form strands of fibrin which comprises the network of a blood clot 4) other proteins -- hormones, etc - plasma is 90% water and has a different makeup than interstitial fluid (more proteins and different ions) (composition of blood: - 47 - 63% plasma - or about 55% - 37 - 52% RBCs/hematocrit - <1% buffy coat - WBCs, and platelets) |
|
|
Approximately how much blood do males and females have? ***
|
- males - about 5-6 liters
- females - about 4-5 liters |
|
|
What is the hematocrit? ***
|
- the percentage of blood volume that is composed of erythrocytes
(his definition has, "the percentage of formed elements in blood, of which 99.9% are RBCs) - a.k.a. packed cell volume (RBCs comprise 1/3 of all human cells--the average human has 25 billion) |
|
|
What is approximate value in males and females?
(I'm assuming of the hematocrit?) *** |
- about 42% (book has 37-48%)
- about 47% (book has 45-52%) |
|
|
Why is it different in males and females? (I'm assuming we're still speaking of the hematocrit?)***
|
- androgens/testosterone contribute to EPO production, thus RBC production
- women of child-bearing age have cyclic menstrual losses - males have greater muscle mass, thus more metabolically active tissue requiring higher oxygen-carrying capacity (inversely proportionate to body fat levels) |
|
|
How is the hematocrit used to diagnose abnormal conditions? ***
|
can be used to diagnose:
- dehydration - high hematocrit, low plasma levels - anemia - low hematocrit/RBCs - polycythemia - excess RBCs |
|
|
What is the general structure of a erythrocyte? ***
|
- enucleate - nucleus ejected during development, thus no genes and unable to reproduce or repair themselves
- biconcave - for unknown purpose; may be: --- to increase surface area (thus oxygen-carrying capacity) without increasing volume --- to allow them to fit through small capillaries --- simply a result of the enucleation - discoid |
|
|
What is the general structure of the hemoglobin molecule? ***
|
- a protein contained within the RBC, approximately 280 million per cell
- 4 polypeptide chains + 4 heme units (heme = iron containing pigment) --- two alpha chains (141 amino acids long) --- two beta chains (146 amino acids long), occasionally 2 delta chains instead (2.5% of total same number of amino acids, but different sequence) - carries oxygen to cells as oxyhemoglobin - oxygen has weak binding affinity to heme group (weak because it needs to carry the oxygen, but also needs to give it up) - oxygen diffuses into tissues = deoxyhemoglobin - each heme can carry 1 molecule of oxygen (so maximum of 4 per hemoglobin molecule) --- hemoglobin molecules can vary in saturation however, by carrying only 1, 2, or 3 oxygen molecules (thus would be 25%, 50% or 75% saturated instead of 100%) |
|
|
How is fetal hemoglobin different than adult hemoglobin? ***
|
- has a higher oxygen-binding affinity (a "stronger magnet" if you will) in order to extract/keep oxygen from the mother's bloodstream
- has two gamma chains in place of the beta chains (same amino acid chain length, different sequence) |
|
|
What is the fate of hemoglobin after a red blood cell is broken down? ***
|
- RBC life-cycle is approximately 120 days
- 2.5 million cells per second are recycled - expired erythrocytes are broken up in the spleen ("erythrocyte graveyard") and liver via hemolysis (rupture of RBC) --- cell fragments are phagocytized by macrophages within the spleen/liver --- hemoglobin must be further broken down or it can block kidney tubules and cause renal failure - macrophages separate the heme from the globin --- then hydrolyze globulin into free amino acids and recycle for catabolism or protein synthesis - heme units undergo further breakdown --- macrophages remove the iron and release it into blood where it combines with transferrin and is used or stored same way as dietary iron (carried to marrow and some organs where it is bound to ferritin) --- macrophages then convert remainder of heme into biliverdin (greenish pigment) --- later broken down to bilirubin (yellowish pigment) --- bilirubin released by macrophages and binds to albumin in blood plasma --- liver removes it from albumin and secretes it into bile (giving bile a dark green color as it concentrates in gallbladder) --- gallbladder discharges bile into small intestine |
|
|
Where do RBCs develop? What stimulates their development? ***
|
- develop from hemocytoblasts in red bone marrow
- takes 3-5 days - 4 major developments: 1) reduction in cell size 2) increase in cell number 3) synthesis of hemoglobin 4) loss of nucleus and other organelles - blood stem cells (hemopoietic stem cells--HSC), which become - erythrocyte colony-forming units (ECFU) which are then - stimulated to mature by erythropoietin (EPO) into - erythroblasts (normoblasts), which multiply, synthesize hemoglobin, then eject the nucleus to become - reticulocytes, which leave the bone marrow and enter the circulating blood, where - over a day or two the last of the polyribosomes disintegrate and disappear and the cell becomes - mature erythrocyte development stimulated by: - EPO production by kidneys in response to: --- reduced blood flow to kidneys or reduced BP --- anemia - shortage of RBCs --- low O2 levels for other reasons (e.g., hypoxemia due blood loss, move to high altitude, or sudden increase in activity) - also stimulated by other hormones --- androgens --- GH - requires the presence of vitamin B12 (lack of B12 causes pernicious anemia) |
|
|
What determines your blood type? ***
|
- blood type depends on combinations of proteins present on RBC surface
- 3 major proteins --- A protein --- B protein --- D (Rh) proteins - people have antibodies against the proteins they lack - their systems will attack and agglutinate any cells with the foreign antigens |
|
|
What proteins (antigens) and antibodies are present in each blood type? ***
|
- Type A blood
--- surface antigen A --- anti-B antibodies - Type B blood --- surface antigen B --- anti-A antibodies - Type AB blood --- surface antigens A and B --- no anti-A or anti-B antibodies - Type O blood --- no surface antigens --- anti-A and anti-B antibodies |
|
|
How and when does hemolytic disease of the newborn occur? ***
|
- occurs when Rh- woman carries Rh+ fetus
- first pregnancy generally uneventful, because the placenta prevents intermingling of maternal and fetal blood - at birth or miscarriage, however, placental tearing can expose mother to Rh+ blood of fetus - she then begins to produce anti-D antibodies which in subsequent pregnancies may pass through placenta and agglutinate fetal RBCs of Rh+ baby - baby is born with severe anemia (HDN or erythroblastosis fetalis) - not always due to Rh incompatibility --- 2% can result from ABO incompatibility --- about 1 of 10 cases of ABO incompatibility result in HDN - easier to prevent than to treat - postnatal shot of Rh immune globulin (RhoGAM/Gamulin Rh) prevents mother from making antibodies - gives mother anti-Rh antibodies - given at 28-32 weeks gestation and at birth to Rh- mothers - destroy any transferred fetal blood |
|
|
What are the general characteristics of WBCs? ***
|
- large, nucleate blood cells
- no hemoglobin (which is why they are white) - approximately 1 wbc to every 1000 rbcs - can leave bloodstream --- margination – adhere to blood vessel walls (secrete sticky proteins) --- diapedesis – squeeze out of capillaries - amoboid movement - often found outside circulatory system - positive chemotaxis - release chemicals to attract other wbcs - some are phagocytic (neutrophils, monocytes, eosinophils) |
|
|
What are the major classes of WBCs and what are their functions? ***
|
- major classes: granulocytes and agranulocytes
- granulocytes --- neutrophils --- eosinophils --- basophils - agranulocytes --- lymphocytes --- monocytes 1) neutrophil - 60-70% of WBC count - most common WBC - cytoplasm stains neutrally/pale lilac; complex multi-lobed nucleus (polymorphonuclear leukocyte) - first WBC to leave blood and start immune defense - phagocytic - primary antibacterial WBC - release prostaglandins and leukotrienes --- increase capillary permeability --- attracts other leukocytes to area (chemotaxis) 2) eosinophil - 2-4% of WBC count - granular, cytoplasm stains pink/orange; large, bilobed nucleus - attack materials covered with antibodies (labeled as "foreign") - may be phagocytic - secrete toxic materials to kill targeted cells ("suicide bombers") --- can target much larger pathogens --- primary anti-parasitic WBC --- also active vs. allergens/in allergic reactions, collagen diseases, and diseases of spleen and CNS - may decrease inflammation triggered by other immune cells (anti-histamine response) - count fluctuates day/night, seasonally, and with phases of menstrual cycle 3) basophil - < 0.5% of WBC count - least common WBC - very coarse and granular, stains very dark blue/violet; likely obstructing nucleus - release granules of histamine and heparin at site of injury/infection --- histamine - promotes inflammation; vasodilates to increase blood flow --- heparin - prevents blood clots from forming (because some bacteria produce protective clots) release chemotaxic chemicals to attract other cells (eosinophils, neutrophils) - increases with chickenpox, sinusitis, DM, myxedema, polycythemia 4) lymphocyte - 25-33% - relatively agranular; large nuclei fill nearly entire cell, leaving scanty rim of clear, light cytoplasm - types --- T cells - cell-mediated immunity (attach and kill; blood) --- B cells - humoral immunity (make antibodies; spleen) --- NK cells - destroy abnormal tissues - increase in diverse infections and immune responses - destroy cancer cells, cells infected with viruses, and foreign cells - release chemicals to attract other immune cells (antigen-presenting cells) - coordinate actions of other immune cells 5) monocyte - 3-8% of WBC counts - largest WBCs - cytoplasm fairly clear; distinctive oval/kidney-shaped nucleus - life cycle --- start off in circulation as immature cells --- leave blood vessels and mature into macrophages - highly aggressive phagocytes (consume up to 25% of their own volume hourly) - count rises in response to inflammation and viral infections - found in specific tissues in body - release chemicals to attract other immune cells (antigen-presenting cells) |
|
|
What regulates the production of WBCs? ***
|
- occurs in multiple tissues
- all begin from hemopoietic stem cells (same cell as produces RBCs) - then become their specific colony-forming unit; from there, paths differentiate: --- myeloblasts become one of the types of granulocytes --- monoblasts become monocytes --- lymphoblasts become lymphocytes - development --- all develop in red marrow; some wait there until needed --- some lymphocytes move to lymphatic tissues and mature in thymus --- all lymphocytes eventually colonize spleen, lymph nodes, and other lymph organs/tissues - regulation --- thymus (thymosins) - differentiation of T and B cells --- colony stimulating factors - produced by other blood cells - each colony-stimulating factor stimulates a different WBC type to develop in response to specific needs (e.g., bacteria-neutrophil, parasite-eosinophil, virus-monocyte) |
|
|
How are platelets formed? ***
|
- characteristics
--- fragments of cell membrane --- contain clotting factors --- a.k.a. thrombocytes - functions - prevent loss of blood through injured vessels/tissues - production --- develop from megakaryocytes ("big nucleus cells") --- fragments of cytoplasm break off and form platelets - regulation --- thrombocyte stimulating factor from kidneys --- interleukins from wbcs --- colony stimulating factors --- thrombopoeitin from liver |
|
|
What happens during the vascular phase of hemostasis? ***
|
- vascular spasm
--- damaged blood vessels constricts through smooth muscle contraction --- reduces blood flow through damaged vessel - endothelial cells --- release factors to stimulate spasm --- become sticky/adherent helping to close vessel |
|
|
What happens during the platelet phase of hemostasis? ***
|
- platelet adhesion- they get sticky and adhere to:
--- endothelial cells --- basal lamina of endothelium --- exposed collagen fibers --- other platelets - form platelet plug - may plug opening in blood vessel - release chemical mediators --- promote healing --- promote clotting - clotting factors --- calcium ions - process is a positive feedback loop |
|
|
What happens during the coagulation phase of hemostasis? ***
|
- stimulated by protein factors - about a dozen chemicals in cascade
--- conversion of prothrombin to thrombin --- prothrombin converts fibrinogen to fibrin (insoluble, sticky threads) - fibrin forms insoluble fibers which tangle over opening --- form a net to catch escaping formed elements --- tangle of cells and fibrin forms clot - clot retraction --- platelets and fibrin filaments contract --- fibrin threads shorten and close wound --- allows healing to begin - healing - clot fibers broken down by enzymes |
|
|
What are the major circuits of the cardiovascular system? ***
|
- pulmonary circulation - carries blood to and from the lungs
- systemic circulation - carries blood to and from the rest of the body - blood alternates between the two systems |
|
|
Describe the general anatomy of the heart. ***
|
four chambers
- right atrium - receives blood from the systemic circuit - right ventricle - sends blood to the pulmonary circuit - left atrium - receives blood from the pulmonary circuit - left ventricle - sends blood to the systemic circuit |
|
|
Describe the flow of blood through the heart including the major vessels, valves and chambers. ***
|
- through superior/inferior venae cavae and coronary sinus to the
- right atrium, which contracts and sends blood through the - tricuspid valve/right atrioventricular valve to the - right ventricle, which contracts and sends blood up through the - conus arteriosus, then through the - pulmonary semilunar valve, through the - pulmonary trunk, which branches into the - R/L pulmonary arteries, which route the blood to the - lungs for oxygenation, then back through the - R/L pulmonary veins and into the - left atrium, through the - bicuspid valve/mitral valve/left atrioventricular valve into the - left ventricle, and out through the - aortic semilunar valve into the - ascending aorta, aortic arch, and coronary arteries to - all reaches of the body and the heart itself through the systemic circulation for gas exchange, then back to the - superior/inferior venae cavae and coronary sinus |
|
|
What are the tissue layers of the heart? ***
|
- pericardium - lining of the pericardial cavity
--- membranes ----- parietal pericardium - inner layer of the pericardial sac ----- visceral pericardium - the membrane that covers the heart itself (a.k.a., epicardium) - pericardial cavity --- space between the pericardia --- contains lubricating pericardial fluid - epicardium --- outer covering of heart (a.k.a., visceral pericardium) --- simple squamous epithelium over loose connective tissue - myocardium --- thick muscular wall of the heart --- spiraling layers of cardiac muscle - endocardium --- lines chambers of heart --- squamous epithelium --- continuous with endothelium of vessels |
|
|
Describe the surface anatomy of the heart. ***
|
- located in pericardial cavity
- within mediastinum - center of thoracic cavity - oriented at an angle - top is called the base - large vessels leave here - pointed apex at bottom on left side - coronary sulcus - groove between atria and ventricles - posterior side contains coronary sinus - enlarged vessel which collects blood from cardiac veins - interventricular sulci - grooves between ventricles that contain: --- adipose tissue --- cardiac vessels |
|
|
How are cardiac muscle cells connected to each other? ***
|
- narrow striated cells with single, central nucleus and branching cells
- intercalated discs - disks of protein connecting neighboring cells - gap junctions between cells --- allow Ca++ to flow from one cell to another --- allow cells to stimulate contraction in neighboring cells - some cells are self-stimulating |
|
|
What is the function of gap junctions between cardiac muscle cells? ***
|
- gap junctions between cells
--- allow Ca++ to flow from one cell to another --- allow cells to stimulate contraction in neighboring cells |
|
|
Describe the general structure and function of each of the four heart chambers. ***
|
right atrium - receives blood from systemic circulation (via superior/inferior venae cavae and coronary sinus)
- contraction sends blood to right ventricle - passes through right atrioventricular valve (a.k.a., tricuspid valve) - separated from left atrium by interatrial septum - fossa ovalis remnants of foramen ovale right ventricle - sends blood to pulmonary circulation - through conus arteriosus - then pulmonary (semilunar) valve - then into pulmonary trunk - branches into right and left pulmonary arteries left atrium - blood returns to heart through pulmonary veins - leaves through left atrioventricular valve (a.k.a., bicuspid or mitral valve) - enters left ventricle left ventricle - thick muscular chamber - receives blood from left atrium - blood leaves through aortic (semilunar) valve - sent to systemic circulation |
|
|
What is the fibrous skeleton of the heart? ***
|
- tough bands of connective tissue at base of heart
--- support valves and major vessel openings --- provide solid anchor for cardiocyte contraction --- non-conductor prevents A-V transmission (slows signal between atrium and ventricle, allowing complete contraction of atrium) |
|
|
Describe the cardiac circulatory circuit. ***
|
coronary arteries
- branch off at base of aorta - take blood to the heart muscle coronary veins - take blood back to sinus coronary sinus - collects blood from coronary veins - blood passed into right atrium |
|
|
What are the two functional roles of different cardiac cells? ***
|
heart contracts in organized fashion - first the atria, then the ventricles
types of cardiac muscle cells - conductive cells --- control and coordinate the heartbeat --- fewer myofibrils than other muscle cells - contractile cells --- produce contractions --- autorhythmic |
|
|
Where does the cardiac cycle begin? ***
|
the pathway
- action potential at the SA node - transmitted by the conductive cells - contractile cells receive AP and contract |
|
|
How is the signal carried through the atria and ventricles? ***
|
The Conducting System
- a system of specialized cardiac muscle cells --- starts and distributes the electrical impulses that stimulate contraction - parts --- the sinoatrial (SA) node - region of cells in wall of right atrium --- the atrioventricular (AV) node - located between atrium and ventricles --- conducting cells - connect the SA and AV nodes ----- distribute the stimulus through the heart - the conductive pathways --- internodal pathways in atria --- distribute the impulse to atrial cells and the AV node - ventricular conducting cells --- AV bundle --- bundle branches --- Purkinje fibers The Process - sinoatrial node --- in posterior wall of right atrium --- contains pacemaker cells --- initiates heartbeat as cells depolarize spontaneously --- begins atrial contraction - internodal pathways --- carry depolarization to AV node --- spread depolarization to other atrial cells - atrioventricular (AV) Node --- in floor of right atrium --- receives impulse from SA node --- impulse is delayed in AV node (small fibers) --- ensures atrial contraction finishes first - atrioventricular bundle --- takes signal from AV node and distributes to ventricular conduction fibers - bundle branches and Purkinje fibers --- distribute signals to regions of ventricles --- signal goes to bottom first |
|
|
How does the heart ensure atrial contraction finishes before ventricular contraction? ***
|
- atrioventricular (AV) Node
--- in floor of right atrium --- receives impulse from SA node --- impulse is delayed in AV node (small fibers) --- ensures atrial contraction finishes first |
|
|
What does an electrocardiogram measure? ***
|
- measures electrical activity/changes in the heart
- measures health of heart --- width of peaks --- height of peaks |
|
|
What are the major peaks and intervals of the EKG and what do they signify? ***
|
peaks
- P wave - represents atrial depolarization - QRS wave - represents ventricular depolarization - T wave - represents repolarization of ventricles important intervals - PR interval --- represents time between atrial and ventricular depolarization --- measure of conduction within heart - P-T interval --- the full heart cycle --- from atrial depolarization to ventricular repolarization --- after MI, dead tissue increases this time--can help dx - T-P interval --- time between cycles --- period for coronary circulation |
|
|
What is the role of calcium in cardiac muscle contraction? Where does it come from? ***
|
- calcium triggers contraction
--- frees myosin binding sites on actin filaments - sources of calcium --- extracellular – calcium enters through slow Ca channels --- intracellular – SR releases Ca in response to depolarization and elevated Ca levels |
|
|
How is a cardiac twitch different than a skeletal muscle twitch? ***
|
depolarization (this portion is the same in both cardiac and skeletal muscle twitch)
- very rapid - due to fast Na+ channels opening - open quickly and close plateau - slow Ca++ channels open - influx of Ca++ counteracts effects of Na+/K+ pumps - membrane doesn’t repolarize repolarization - K+ channels open and K+ diffuses out refractory period - time during which muscle cannot contract - restoration of membrane potentials role of calcium - calcium triggers contraction - frees myosin binding sites on actin filaments - sources of calcium --- extracellular – calcium enters through slow Ca channels --- intracellular – SR releases Ca in response to depolarization and elevated Ca levels long slow contractions - this is how the heart maintains the slow (approximately 70 bpm) heart rate |
|
|
What causes the difference between a cardiac twitch and a skeletal muscle twitch? ***
|
Ca++ counteracts repolarization, producing a plateau and a long reset period before the cardiac muscle is capable of contracting again
plateau - slow Ca++ channels open - influx of Ca++ counteracts effects of Na+/K+ pumps - membrane doesn’t repolarize repolarization - K+ channels open and K+ diffuses out refractory period - time during which muscle cannot contract - restoration of membrane potentials |
|
|
Describe the steps of the cardiac cycle. ***
|
period from start of one heartbeat to start of next
steps - systole - contraction of the chamber (upper number of BP) - diastole - relaxation of the chamber (lower number of BP) (while there is an atrial systole and diastole, our BP measurements represent ventricular systole and diastole) phases - atrial systole --- atria contract --- blood forced into ventricles --- backflow into veins prevented by valves in veins and small openings into atria - atrial diastole --- atria relax (chambers only fill when relaxed) --- fill with venous blood --- AV valves prevent backflow of ventricular blood --- simultaneous with ventricular systole - ventricular systole --- ventricles contract --- increased ventricular pressure closes AV valves --- first heartbeat sound ("lub") --- increased pressure opens semilunar valves --- blood forced into pulmonary artery and aorta - ventricular diastole --- ventricles relax --- change in pressure closes semilunar valves --- second heart sound ("dub") --- blood begins to come in through AV valves due to negative pressure "lub" = AV valves closing and beginning of ventricular contraction "dub" = semilunar valves closing and end of ventriculation contraction |
|
|
What are the two main variables influencing blood pressure? ***
|
cardiodynamics - the study of the movement and force of cardiac output
blood pressure - the hydrostatic pressure on the blood - dependent on two factors --- cardiac output - force at which blood is being pumped --- peripheral resistance - how much vessels are resisting |
|
|
What are chronotropic and inotropic factors? ***
|
influencing factors
- chronotropic factors – affect heart rate - inotropic factors – affect force of cardiac contraction |
|
|
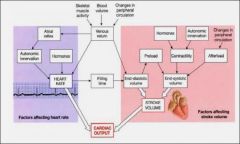
What are EDV, ESV, SV and CO? ***
|
cardiac variables
- end-diastolic volume (EDV) --- amount of blood in each ventricle at the end of diastole --- pre-contraction blood volume (could also call it pre-systolic volume) - end-systolic volume (ESV) --- amount of blood in each ventricle at end of systole --- post-contraction blood volume - stroke volume --- volume of blood pumped from each ventricle SV = EDV – ESV - generally only read left ventricle - ejection volume --- percentage of EDV represented by SV --- percentage of blood pumped out of ventricle - cardiac output --- amount of blood pumped out of heart in one minute CO = SV X HR (bpm) |
|
|
What are the major factors affecting heart rate? ***
|
- autonomic innervation
--- sympathetic neurons - post-ganglionic fibers from upper thoracic and cervical ganglia - parasympathetic neurons --- vagus nerve (X); synapse in cardiac plexus - cardiac reflexes --- chemo and baroreceptors in major vessels send sensory input to medulla - regulation --- cardiac center in medulla ----- cardioacceleratory center - sympathetic adrenergic fibers increase rate of depolarization in SA node ----- cardioinhibitory center - parasympathetic cholinergic fibers slow depolarization of SA node cells - the atrial reflex - stretch receptors in atria stimulate cardioaccelerator center - hormones --- epinephrine, norepinephrine, thyroid hormones can all increase heart rate |
|
|
What are the major factors affecting stroke volume? ***
|
1. EDV
- filling time (heart rate) - venous return rate 2. preload - amount of stretch in ventricular sarcomeres - more stretch = more forceful contraction 3. ESV - determined by ventricular contraction --- sympathetic stimulation (NE) increases contractility --- parasympathetic stimulation (ACh) decreases contractility - afterload --- amount of force (pressure) in arteries --- resists the contraction of the ventricles |
|
|
What is preload and afterload? ***
|
preload
- the amount of tension in the ventricular myocardium immediately before it begins to contract - the greater the stretch, the more forcefully the ventricles contract, thus expelling more blood and adjusting CO to the increase in venous return afterload - the sum of all forces a ventricle must overcome before it can eject blood - most significant contribution is the BP in the aorta and pulmonary trunk immediately distal to semilunar valves--it opposes opening of these valves and limits stroke volume |
|
|
How can the body affect EDV, ESV, preload, and stroke volume? ***
|
- increased HR
- hormones (e.g., NE) - increase in activity increases squeezing of skeletal muscles - dehydration |
|
|
What are the classes of blood vessels and how do they differ structurally? ***
|
- arteries - take blood away from heart
- arterioles - smallest arteries (these have greater musculature and smaller lumina) - capillaries - networks of small vessels --- most abundant vessels --- most body cells are within 1-2 cells of a capillary --- more blood in capillaries than in large vessels --- gas, nutrient exchange (more or less just a tube of endothelium) - venules - small veins - veins - return blood to heart (these have lesser musculature and larger lumina) |
|
|
What are the tissue layers of blood vessels and what types of tissue do they contain? ***
|
tunica intima
- innermost layer - simple squamous epithelium - endothelium - continuous with the endothelium of the heart - elastic connective tissue outside tunica media - middle layer - smooth muscle tunica externa - outer layer - connective tissue covering - continuous with surrounding tissue (e.g., areolar, etc.) - may also anchor vessel to surrounding tissues |
|
|
What are the structural differences between elastic arteries, muscular arteries and arterioles? ***
|
conducting arteries (a.k.a., elastic arteries or muscular arteries)
- large diameter arteries - elastic walls --- expand during ventricular systole --- contract and push blood during ventricular diastole - dampen systolic/diastolic difference distributing arteries (a.k.a., muscular arteries) - medium-sized arteries - thinner tunica externa arterioles - small diameter arteries - tunica externa very thin or absent - thin layer of muscle (tunica media) elastic rebound/recoil - during systole, arterial walls stretch, during diastole, they return to their original size (elastic rebound), keeping the blood moving in the arteries when not under direct pressure from the heart. ****** He said to count on this being a test question!!!!******* |
|
|
What are new continuous and fenestrated capillaries and generally where are they found? ***
|
(not sure why "new" but:)
thin walled vessels - no tunica externa or media; tunica intima only - simple squamous epithelial and some connective tissue - endothelium only diffusion of nutrients, gases - close to most cells in body continuous capillaries - endothelium forms continuous lining --- no openings in cell membranes --- water, small solutes, non-polar materials can pass - modified to form blood brain barrier --- tight junctions between cells (surrounded by astrocytes) fenestrated capillaries - endothelial cells have pores --- allow increased exchange of fluids through walls --- found in places where increased filtration is needed (e.g., kidneys are very leaky) - distribution of pores varies sinusoids - loose network of highly fenestrated capillaries - allow movement of large molecules and even cells out into interstitial spaces - found in large, highly vascular organs (e.g., liver, spleen, etc.) |
|
|
What are the parts of a capillary plexus? ***
|
- interconnected network of capillaries
- metarterioles and throughfare channels --- pass directly through plexus - precapillary sphincters --- constrict/dilate to control blood flow through plexus --- e.g., to move blood away from skin to avoid heat loss when individual is cold - arteriovenous anastomoses --- bypasses capillary beds |
|
|
What are pre-capillary sphincters and what is their role? ***
|
- precapillary sphincters
--- constrict/dilate to control blood flow through plexus --- e.g., to move blood away from skin to avoid heat loss when individual is cold --- when sphincters are open, the capillaries are well perfused --- when the sphincters are closed, little to no blood flow occurs |
|
|
What is the general anatomy of a vein and how are they different from arteries? ***
|
characteristics
- thin walled - thinner tunica media - larger lumina - valves --- infoldings of endothelium --- prevent backflow of blood --- needed due to reduced blood pressure --- found in limbs --- skeletal muscle contractions help move blood types of veins - venules - thin tunica externa - medium sized veins --- thicker tunica externa --- thin tunica media - large veins --- thick tunica externa --- thin tunica media --- may use skeletal muscles to help blood flow |
|
|
Where is most of the blood in the body found? ***
|
blood is unevenly distributed in the body:
- systemic circuit - 84% - pulmonary circuit - 9% - heart - 7% within the systemic circuit: - veins - 64% - arteries - 15% - capillaries - 5% veins hold the blood reserve capacitance - ability to store blood when stretched (not static) ****He hinted at this one for a test question!!!!***** - veins have high capacitance due to thin walls |
|
|
Where is blood pressure highest? Where is it lower? ***
|
blood pressure
- hydrostatic pressure on blood - must be adequate to return blood to heart --- must overcome peripheral resistance (friction of vessels) - lowest in veins, highest in arteries --- measured as arterial blood pressure --- mm Hg --- veins provide peripheral resistance (afterload) |
|
|
Why do you have to have your blood under pressure? ***
|
must be adequate to return blood to heart
- must overcome peripheral resistance (friction of vessels) peripheral resistance (PR) - vascular resistance - due to friction of blood within vessels - vessel length - long vessels provide more resistance - vessel diameter - small vessels have higher friction --- vasodilation and vasoconstriction - viscosity --- viscosity of blood affects PR --- normally constant, but can vary with conditions - turbulence --- changes in direction --- irregularities of vessel surface |
|
|
What causes the fluctuations in arterial pressure and why are they not present in venous pressure? ***
|
arterial pressure
- changes during cardiac cycle --- systolic pressure - highest value --- diastolic pressure - lowest value --- hypertension/hypotension - elastic rebound --- large arteries expand during systole --- during diastole, they go back to original size --- blood is forced along the vessel --- maintains blood flow during diastole (when heart is not creating pressure) venous pressure - pressure in veins is lower than arteries - resistance is decreasing as blood flows through veins - aided by other systems --- muscular compression - contraction of skeletal muscles forces blood through veins --- respiratory pump - changes in pressure of thoracic cavity (i.e., by breathing) move blood in/out of venae cavae |
|
|
What is elastic rebound and how does it contribute to blood pressure? ***
|
elastic rebound
- large arteries expand during systole - during diastole, they go back to original size - blood is forced along the vessel - maintains blood flow during diastole (when heart is not creating pressure) |
|
|
What mechanisms are present to keep blood flowing in veins? ***
|
venous pressure
- pressure in veins is lower than arteries - resistance is decreasing as blood flows through veins - aided by other systems --- muscular compression - contraction of skeletal muscles forces blood through veins --- respiratory pump - changes in pressure of thoracic cavity (i.e., by breathing) move blood in/out of venae cavae |
|
|
Where is hydrostatic pressure high in a capillary plexus? Why? ***
|
- hydrostatic pressure in a capillary plexus is:
--- high in arterial end --- low in venous end - pressure forces fluids out of blood by filtration (a "pushing force") --- fluids moving across porous barrier under pressure --- large solutes and cells left behind |
|
|
Where is osmotic pressure high in a capillary plexus and why? ***
|
osmotic pressure increases as blood passes through capillary plexus
- low in arterial end - high in venous end - fluid lost through filtration --- interstial fluids become more dilute --- blood becomes more concentrated - difference in solute concentrations draws fluid back into capillary --- fluid balance restored by lymphatic system --- no fluid balance can lead to edema osmosis (a "pulling force") - diffusion of water across a membrane to areas of high solute concentration - osmotic pressure pulls water towards high solute areas |
|
|
What is filtration? ***
|
- pressure forces fluids out of blood by filtration (a "pushing force")
--- fluids moving across porous barrier under pressure --- large solutes and cells left behind |
|
|
What happens if the fluid lost through filtration exceeds the fluid recovered through osmosis? ***
|
fluid remains in the tissues, causing edema
|
|
|
How is blood pressure regulated –
- at the local level? - neurally? - through reflexes? *** |
autoregulation (local) BP regulation
- local vasodilators and vasoconstrictors --- released by tissues to increase/decrease blood flow to area - control blood flow in individual capillary beds --- regulate precapillary sphincters neural mechanisms - cardiac center in medulla --- sympathetic stimulation = increase heart rate --- parasympathetic stimulation = decreased heart rate - vasomotor center --- stimulates vasodilation or vasoconstriction baroceptor reflexes - found in carotid and aortic sinuses - constantly depolarizing and sending pressure signals to medulla chemoreceptor reflexes - measure CO2, O2, and pH - send information to medulla |
|
|
Which hormones are involved in the regulation of blood pressure?
- Where are they produced/released? - How do they affect blood pressure? *** |
- NE/E
--- released by adrenal medulla --- stimulates vasoconstriction and increases CO - ADH --- released by posterior pituitary in response to drop in BP --- stimulates vasoconstriction --- stimulates recovery of water from urine --- recovered water increases blood volume = increased BP - angiotensin --- renin released by kidney (juxtaglomerular cells) in response to low BP (renin-angiotensin cascade) --- renin converts angiotensinogen to angiotensin I in liver --- angiotensin I converted to angiotensin II in lungs --- angiotensin II roles ----- stimulates production of aldosterone in adrenal cortex -------- increased Na+ resorption = increased water resorption ----- stimulates ADH release ----- stimulates cardioacceleratory center ----- stimulates vasoconstrictor center ----- more water = increased BP - EPO - released by kidneys in response to low BP or blood O2 - stimulates maturation of RBCs - more RBCs = more viscous blood = more resistance = increased BP - natriuretic peptides (reverse effect - lowers BP) --- released by cardiac muscle and brain vessel cells when stretched ----- increase sodium excretion in urine ----- increase water excretion in urine ----- decrease thirst ----- block release of BP-increasing hormones (ADH, aldosterone, renin-angiotensin cascade) ----- stimulate vasodilation when BP drops juxtaglomerular cells relax and make renin ---> angiotensin I/II ---> aldosterone ---> ADH ***** What effect does the (adrenal cortex, e.g.) have on BP? He gave this (with a varying organ/endocrine gland) as a test question possibility!!!!!****** |
|
|
How is the regulation of blood pressure dependent on the
- heart? - lungs? - kidneys? - vessels? - medulla? - adrenal medulla? - posterior pituitary? *** |
heart - natriuretic peptide released when cardiac muscle stretched
lungs - sensory bodies located in the aorta and carotid arteries as well as in the brain monitor the oxygen and carbon dioxide levels in the blood. An increased concentration of carbon dioxide signals the lungs to breathe more deeply, and the heart pumps harder kidneys - juxtaglomerular cells detect drop in BP and release renin, which triggers the renin-angiotensin cascade, which ultimately signals for the release of aldosterone (adrenal cortex) and ADH (posterior pituitary) to retain Na+ and water; also kidney releases EPO to increase RBC count, thereby increasing blood viscosity and resistance to flow, thus increasing BP vessels - vasodilate or vasoconstrict in response to hormonal or ANS control medulla - baroceptors relay data to vasomotor center regarding BP - cardiac center – sympathetic, parasympathetic system make adjustments in BP adrenal medulla - releases NE/E; stimulates cardiac and vascular alpha and beta-receptors, resulting in vasoconstriction of both the arterial and venous side of the circulation (alpha-receptors) and increased contractility of the heart (beta-receptors) posterior pituitary - releases ADH which increases fluid retention, increases blood volume, thus increases BP |
|
|
What is the function of the lymphatic system? ***
|
functions
- return excess interstitial fluid to blood - localize and distribute cells of immune system - absorb and transport non-polar nutrients, particularly lipids |
|
|
What is the function of the immune system? ***
|
- a population of cells
- found in many organs - function --- defense of the body against foreign pathogens |
|
|
Where is the immune system located? ***
|
- it is not a "true" system, it is poorly defined
- exists as a population of cells found in many organs |
|
|
What are the components of the lymphatic system? ***
|
- lymph
- lymphatic vessels - lymphatic tissues - aggregates of lymphoytes and macrophages that populate many organs of the body - lymphatic organs - places in which lymphatic tissue is especially concentrated and which are set off from surrounding organs by connective tissue capsules |
|
|
What is lymph? ***
|
- clear colorless fluid derived from blood plasma
- lower protein content - may contain immune cells, cellular debris, hormones, bacteria, etc. |
|
|
Where does lymph come from? ***
|
- lymph is the fluid "left over" from systemic circulation
- when blood flows through capillaries, some of the fluid leaves the capillaries through filtration, and not all is recaptured via osmosis - the leftover fluid subsequently is driven into openings in the lymphatic capillaries by hydrostatic pressure in the interstitial spaces |
|
|
How is lymphatic fluid different than blood? ***
|
- clear and colorless
- derived from blood plasma - lower protein content - contains immune cells, cellular debris, hormones, bacteria, etc. that were picked up in the interstitial spaces and will be brought through the system for filtering |
|
|
How are lymphatic capillaries different than blood capillaries? ***
|
lymphatic capillaries (a.k.a., terminal lymphatics)
- closed end capillaries - overlapping flap-like endothelial cells - hydrostatic pressure in interstitial space forces fluid and loose cells into capillary |
|
|
What pathway does lymph follow back to the blood? ***
|
- larger lymphatic vessels
--- collect lymph from capillaries --- similar in structure to veins --- overlapping endothelial cells form valves, prevent backflow --- fluid passes through lymph nodes - lead into larger collecting vessels and lymphatic trunks --- eventually carries lymph back to subclavian veins lymphatic ducts drain lymph back into subclavian veins - right lymphatic duct --- drains lymph from right side of upper body --- drains into right subclavian vein - thoracic duct --- drains lymph from lower body and left side of upper body --- drains into left subclavian vein |
|
|
How does lymph move through lymphatic vessels? ***
|
lymph flow
- forces --- contraction of lymphatic vessels --- skeletal muscle contraction --- arterial pressure (pulse) --- respiratory pump in thoracic cavity - slow, low pressure flow --- stimulated by activity |
|
|
Which lymphatic ducts drain which regions of the body? ***
|
- right lymphatic duct
--- drains lymph from right side of upper body --- drains into right subclavian vein - thoracic duct --- drains lymph from lower body and left side of upper body --- drains into left subclavian vein |
|
|
What are the three main types of lymphocytes? ***
|
lymphatic cells - found in various tissues of the body
- natural killer cells (NK) --- phagocytes --- immune surveillance - looking for damaged host cells - T cells --- maturation depends on thymic hormones --- mature in thymus --- cell-mediated immunity - B cells --- mature in bone marrow --- humoral immunity (fluid) |
|
|
What are the other cells of the lymphatic system? ***
|
- macrophages
--- mature monocytes that migrate from the bloodstream --- powerful phagocytes - dendritic cells --- macrophage-like cells of the epidermis - reticular cells --- specialized antigen-presenting cells (APCs) found in some connective tissues |
|
|
What is diffuse lymphatic tissue? ***
|
- there are masses of lymphocytes within mucosa of some organs
- diffuse lymphatic tissue --- scattered lymphocyte masses in respiratory and digestive tracts --- Mucosa-associated Lymphatic Tissue (MALTs) |
|
|
What are lymph nodules? ***
|
- dense masses of lymphocytes and macrophages
--- generally found in the same places in different people - localized patches such as Peyer’s Patches (small intestine), tonsils - enlarge during times of infection - nodules are not the same thing as nodes!! --- a lymph nodule differs from a lymph node in that it is much smaller and does not have a well-defined connective-tissue capsule as a boundary --- it also does not function as a filter, because it is not located along a lymphatic vessel --- lymph nodules frequently contain germinal centres—sites for localized production of lymphocytes. |
|
|
Where are some of the major lymph nodules located? ***
|
- digestive system
- respiratory system and - urinary bladder - lymph nodules form in regions of frequent exposure to microorganisms or foreign materials and contribute to the defense against them - in the small intestine, collections of lymph nodules are called Peyer’s patches - the tonsils are also local regions where the nodules have merged together |
|
|
What is the role of red marrow to the lymphatic system? ***
|
lymphatic organs - two groups
- primary lymphatic organs --- site of development of immunocompetence of T/B cells - secondary lymphatic organs --- site of maturation and storage of immunocompetent cells - red marrow is a primary lymphatic organ in that it contains hematopoietic cells (is a place where they develop) |
|
|
What is the role of the thymus in the lymphatic system? ***
|
- bilobed organ in mediastinum
- made of active regions separated by trabeculae - release chemicals to stimulate T cell maturation - involution --- reaches max around 5-6 --- after age 60, reduced to fatty tissue |
|
|
What is the role of the lymph nodes in the lymphatic system? ***
|
- elongated, bean-shaped structure
--- fibrous capsule --- compartments separated by trabeculae - found along lymphatic vessels where they --- immunologically filter lymph as it passes through --- cleanse lymph of foreign materials and damaged cells --- house lymphocytes --- enlarge during times of infection due to increase in number of lymphocytes (lymphadenitis – enlargement of nodes) |
|
|
How does fluid flow through lymph nodes (the path)? ***
|
- series of afferent lymphatics bring lymph into the node along convex surface
- lymph flows from these vessels into the subcapsular sinus - percolates slowly through sinuses of cortex and medulla (flows through sinusoids like water through sand) - lymphocytes remove foreign/damaged tissues - leaves the node through 1-3 efferent lymphatic vessels that emerge from the hilum |
|
|
What are the sinusoids/sinuses of the lymph node? ***
|
passageways through which the lymph passes for filtering
(this is not from his slides--there is no answer to this question on the slides and the book is not much more help) from Wikipedia: - sinus is a channel within the lymph node lined by the endothelial cells along with fibroblastic reticular cells and allows for smooth flow of lymph through them --- subcapsular sinus is a sinus immediately deep to the capsule, and its endothelium is continuous with that of the afferent lymph vessel; it is also continuous with similar sinuses flanking the trabeculae and within the cortex (cortical sinuses) --- cortical sinuses and that flanking the trabeculae drain into the medullary sinuses, from where the lymph flows into the efferent lymph vessel |
|
|
What types of cells are found in lymph nodes? ***
|
lymphocytes
- T-cells - B-cells - macrophages also - dendritic cells - plasma cells - reticular cells |
|
|
What is the role of the lymphatic system in metastasis of cancer? ***
|
metastatis and lymph nodes
- cancer cells break free from tumor, circulate into interstitial spaces, then are picked up by lymph - move into lymphatics, get stuck and reproduce - node destroyed, cells move to next node - lymphoma = cancerous lymph node |
|
|
What is the role of the spleen? ***
|
- located in the abdominal cavity lateral to the stomach
- basically, like a "giant" lymph node - very susceptible to rupture - RBC "graveyard" - hilus --- indentation on medial side --- splenic artery and veins enter here - fibrous capsule - reticular fibers - support cells inside - blood flow --- brought in by splenic artery (branch of celiac trunk) --- capillaries release blood into sinuses of spleen --- trabecular veins collect blood --- returned to hepatic portal vein by splenic vein - red pulp --- open areas of reticular tissue containing blood - white pulp --- masses of lymphocytes --- “cleanse” blood |
|
|
How does blood flow into and through the spleen? ***
|
- blood flow
--- brought in by splenic artery (branch of celiac trunk) --- capillaries release blood into sinuses of spleen --- trabecular veins collect blood --- returned to hepatic portal vein by splenic vein |
|
|
What is the general structure of the spleen? ***
|
- located in the abdominal cavity lateral to the stomach
- basically, like a "giant" lymph node - very susceptible to rupture - RBC "graveyard" - hilus --- indentation on medial side --- splenic artery and veins enter here - fibrous capsule - reticular fibers - support cells inside - red pulp --- open areas of reticular tissue containing blood - white pulp --- masses of lymphocytes - “cleanse” blood |
|
|
True or false: The cardiovascular system includes the heart and blood vessels.
|
True
(The circulatory system includes the blood) |
|
|
List the three layers of the heart wall from deep to superficial.
|
- endocardium
- myocardium - epicardium |
|
|
The ____ is the layer that lines the inner chambers of the heart.
|
endocardium
|
|
|
When a normal heart rate is established by the appropriate firing of the SA node, this is known as a _____ rhythm.
|
sinus
|
|
|
The term ______ refers to contraction of the heart.
|
systole
|
|
|
The _____ side of the heart supplies blood to the pulmonary circuit.
|
right
|
|
|
The _____ circuit of the cardiovascular system carries blood to the body (excluding the interior of the lungs) then returns it to the heart.
|
systemic
|
|
|
The depolarization of the SA node (from threshold to peak) is due to the inflow of _____ and _____ ions.
|
- sodium
- calcium |
|
|
The term _____ refers to relaxation of the heart.
|
diastole
|
|
|
The inferior end of the heart that tapers to a blunt point immediately above the diaphragm is called the _____ of the heart.
|
apex
|
|
|
The broad, flat, superior top portion of the heart is known as the ______.
|
base
|
|
|
The _______ are the lower chambers of the heart that pump blood to the lungs and to the body.
|
ventricles
|
|
|
_______ are short, thick, branched muscle cells of the heart.
|
cardiac myocytes
|
|
|
The amount of blood pumped by the left ventricle is ____ the amount of blood pumped by the right ventricle.
|
equal to
|
|
|
The volume of blood ejected from the left ventricle as measured in liters/minute is known as the _____ _____.
|
cardiac output
|
|
|
Pressure and volume within a chamber are:
|
inversely proportional
|
|
|
The _____ is a composite recording of all nodal and myocardial action potentials.
|
EKG
|
|
|
Describe the flow of blood through the heart once blood has returned from the superior and inferior venae cavae.
|
- right atrium
- right ventricle - left atrium - left ventricle |
|
|
True or false: The left ventricle always pumps more blood per beat than the right ventricle.
|
false
(both ventricles must pump the same amount, otherwise blood will build up somewhere in the circulation) |
|
|
The artery that exits the aorta, travels under the left auricle, and then divides into two branches is the left _____ artery.
|
coronary
|
|
|
A normal heart rate, triggered by the SA node, is referred to as ______ rhythm.
|
sinus
|
|
|
The _____ nerve conveys parasympathetic signals to the heart.
|
vagus
|
|
|
List in correct order the major phases of the cardiac cycle, starting with ventricular filling.
|
- isovolumetric contraction
- ventricular ejection - isovolumetric relaxation |
|
|
The volume of blood ejected by the ventricles per minute is the:
|
cardiac output
(stroke volume is the volume of blood ejected by a ventricle in one contraction of the heart) |
|
|
The _____ _____ branch of the left coronary artery travels down to the apex of the heart.
|
anterior interventricular
|
|
|
As a chamber, such as a cardiac ventricle, contracts and begins to reduce its volume, the pressure of the fluid within would ______.
|
increase
|
|
|
With the onset of ventricular contraction, the pressure within the ventricles _______.
|
increases
(As the ventricles contract, the internal pressure rises sharply. At the initiation of contraction, the volume of blood is constant but the space containing the blood has just decreased, which causes the momentary increase in pressure. This increased pressure forces the blood to push against the AV valves, thus allowing the ejection of blood from the ventricle. |
|
|
With ventricular contraction, the ejection of blood occurs because the pressure within the ______ exceeds the pressure within the ______
|
- ventricles
- great arteries |
|
|
When ventricles are relaxed and their pressure is low, the _____ valves are open.
|
atrioventricular
|
|
|
Fluids always flow from an area of ____ pressure to an area of ____ pressure.
|
- high
- low |
|
|
The opening and closing of heart valves are governed by changes in ______ within heart chambers.
|
pressure
|
|
|
The blood pressure in the great arteries determines the ____ of the heart.
|
afterload
|
|
|
Cardiac output is equal to
|
SV x HR
|
|
|
The strength of a contraction for a given preload is defined as the _____ of the myocardium.
|
contractility
|
|
|
The epicardium is also called the:
|
visceral pericardium
|
|
|
The outer wall, with its superficial fibrous layer of dense, irregular connective tissue, is also called the _____ pericardium.
|
parietal
|
|
|
Blood flow through the coronary circulation increases during ventricular:
|
diastole
|
|
|
The study of the heart and its disorders is known as ______.
|
cardiology
|
|
|
In the posterior coronary sulcus is a large vein called the _____ _____ which collects venous drainage from all of the coronary veins and drains into the right atrium.
|
coronary sinus
|
|
|
List in order the events of an action potential of a ventricular cardiocyte.
|
- voltage-gated Na channels open
- influx of Na causes more Na channels to open; depolarization - Na channels close as membrane potential peaks at +30 mV - Ca enters through slow calcium channels; creates plateau - Ca channels close, K channels open; repolarization |
|
|
The pacemaker potential of SA node cells is due to the influx of _____ ions.
|
- sodium
(The pacemaker potential refers to a gradual depolarization due to a slow influx of sodium ions. When the pacemaker potential reaches a threshold of -40 mV, calcium channels open and calcium flows in, creating the total depolarization, which peaks slightly above 0mV. |
|
|
The ______ artery is a branch of the left coronary artery that continues around to the back of the heart in the coronary sulcus.
|
circumflex
|
|
|
A patient presents with a persistently elevated heart rate of over 100 bpm. This clinical condition is known as _____.
|
tachycardia
|
|
|
The closing of the atrioventricular valves produces which of the heart sounds?
|
the first ("lub")
|
|
|
______ is the process of listening to sounds made by the body.
|
auscultation
|
|
|
True or false: The coronary circulation is made up of the systemic blood vessels.
|
true
(The coronary circulation pertains to the heart, consisting of the blood vessels within the heart tissue.) |
|
|
The _____ center of the medulla oblongata initiates autonomic output to the heart.
|
cardiac
|
|
|
In a healthy person at rest, under the influence of the parasympathetic nervous system, the SA node normally fires about _____ times per minute, setting the heart rate.
|
75
|
|
|
A spontaneously developing local potential that generates action potentials in the SA node is called a(n) ____ potential.
|
pacemaker
|
|
|
The heartbeat is described as _____ because the signal for contraction originates in the heart muscle itself.
|
myogenic
|
|
|
The role of the papillary muscles is to:
|
tense the tendinous cords just prior to ventricular contraction
|
|
|
The right and left coronary arteries arise from the:
|
aorta
|
|
|
An increase in venous return to the heart leads to a(n) _______ in preload and therefor a(n) _____ in stroke volume.
|
- increase
- increase |
|
|
The amount of tension in the ventricular myocardium immediately before it begins to contract is known as the ______.
|
preload
|
|
|
True or false: Papillary muscles contract just before the rest of the myocardium in order to tense the tendinous cord prior to ejection of blood.
|
True
(Papillary muscles do contract first. By tensing the tendinous cords, they prevent the AV valves from being pushed up into the atria when ventricular ejection occurs |
|
|
Cardiac muscle requires oxygen and therefore relies on ____ metabolism to produce ATP.
|
aerobic
|
|
|
The cardiocytes are described as _____ because individual cells can depolarize on their own without outside stimulation.
|
- myogenic
- autorhythmic |
|
|
The term ____ refers to contraction of the heart.
|
systole
|
|
|
Describe stroke volume.
|
amount of blood ejected per beat
|
|
|
Which of the following chemicals can cause an increase in HR.
- caffeine - nicotine - acetylcholine - thyroid hormone |
- caffeine
- nicotine - thyroid hormone |
|
|
_______ is the electrolyte that has the greatest chronotrophic (heart rate) effect on the heart. An imbalance in this electrolyte is a medical emergency.
|
Potassium
|
|
|
The strength of contraction for a given preload is defined a the ______ of the myocardium.
|
contractility
|
|
|
The blood vessels that supply nutrients and oxygen only to the heart muscle make up the specific type of circulation called the ______ circulation.
|
coronary
|
|
|
The _____ circuit of the cardiovascular system carries blood from the right ventricle to the lungs for gas exchange and returns it to the left atrium of the heart.
|
pulmonary
|
|
|
The _____ circuit of the cardiovascular system carries blood to the lungs for gas exchange and returns it to the heart.
|
pulmonary
|
|
|
The _____ side of the heart supplies blood to the systemic circuit.
|
left
|
|
|
________ impedes the opening of the semilunar valves and opposes ventricular ejection.
|
afterload
|
|
|
The arterial branch that usually arises from the right coronary artery and supplies the back wall of the heart is the _____ _____ branch.
|
posterior descending
|
|
|
The _____ wave of an ECG is a recording of the depolarization of the atrial myocardium.
|
P
|
|
|
An ear-like extension of a heart chamber is known as a(n):
|
auricle
|
|
|
One cause of arrhythmia is _____ ______, failure of the cardiac conduction system to transmit signals.
|
heart block
|
|
|
Blood flow through the coronary circulation increases during ventricular:
|
diastole
|
|
|
The groove that extends downward from the coronary sulcus on the back of the heart is the posterior ________ sulcus.
|
interventricular
|
|
|
The groove that extends downward from the coronary sulcus on the front of the heart is the anterior _______ sulcus.
|
interventricular
|
|
|
True or false: The heart receives both sympathetic and parasympathetic stimulation.
|
true
|
|
|
Stimulation of the SA node by the _____ nervous system raises the heart rate.
|
sympathetic
|
|
|
Abnormal cardiac rhythm is known as ________.
|
arrhythmia
|
|
|
________ impedes the opening of the semilunar valves and opposes ventricular ejection.
|
afterload
|
|
|
An arterial _____ is a convergence of two arteries.
|
anastomosis
|
|
|
Ventricular contraction begins at the ______ of the heart.
|
apex
|
|
|
The difference between the maximum and resting cardiac output is known as the:
|
cardiac reserve
|
|
|
The _____ valves regulate the opening between the atria and the ventricles.
|
atrioventricular
|
|
|
The valve between the right atrium and ventricle is specifically called the ______ valve.
|
tricuspid
|
|
|
The alternate name for the left atriventricular valve is the _____ valve.
|
bicuspid (or mitral)
|
|
|
List ways the body uses iron.
|
- the muscles use Fe++ to make the myoglobin
- the bone marrow uses Fe++ for hemoglobin synthesis - nearly all cells use Fe++ to make electron-transport molecules (cytochromes) in their mitochondria |
|
|
The general term for limiting blood loss from an injured vessel is _______.
|
hemostasis
|
|
|
List in order the events of platelet plug formation.
|
- upon contact with collagen of a broken vessel, platelets grow long spiny pseudopods
- platelets adhere to exposed collagen and other platelets - the pseudopods then contract and draw the vessel wall together - this mass of platelets forms a platelet plug |
|
|
Define thrombocytopenia.
|
platelet count below 100,000
|
|
|
A _____ is a giant precursor cell with a multilobed nucleus which fragments to form platelets.
|
megakaryocyte
|
|
|
Name the three hemostatic mechanisms.
|
- vascular spasm
- platelet plug formation - blood clotting |
|
|
Thrombosis is more likely to occur in veins than in arteries because:
|
blood flows more slowly and does not dilute thrombin and fibrin as rapidly
|
|
|
A(n) _____ is a mass of clotted blood in the tissues.
|
hematoma
(A thrombus is a clot that forms in a blood vessel or heart chamber, which may break free and travel in the bloodstream as a thromboembolus) |
|
|
Name some mechanisms that prevent inappropriate clotting.
|
- presence of anticoagulants such as heparin and antithrombin
- dilution of clotting factors - platelet repulsion caused by prostacyclin |
|
|
When hypoxemia is detected, a mechanism of correction is initiated: erythropoietin is secreted by the kidneys and liver and the rate of erythropoiesis accelerates. This is an example of a(n):
|
negative feedback control
|
|
|
Cell fragments produced from megakaryocytes are called:
|
platelets
|
|
|
Describe vascular spasm
|
a short-lived mechanism in which the damaged vessel narrows to minimize blood loss
|
|
|
List, in order, the events that occur during fibrinolysis.
|
- prekallikrein is converted to kallikrein
- kallikrein catalyzes the formation of plasmin - plasmin dissolves the blood clot |
|
|
When collagen in the wall of a blood vessel is exposed as a result of injury, ______ grow long, spiny pseudopods which adhere to the vessel and draw its walls back together.
|
platelets
|
|
|
What is a pathogen? ***
|
an agent capable of causing disease
- can include living organisms and toxins |
|
|
What is an antigen? ***
|
- a molecule capable of triggering a specific immune response
- a cell bearing such a molecule |
|
|
What is the difference between non-specific resistance and specific immunity? ***
|
- non-specific resistance
--- general responses to any threat or foreign material (e.g., fever) --- put in place once external barriers/first line of defense have been penetrated - specific responses --- targeted to a particular antigen --- involve specific antigen-matched proteins (i.e., antibodies) --- once exposed, can produce memory cells to reduce response time in future exposures - often a nonspecific response is triggered while waiting for specific response to occur |
|
|
What are the three lines of defense in the immune system? ***
|
- first line – external barriers (skin, mucus, etc.)
- second line – non-specific defenses - third line – specific immunity (vs. 1 particular antigen) |
|
|
How does the epidermis contribute to the first line of defense? ***
|
- not easily penetrated
- nutrient poor surface (because it is dead tissue) - acid mantle --- lactic acid in sweat --- low pH of sebum - antibacterial secretions --- dermicidins and defensins (staphylococci tolerate lower pH; this is why most of us are colonized) |
|
|
How does mucosa contribute to the first line of defense? ***
|
- linings of the respiratory and digestive tracts (sticky)
- ciliary escalator keeps pathogens moving (eject via cough, etc.) - some mucosa release lysozyme --- antimicrobial enzyme in sweat, tears |
|
|
How does hyaluronic acid contribute to the first line of defense? ***
|
- thick gel-like material inhibits movement and growth of bacteria
(e.g., in matrix of cartilage) |
|
|
How do normal flora contribute to the first line of defense? ***
|
- non-pathogenic bacteria use up space and resources
- make environment difficult for pathogens (thrown off frequently by use of antibiotics) |
|
|
How do the neutrophils and macrophages contribute to the second line of defense? ***
|
neutrophils
- can phagocytize bacteria - can produce cytokines - can create a respiratory burst - rapidly absorb oxygen and --- produce a series of toxic ions (hydrogen peroxide, hypochlorite, etc.) --- destroy any cells around the neutrophil macrophages - mature monocytes - some wander, some localize --- microglial cells in CNS --- alveolar macrophages in lungs --- Kupffer cells - hepatic macrophages |
|
|
What is an activated macrophage? ***
|
- second line of defense
- under the influence of cytokines (particularly γ-interferon and interleukin 4), resting macrophages are activated - they become larger, more motile, stickier, express more MHCII proteins on their surface, contain more lysosomes and lysosomal enzymes, and secrete a variety of substances including interleukin 1 and tumor necrosis factors - they have increased phagocytic activity and increased killing via reactive oxygen intermediates, collagenases and lysosomal enzymes interferons - released by virally infected cells - stimulate production of antiviral proteins by neighboring cells - attract macrophages and NK cells |
|
|
Where are macrophages found? ***
|
- mature monocytes
- some wander, some localize --- microglial cells in CNS --- alveolar macrophages in lungs --- Kupffer cells - hepatic macrophages - second line of defense |
|
|
Which antimicrobial proteins are produced in the immune system? ***
|
- interferons
- complement system - second line of defense |
|
|
What is the role of the antimicrobial proteins produced in the immune system, and how do they do their job? ***
|
- interferons
--- released by virally infected cells --- stimulate production of antiviral proteins by neighboring cells --- attract macrophages and NK cells - complement system --- series of 30+ proteins --- perform many functions ----- activation of immune cells ----- binds foreign antigens to red blood cells (taken to liver for removal - immune clearance) ----- opsonization of pathogens ----- cytolysis of pathogens - second line of defense |
|
|
What does complement do and how does it do it? ***
|
- series of 30+ proteins
- perform many functions --- activation of immune cells --- binds foreign antigens to red blood cells (taken to liver for removal - immune clearance) --- opsonization of pathogens --- cytolysis of pathogens - second line of defense |
|
|
What is opsonization? ***
|
- complement system
- coating of microbial cells by C3b, which serves as binding sites for phagocyte attachment - process by which bacteria are altered by opsonins so as to become more readily and more efficiently engulfed by phagocytes |
|
|
What is an epitope? ***
|
- a.k.a. antigenic determinant
- the specific regions of an antigen molecule which stimulate immune responses and are recognized by antibodies, B-cells, or T-cells - usually are non-self proteins - one antigen molecule typically has several different epitopes that can stimulate production of different antibodies - second line of defense |
|
|
What is immune surveillance and which are the primary cells involved? ***
|
- NK cells look for damaged cells, infected cells
- release perforins - granzymes destroy enemy cell from within - second line of defense |
|
|
What causes fever? ***
|
- pyrogens released by some phagocytes
--- can be directly stimulated by certain bacterial glycolipids - benefits --- increase metabolism and immune activity --- inhibits some bacterial growth - second line of defense |
|
|
What is the purpose of fever? ***
|
- benefits
--- increase metabolism and immune activity --- inhibits some bacterial growth |
|
|
What causes inflammation? ***
|
functions
- limit spread of pathogens - localize and destroy pathogens - remove damaged tissues - attract immune cells to site of injury triggered by series of cytokines - vasoactive chemicals the process - cytokines cause --- increased capillary dilation - increased blood flow to area --- increased capillary permeability - increases: ----- margination (selectins cause leukocytes to adhere to blood vessel walls) and ----- diapedesis (leukocytes squeeze between endothelial cells into tissue space) - fibrinogen activated by damaged tissues --- clot forms --- traps bacteria in area surrounding injury --- heparin keeps tissues fluid inside of clot - allows WBC and complement to function - second line of defense |
|
|
What are the four cardinal signs of inflammation? ***
|
- warmth
- redness (erythema) - swelling (edema) - pain |
|
|
What produces the four cardinal signs of inflammation? ***
|
- warmth results from hyperemia
--- increased blood flow to the area - redness is also from the hyperemia --- may also be due to extravasated RBCs in the tissue (e.g., sunburn) - swelling is due to increased fluid filtration from the capillaries - pain results from --- direct injury to the nerves --- pressure on nerves from edema --- stimulation of pain receptors by prostaglandins, some bacterial toxins, and a kinin called bradykinin |
|
|
What is the purpose of inflammation? ***
|
functions
- limit spread of pathogens - localize and destroy pathogens - remove damaged tissues - attract immune cells to site of injury |
|
|
What role does fibrinogen play in the inflammatory process? ***
|
- fibrinogen activated by damaged tissues
--- clot forms --- traps bacteria in area surrounding injury --- heparin keeps tissues fluid inside of clot - allows WBC and complement to function - second line of defense |
|
|
The ability of a tissue to adjust its own blood supply through vasomotion or angiogenesis is known as -________.
|
autoregulation
|
|
|
A collateral route of blood supplied to a tissue is called a(n):
|
anasomosis
|
|
|
Degenerative changes of the blood vessels characterized by the presence of atheromas and often leading to calcification of the vessel wall is known as _______.
|
atherosclerosis
|
|
|
______ blood pressure is the arterial blood pressure attained during ventricular relaxation.
|
Diastolic
|
|
|
A ______ is an autonomic, negative feedback response to changes in blood pressure.
|
baroflex
|
|
|
An excess of carbon dioxide in the blood is known as ______.
|
hypercapnia
|
|
|
The physiological functions of vasomotion are to:
|
- regulate BP
- modify perfusion to an organ or tissue |
|
|
_______ is a process in which endothelial cells pick up material on one side of the plasma membrane by pinocytosis or receptor-mediated endocytosis, transport the vesicles across the cell, and discharge the material on the other side by exocytosis.
|
Transcytosis
|
|
|
The most significant factors which influence blood viscosity are:
|
- erythrocyte count
- albumin concentration |
|
|
Which of the following can easily diffuse through the plasma membrane?
- glucose - steroid hormones - electrolytes - large proteins - carbon dioxide - oxygen |
- steroid hormones
- carbon dioxide - oxygen |
|
|
All forms of circulatory shock fall into which two categories?
|
- low venous return shock
- cardiogenic shock |
|
|
The physical force exerted by a liquid against a surface such as a capillary wall is called ______ pressure.
|
hydrostatic
|
|
|
True or false: Large veins of the neck are normally collapsed and their venous pressure is close to zero.
|
true
|
|
|
The basal lamina is the non-cellular, proteinacious material that surrounds the capillary ______ cells and separates it from adjacent connective tissue.
|
endothelial
|
|
|
Common causes of hypovolemic shock include:
|
- dehydration
- burns - bleeding ulcers - hemorrhage |
|
|
True or false: Exercise decreases venous return.
|
false
|
|
|
Name the forces that oppose hydrostatic pressure along with the capillary and interstitial pressures.
|
colloid osmotic pressure
|
|
|
A ______ is an autonomic, negative feedback response to changes in blood pressure.
|
baroreflex
|
|
|
______ venules receive blood from the postcapillary venules.
|
Muscular
|
|
|
Portal systems occur in which of the following:
- between lungs and heart - between intestines and liver - kidneys - between the hypothalamus and anterior pituitary - brain |
- between the intestines and liver
- kidneys - between the hypothalamus and anterior pituitary |
|
|
The difference between the colloid osmotic pressure of the blood and that of the tissue fluid, usually favoring fluid absorption by the blood capillaries is known as _____ pressure.
|
oncotic
|

