![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
60 Cards in this Set
- Front
- Back
|
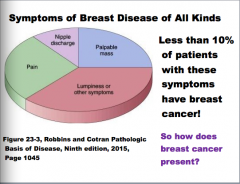
What are the symptoms of breast disease? How does it present? What percent of patients with these symptoms have breast cancer? |
|
|
|
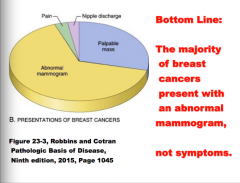
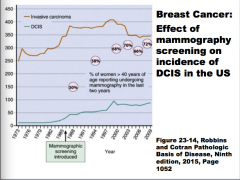
The majority of breast cancers present with abnormal _____, not symptoms. |
|
|

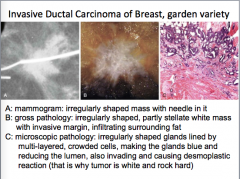
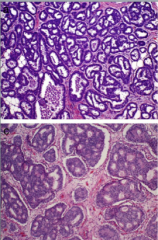
What is shown in A, B, C? |
|
|
|
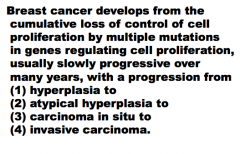
Breast cancer develops from the cumulative loss of control of cell _______ by multiple mutations in genes regulating cell proliferation, usually slowly progressive over many years, with a progression from...
What are the four steps in the progression? |
|
|
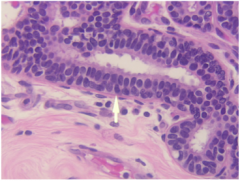
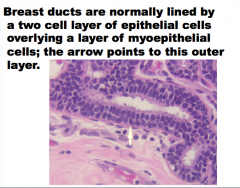
Breast ducts are normally lined by ____- cell layer of epithelial cells overlying a layers of ______ cells. The arrow points to which layer? |
|
|
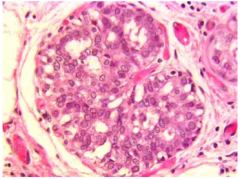
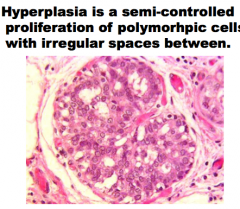
_____ is a semi-controlled proliferation of polymorphic cells with irregular spaces between. |
|
|
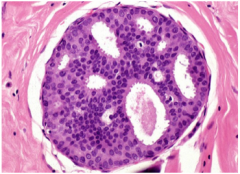
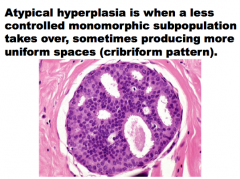
Atypical ______ is when a ______ controlled monomorphic subpopulation takes over, sometimes producing more uniform spaces (_______ pattern) |
|
|
|
What does the term cribriform mean? |
|
|
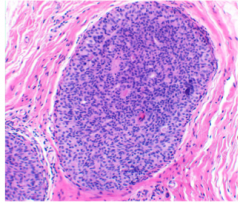
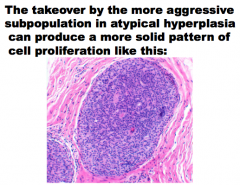
The takeover by the more ______ |
|
|
|
Carcinoma in situ is ______ transformation, producing cells capable of ______ and metastasis. There are features more common in |
|
|
|
Is there any feature in cancer and never in benign atypia?
|
No! Diagnosing carcinoma in situ requires assessing whether the weight of benign features is more than the weight of malignant features. |
|
|
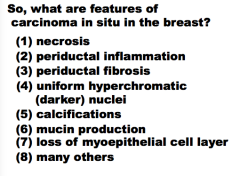
What are the features of carcinoma in situ in the breast? |
|
|
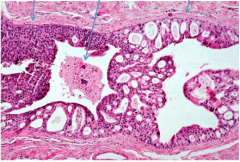
What is this? Identify the solid pattern, cribriform pattern, and necrosis. |

|
|
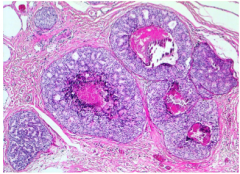
The necrosis can make the ducts look like _____ . What is this pattern called?
Is there peridicuctal inflammation here also? |

|
|
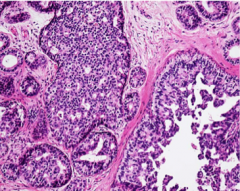
What does this carcinoma in situ show (nuclei)? |
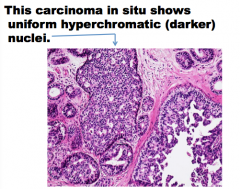
|
|
This carcinoma in situ has numerous ______. They are small round dark thing. How many are there? |

Calcifications are one of the most common ways to recognize carcinoma in situ. |
|
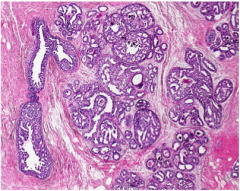
This carcinoma has a very large blob of _____ in the lumen. |

|
|
|
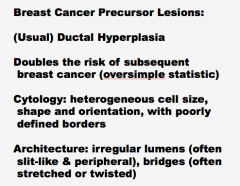
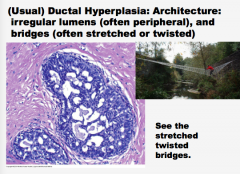
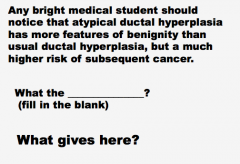
Breast Cancer Precursor Lesions:
(Usual) ______ Hyperplasia
______ the risk of subsequent
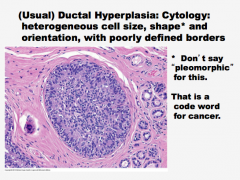
Cytology: ________s cell size,
Architecture: ______ lumens (often |
|
|
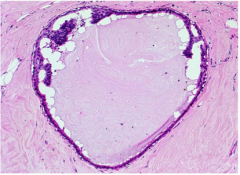
What is this? Cell size, shape and orientations, border. What word should you not use with this because it refers to cancer? |
|
|
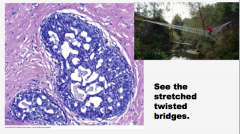
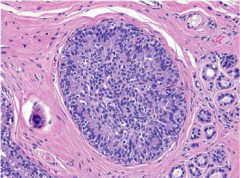
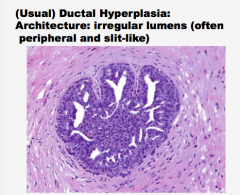
What is this? Comment on the lumens and the bridges. |
|
|
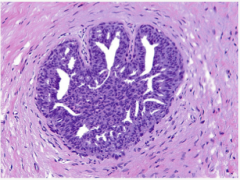
What type of hyperplasia? Are the lumens regular or irregular? |
|
|
|
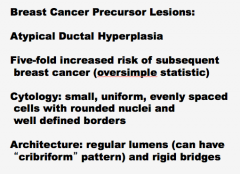
Breast Cancer Precursor Lesions:
Atypical Ductal Hyperplasia
_______-fold increased risk of subsequent
Cytology: small, _____, evenly spaced
Architecture: ______ lumens (can have |
|
|
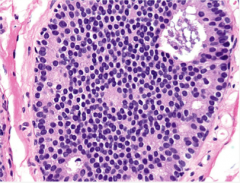
What type of hyperplasia? Comment on what you see and some of the typical findings of this type of hyperplasia. |
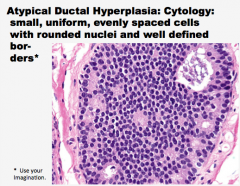
|
|
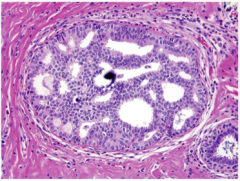
Again, what type of hyperplasia? Comment on the lumens (can they have a cribriform pattern)? What is the dark purple thing in the middle of the picture? |
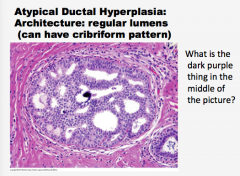
|
|
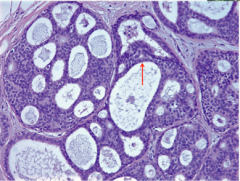
What type of hyperplasia? Comment on the bridges. |
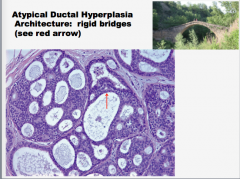
|
|
|
|
|
One of these is invasive. Only one is ductal carcinoma in situ. Which is invasive? |

|
|
|
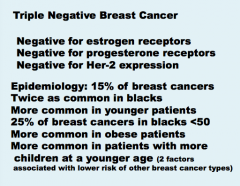
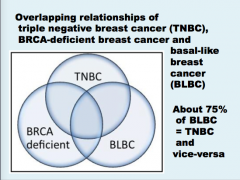
What is triple negative breast cancer?
Epidemiology? More common in what races, ages? Lifestyle? Children? |
|
|
|
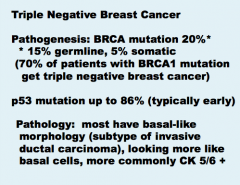
What is the pathogenesis of triple negative breast cancer?
What percent BRCA, germline, somatic?
70% of patients with BRCA1 mutation get ______ breast cancer.
What percent have p53 mutation?
What is the pathological stain? |
|
|
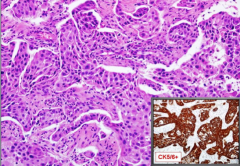
What is this? What type of morphology? |

|
|
|
|
|
|
Triple negative breast cancer is highly _______.
Triple negative breast cancer has higher stage (larger tumor size, more lymph node metastases) and _______grade at presentation.
Triple negative breast cancer more commonly metastases to ____, lung, ____ and distant lymph nodes, and less commonly to _______.
|
|
|
|
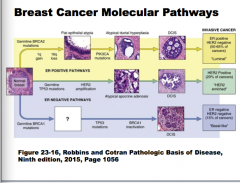
Molecular Subtyping of Breast Cancer
Basal-like type breast cancer has a set of genetic alterations typical for it and this molecular subtype is called “_______”.
Her-2 positive breast cancer (~15%) has a set of genetic alterations typical for it and this molecular subtype is called “Her2”.
Other breast cancers (~70%) have “_________” or “luminal B” molecular subtype. Luminal A subtype is usually ER ______, PR __ or __ and Her-2 _______. Luminal B is complicated. |
|
|
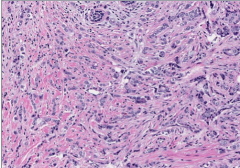
|
What indicates invasion? |
Strong desmoplastic reaction = dense fibrous growth around the tumor. |
|
|
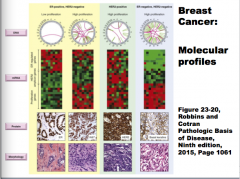
ER+/HER-2 negative HER2-positive ER-negative/HER-2 negative
Comment on the DNA proliferation, mRNA, proteins, and morphology of each. |
|
|
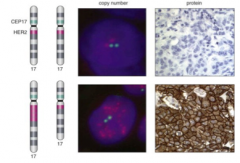
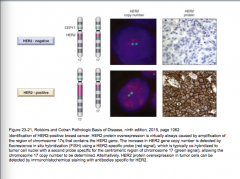
Which is HER-2 negative, which is positive?
What is HER-2 caused by? |
|
|
|
|
|
|
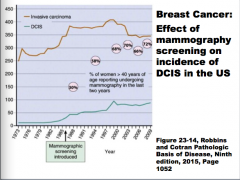
What is the average age of BC diagnosis for whites, hispanics, and for blacks? |
|
|
|
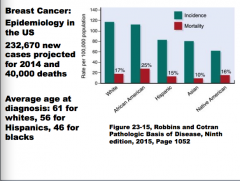
Draw the ER positive pathways and the ER negative pathways. |
|
|
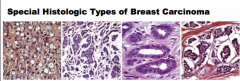
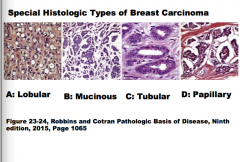
Identify each as tubular, papillary, lobular, or mucinous. |
|
|
Identify each as medullary, secretory, micro papillary, or apocrine. |

|
|
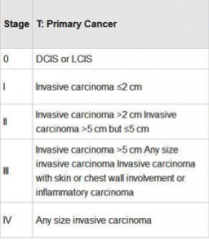
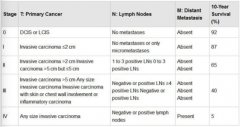
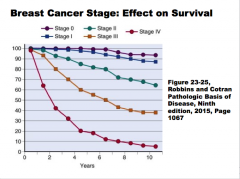
Identify the lymph node involvement with each, distant metastasis involvement, and survival rates. |
|
|
|

|
|
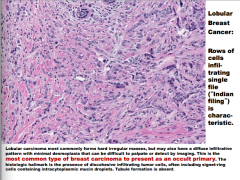
What type of breast cancer? What is the term for the characteristic cell pattern?
What is the most common type of breast carcinoma to present as an occult primary? What is the histologic hallmark? |
|
|
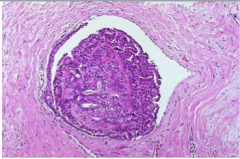
What is a benign epithelial neoplasm growing within a dilated duct composed of multiple branching fibrovascular cores?
What two things are often present? Where are normally situated? Are they normally solitary? Which are commonly multiple and located deeper within the ductal system? |
|
|
|
Over 80% of large duct papillomas produce a nipple _______ ( ______ if the stalk undergoes torsion causing infarction). ______ discharge results from intermittent ______ and release of normal breast secretions or irritation of the duct by the ______. Most small duct papillomas come to clinical attention as small palpable _______, or as densities on mammograms. |
|
|
|
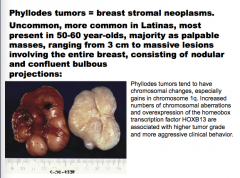
What are breast stromal neoplasms?
Are they common? Distribution? Ages? How does it present in younger women an in older women?
|
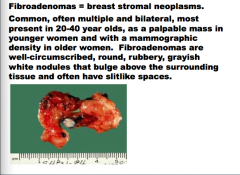
Fibroadenomas |
|
|
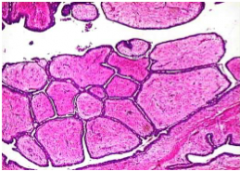
Fibroadenomas have both ____ and _____ components, with delicate, often ____ stroma resembling normal intralobular stroma. The epithelium may be surrounded by ____ or compressed and distorted by it. In older women, the stroma typically becomes densely ______ and the epithelium atrophic. The epithelial component is _____ responsive and there is typically an ______ in size due to lactational changes during pregnancy. |
Fibroadenomas have both stromal and epithelial components, with delicate, often myxoid stroma resembling normal intralobular stroma. The epithelium may be surrounded by stroma or compressed and distorted by it. In older women, the stroma typically becomes densely hyalinized and the epithelium atrophic. The epithelial component is hormonally responsive and there is typically an increase in size due to lactational changes during pregnancy. |
|
Fibroadenomas are grouped with “proliferative changes ______ atypia” in conferring a mildly _______ risk of subsequent cancer, but in one study the increased risk was limited to _______ associated with cysts larger than 0.3 cm, sclerosing _______, epithelial calcifications, or papillary _____ change (“complex fibroadenomas”). |
Fibroadenomas are grouped with “proliferative changes without atypia” in conferring a mildly increased risk of subsequent cancer, but in one study the increased risk was limited to fibroadenomas associated with cysts larger than 0.3 cm, sclerosing adenosis, epithelial calcifications, or papillary apocrine change (“complex fibroadenomas”). |
|
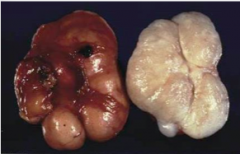
What type of breast stromal neoplasms?
Are they common? More common in what race? Most present in what ages? How do they present?
What chromosomal changes do they often have? Which is often associated with higher tumor grade and more aggressive clinical behavior? |
|
|
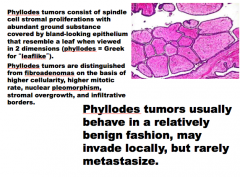
Fibroadenomas are grouped with “proliferative changes _____ atypia” in conferring a mildly ______ risk of subsequent cancer, but in one study the increased risk was limited to ________ associated with cysts larger than 0.3 cm, sclerosing _____, epithelial calcifications, or papillary ______ change (“complex fibroadenomas”).
Phyllodes tumors usually behave in a relatively ______ fashion, may invade locally, but rarely _______. |
|
|
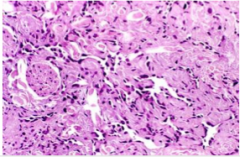
_______ = the only sarcoma that occurs with any frequency in the breast, but it accounts for <0.05% of breast malignancies; it can be _______ or a complication of therapy. Most sporadic angiosarcomas occur in ______ women (mean age ____), are of _____ grade, and have a ____ prognosis. Treatment-related tumors arise _____ to radiation in about 0.3% of women, in breast skin, most cases ___ to ___ years after treatment.
Angiosarcomas have _____ channels lined by large _____ endothelial cells. |
Angiosarcoma = the only sarcoma that occurs with any frequency in the breast, but it accounts for <0.05% of breast malignancies; it can be sporadic or a complication of therapy. Most sporadic angiosarcomas occur in young women (mean age 35), are of high grade, and have a poor prognosis. Treatment-related tumors arise secondary to radiation in about 0.3% of women, in breast skin, most cases 5 to 10 years after treatment.
Angiosarcomas have vascular channels lined by large atypical endothelial cells. |
|
What do pathologists call something that looks very much like adenocarcinoma but isn't.
The number of acini is _____ and they are compressed and ______ in the _____ portion of the lesion. Stromal ______ may completely compress the lumens to create the appearance of solid cords or _____strands of cells lying within dense _____, a histologic pattern that at times closely mimics _____ carcinoma. Sclerosing adenosis can come to attention as a _____ mass, a radiologic density, or calcifications. |
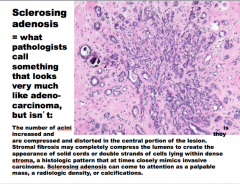
|
|
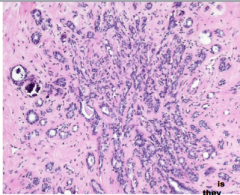
What is this?
The involved terminal duct lobular unit is _____, and the acini are compressed and distorted by ______stroma, with _______ in some of the lumens. Unlike carcinomas, the acini are arranged in a ______ pattern, and the outer border is well circumscribed. |
The involved terminal duct lobular unit is enlarged, and the acini are compressed and distorted by dense stroma, with calcifications in some of the lumens. Unlike carcinomas, the acini are arranged in a swirling pattern, and the outer border is well circumscribed. |
|
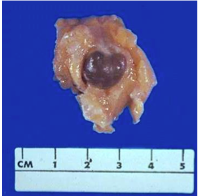
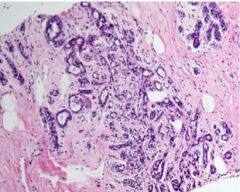
Fibrocystic changes = _____ non-proliferative cysts with associated _____, commonly “_______” breasts on palpation, dense breast with ______ on mammography. Small cysts form by dilation of _____ and may coalesce to form larger cysts. Unopened cysts contain ______, semi-translucent fluid of a ______ or blue color (“blue-dome cysts”). Calcifications are _____ and may be detected by ______. |
|
|
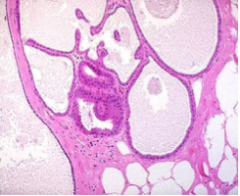
Cysts are lined either by _____ atrophic epithelium or by _______ apocrine cells with abundant _____, eosinophilic cytoplasm and _____ nuclei. The diagnosis is confirmed by the ______ of the mass after fine-needle aspiration of its contents. Cysts frequently ______, releasing _____ material into the adjacent stroma. The resulting chronic inflammation and _____ contribute to the palpable ______ of the breast. |
Cysts are lined either by flattened atrophic epithelium or by metaplastic apocrine cells with abundant granular, eosinophilic cytoplasm and round nuclei. The diagnosis is confirmed by the disappearance of the mass after fine-needle aspiration of its contents. Cysts frequently rupture, releasing secretory material into the adjacent stroma. The resulting chronic inflammation and fibrosis contribute to the palpable nodularity of the breast. |
|
|
Are fibrocystic changes associated with an increased risk of breast cancer? |
NO! |
|
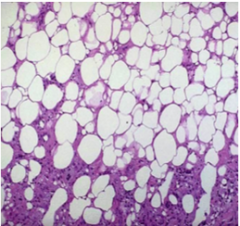
What is this? |
Fat necrosis |
|
|
The presentations of fat necrosis are _____ and can closely mimic cancer: as a _____ palpable mass, skin _______ or retraction, or mammographic densities or ________. |
The presentations of fat necrosis are protean and can closely mimic cancer: as a painless palpable mass, skin thickening or retraction, or mammographic densities or calcifications. |
|
|
Ill-defined, _____ , gray-white nodules containing small _____-white foci are seen grossly. |
Ill-defined, firm, gray-white nodules containing small chalky-white foci are seen grossly. |

