![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
135 Cards in this Set
- Front
- Back
|
What are the structures that comprise the periodontium?
|
gingiva, periodontal ligament, cementum and alveolar bone
|
|
|
What is the function of the gingiva?
|
To provide a seal around the cervical portion of the tooth
|
|
|
What is the function of the periodontal ligament?
|
holds the tissue against the tooth during mastication, suspends and maintains the tooth in it's socket, and surrounds and supports the root.
|
|
|
What is the function of the cementum?
|
holds the tissue against the tooth during mastication, protects the dentin, and surrounds and supports the root.
|
|
|
What is the function of the alveolar bone?
|
Surrounds and supports the root
|
|
|
What structure is part of the periodontium but not part of the attached apperatus?
|
Gingiva
|
|
|
What is considered the most coronal border of the free gingiva?
|
Free gingiva margin
|
|
|
What structures comprise the attachment apparatus?
|
Periodontal tissues involved in the attachment and support of the root in the tooth socket, specifically the periodontal ligament, cementum and alveolar bone
|
|
|
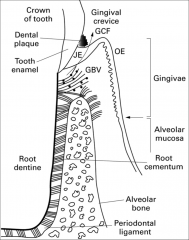
What is the free gingiva?
|
Gingival margin that surrounds the tooth. It is unattached, acts like a turtle neck, has a space for bacteria to hide, has gingival crevicular fluid (GCF), should be 0.5 - 3 mm of depth in health, floss can clean out area.
|
|
|
What will the free gingiva look like in health?
|
Light pink, knife edged or scalloped, 0.5 - 3 mm coronal to CEJ, could be blunted if overaggressive use of an interdental aid
|
|
|
What will the free gingiva look like in disease?
|
Edematous (inflamed) and erythematous (red)
|
|
|
Will the sulcus ever be bordered by attached gingiva?
|
No
|
|
|
Will you ever have a probing depth of "0"?
|
No
|
|
|
What two tissues form the border of the gingival crevice (sulcus)?
|
Tooth and free gingiva, the sulcus is a gap
|
|
|
What are the boundaries of the free gingiva?
|
Coronally the free gingival margin and apically the free gingival groove and laterally the gingival crevice and the tooth
|
|
|
What happens to the free gingiva if there is an open contact?
|
It will be blunted
|
|
|
What type of epithelium is free gingiva?
|
Nonkeratinized stratified squamous over lamina propria
|
|
|
What is the gingival crevice termed in health? Inflamed?
|
Health: sulcus
Inflamed: pocket |
|
|
Where does the sulcus receive its blood supply?
|
Lamina propia (connective tissue)
|
|
|
Where does the gingival crevicular fluid originate?
|
From the blood vessels within the underlying connective tissue (lamina propria)
|
|
|
What do you see in health vs disease with the gingival crevicular fluid?
|
Flow is minimal to absent in health, but increases due to inflammation from accumulation of plaque in the gingival crevice.
|
|
|
What is a pro of the gingival crevicular fluid?
|
Cleanses the sulcus
|
|
|
What are the cons of the gingival crevicular fluid?
|
It is a source of nutrients for subgingival bacteria and supports subgingival calculus formation.
|
|
|
What is another name for the connective tissue layer beneath the oral epithelium?
|
Lamina propria
|
|
|
Is the presence or absence of free gingival groove an indicator of health or disease? And what is it?
|
No. It is a shallow depression on the outer surface of the gingiva, is about 1 - 2 mm apical from the margin of the gingiva and slightly apical to the level of the CEJ. This groove separates the free gingiva from the attached gingiva. Present in about 30 - 40% of adults.
|
|
|
In which layer do you find the melanin layer?
|
The epithelial layer
|
|
|
What is attached gingiva?
|
It is continuous with the free gingiva and is firmly attached to the underlying cementum and periosteum (connective tissue) covering the alveolar process.
|
|
|
What is the mucogingival junction (MGJ)?
|
It joins the attached gingiva to the alveolar mucosa except on the palate because the attached gingival runs into the palatal mucosa. It is well-defined in some but not in others and is not a sign of health or disease.
|
|
|
Where is the widest zone of attached gingiva? Narrowest zone?
|
Widest: Incisor and molar
Narrowest: Premolar |
|
|
Do you measure on the palate?
|
No because it is palatal mucosa
|
|
|
How would you describe attached gingiva?
|
Firmly bound, usually keratinized, normally coral/salmon pink, sometimes stippled, can vary in degrees of brownish-black color (melanin pigmentation) depending on ethnic variation
|
|
|
What is melanin pigmentation?
|
Varying degrees of brownish-black color depending on ethnic variation. Will be generalized. Caused by melanocytes with are in the basement membrane.
|
|
|
What is stippled gingiva?
|
Outer surface of attached gingiva has an appearance similar to an orange peel with shallow depression between elevations. The free gingiva has a smooth surface.
|
|
|
When is stippling present?
|
In health or disease. The absence of stippling does not necessarily indicate the presence of disease. Only present in about 40% of adults (mainly men). However the presence of inflammation with the loss of stippling can be considered party of the disease process, assuming stippling was present initially.
|
|
|
Stippling is cause by....
|
...junction of epithelial ridges and connective tissue papillae.
|
|
|
Does all attached gingiva have the same consistency?
|
No, there are variations in consistency. When it is thiner it is more likely to get recession.
|
|
|
What are the variations in width of the attached gingiva?
|

1 - 9 mm. Avg: 3.5 - 4.5 in max and 3.3 - 3.9 mm in mand.
A has lots of attached gingiva while C has very minimal attached gingiva (make sure your pt is aware they don't have much attached tissue.) |
|
|
What is effected with periodontal disease?
|
The periodontium
|
|
|
What is the interdental gingiva (interdental papillae)?
|
Consists of facial and lingual papillae, lateral borders and tip are free gingiva
|
|
|
What is the col?
|
Apical to the contact interproximally, concave facial to lingual, nonkeratinized (which is effected with bacteria more then keratinized), and not present if no in contact or if there has been recession involving interproximal area
|
|
|
Do anterior teeth have a col? Where a diastema is present?
|
Ant. teeth have a col, but there is no call when a diastema is present.
|
|
|
What is alveolar mucosa?
|
Nonkeratinized stratified squamous epithelium, loose/freely moveable, highly vascular, mainly elastic fibers, continuous with labial, buccal and lingual mucosas.
|
|
|
Is the alveolar mucosa part of the periodontium?
|
No, but it is an important periodontal structure. It extends from the MGJ to the mucous membrane of the cheek, lip, and floor of mouth.
|
|
|
What is the masticatory mucosa?
|
Located on the hard palate, keratinized straified squamous epithelium, light shade of pink then alveolar due to not seeing the vascularity as much.
|
|
|
What are frenum attachments?
|
Folds in the alveolar mucosa
|
|
|
What does the gingival epithelium consist of?
|
1. Oral epithelium (OE)
2. Sulcular or crevicular epithelium (SE) 3. Junctional epithelium (JE) |
|
|
What is the function of the gingival epithelium?
|
Protect underlying surface, allows selective interchange with oral cavity (such as chewing tobacco, nitro glycerine tablets that are placed sublingual)
|
|
|
Is the gingival epithelium vascular or avascular?
|
Avascular (no blood supply), it relies upon the underlying lamina propria for it's blood supply and nutrients.
|
|
|
Name the layers of the oral epithelium starting with the deepest.
|
It is stratified squamous with stratum basale or stratum germinativum (basal cell layer, deepest layer next to the lamina propria), Stratum spinosum (spinous cell layer), Stratum granulosum (granular layer), Stratum corneum (keratinized/cornified cell layer. this outermost layer serves as a barrier membrane protecting the underlying periodontal tissues from invasion by foreign substances)
|
|
|
Explain cellular renewal of the oral epithelium?
|
It achieves renewal by producing a pool of cells that migrate from the basal layer to the oral environment, which is a process called keratinization (when the cells mature.) Turnover time is different for different types of epithelium. It begins in the basal layer moving the "older" basal cells to the spinous layer where they become keratinocytes, once they reach the outer epithelial layer they are shed in the oral cavity.
|
|
|
What do keratinocytes produce?
|
keratin
|
|
|
Why is keratinization important to oral tissues?
|
Because it contributes to the mechanical toughness of the oral surface of the epithelium.
|
|
|
How many days is the oral epithelial turnover time?
|
Approximately 10 days, while skin is 28 days and the JE is 4 - 7 days
|
|
|
What cells are present in the oral epithelium?
|
Keratinocytes, nonkeratinocytes, melanocytes, langerhans cells, merkel cells, and inflammatory cells.
|
|
|
What cells make up the majority of cellular structure and what are they responsible for?
|
keratinocytes, responsible for the salmon pink color of gingiva
|
|
|
What two cells are located in the (stratum basale) basal cell layer and what do they secrete/associated with?
|
Melanocytes and secrete melanin and merkel cells which are associated with nerve response.
|
|
|
Where are the Langerhans cells located and what what are they involved in?
|
Located in the stratum spinosum and are involved in the early defense mechanism of the gingiva.
|
|
|
What is the major inflammatory cell?
|
Polymorphonuclear leukocytes (PMNs)
|
|
|
Where is the sulcular epithelium and what are it's major characteristics?
|
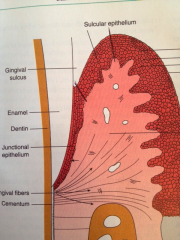
It lines the gingival sulcus to the coronal edge of JE, nonkeratinized, somewhat permeable, contains gingival crevicular fluid, and in health will have a very slight wavy junction
|
|
|
Where is the junctional epithelium (JE) and what are it's major characteristics?
|
Located at the base of the sulcus, nonkeratinized, no wavy junction (smooth, no rete ridges), joined to tooth by epithelial attachment, has the most rapid turnover rate of all oral epithelial tissues (usually <l one week)
|
|
|
Length of the JE?
|
0.71 - 1.35 mm in length
|
|
|
How many zones are there of the JE and what are the cell variations of each?
|
3 zones: 1. Apical - fewer cells 2. Middle 3. Coronal - more cells/more permeable
|
|
|
Are PMN's present in the JE?
|
Yes, in health small numbers are transiently seen
|
|
|
Which part of the epithelium is considered the most permeable?
|
Junctional epithelium
|
|
|
The term stratified refers to?
|
Several layers thick
|
|
|
Which structure has the most elastic fibers?
|
Alveolar mucosa because elastic fibers make it more moveable
|
|
|
Which epithelial layer has the fastest turnover rate?
|
Oral epithelium
|
|
|
What causes the wavy junction where the epithelium and connective tissue meet?
|
Epithelial ridges (rete pegs) and connective tissue papillae
|
|
|
What is the purpose of the wavy junction and what does it look like on the surface?
|
It will be evident on the surface of the gingiva by creating a stippled appearance. The main purposes are to increase the surface area and to get nutrients to the epithelium.
|
|
|
What is the purpose of connective tissue papillae and epithelial ridges?
|
Strength (bond) and blood and nutrient supply
|
|
|
What is the gingival connective tissue made of?
|
60% collagen (Type I 95% and Type III)
40% ground substance (food supply, proteoglycans, glycosaminoglycans, nerves, blood vessels, provides pathway for nutrients and water) |
|
|
What cells make up the connective tissue?
|
Fibroblasts (most prominent/have to have to produce collagen, synthesize ground substance, collagen and collagenase which destroys collagen), Macrophages, mast cells, plasma cells, lymphocytes, and PMN's
|
|
|
Name the primary gingival fibers
|
Circular, dentongingival, dentoperiosteal, alveologingival, and transspetal
|
|
|
Name the secondary gingival fibers
|
Periostogingingival, interpapillary, transgingival, intercrevicular, semicircular, and intergingival
|
|
|
What is the role of gingival fibers?
|
To support and give contour to the free and attached gingivae and firmly connect the attached gingiva to the underlying cementum and alveolar bone. They are arranged in such a way they maintain the gingiva against the tooth and bone.
|
|
|
Enamel is what type of tissue?
|
Epithelial
|
|
|
Gingival fibers are?
|
Collagen fibers
|
|
|
What is the dentogingival unit?
|
Collective refers to the epithelial attachment and the gingival connective tissue attachment (gingival fibers) to the cementum. This is what stabilizes the gingival tissue to the tooth.
|
|
|
Define biologic width
|
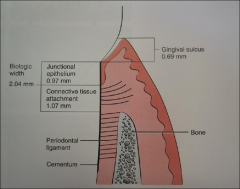
The combined height of the gingival connective tissue (1.07 mm) and the junctional epithelium (0.97 mm) present around teeth
|
|
|
What is the biologic widths relevance to restorative materials and periodontal inflammation?
|
Is important when evaluating a tooth for a crown. There must be an adequate amount of biologic width (soft tissue attachment) for periodontal health. If the margin of a crown violates the biologic width then there will be constant inflammation around the crown.
|
|
|
What do epithelial cell junctions do?
|
Help cells function as a unit
|
|
|
Types of junctions and what do they do?
|
Desmosome: Attachment between epithelial cells
Hemidesmosome: Attachment between epithelial cell and basal lamina *Help to remember: roller coaster - Tracks: basal lamina, Wheels: hemidesomosomes, Cart: desmosomes* |
|
|
Junctional epithelium has ____x fewer desmosomes then oral epithelium, which does what?
|
4x fewer, so the intercellar space is wider
*Help to remember: It's like a coat with buttons (desmosomes) that has gaps between the buttons, the more the desmosomes the less can get in* |
|
|
What does the basal lamina do? And what are it's 2 parts?
|
It separates the JE from connective tissue. The 2 parts are the lamina lucida (near epithelium) and lamina densa (near connective tissue)
|
|
|
What are the basal lamina and the hemidesomosomes referred to as? What does it do?
|
The epithelial attachment, it provides the the attachment of the JE to the tooth surface
|
|
|
What is the periodontal ligament (PDL)? Average width?
|
The connective tissue that extends from the cementum covering the root surface to the alveolar bone, 0.25 mm
|
|
|
Functions of the PDL?
|
Suspensory, shock absorption, remodeling, formative, sensory, and proprioceptive pg 17 (Support and anchor the teeth within the alveolar process along with the cementum and alveolar and supporting bone)
|
|
|
Name the components of the PDL
|
Collagen fibers are the #1 component, attached to alveolar bone and cementum via Sharpey's fibers, and has interstitial space, cells, extracellular matrix, blood vessels and nerves.
|
|
|
What is in the interstitial space?
|
Blood vessels, nerves, lymphatics and cells
|
|
|
The collagen turnover is __________ in the PDL then in bone or gingiva
|
Faster
|
|
|
Cells in the PDL are?
|
Fibroblasts (highest), then osteoblasts, cementoblasts, osteroclasts, epithelial and nerve
|
|
|
Name all 5 PDL fibers
|
Alveolar crest, horizontal, oblique, apical, and interradicular
|
|
|
Alveolar crest (where and what)
|
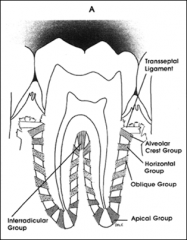
- Cervical cementum to alveolar crest
- Resists lateral motion |
|
|
Horizontal (where and what)
|
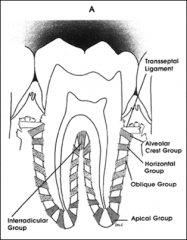
- Apical to ACF
- Cementum to bone - Resists lateral forces |
|
|
Oblique (where and what)
|
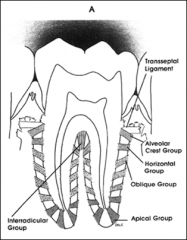
- Apical to above
- Cementum to bone - Most abundant - Absorbs occlusal forces |
|
|
Apical (where and what)
|
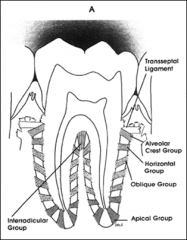
- Apex to bone
- Resists tooth being lifted from it's socket |
|
|
Interradicular (where and what)
|
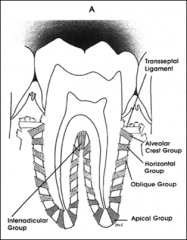
- Furcation to bone
- Only on multi-rooted teeth - Stablization |
|
|
Which part of the PDL fiber is considered to be the most abundant?
|
Oblique
|
|
|
Which part of the basal lamina is connected to the connective tissue?
|
Lamina densa
*Help: dense is deeper* |
|
|
A radiographically widened PDL could mean?
|
Increases occlusal forces placed on the tooth (narrow PDL is hypofunction, widened PDL is hyerfunction)
|
|
|
In health, the JE has a wavy connective tissue/epithelial interface?
|
False, there is a smooth interface in health
|
|
|
Biologic width is?
|
Base (JE) of the sulcus to height of the crestal bone
|
|
|
Rests of Malassez could possibly play a role in what?
|
The development of cysts, it is unknown what rests of malassez are there for
|
|
|
Loss of attachment means?
|
Periodontal ligament fibers have been destroyed.
|
|
|
Is there a loss of attachment with gingivitis?
|
No
|
|
|
In health, the EA/JE is...
|
...at or near the CEJ
|
|
|
In health, the gingival margin is...
|
...above the CEJ or at or near the CEJ (normally 2 mm deep)
|
|
|
In gingivitis, the EA/JE is....
|
...at or near the CEJ
|
|
|
In gingivitis, the gingival margin is....
|
...above the CEJ from the inflammation
|
|
|
In periodontitis, the EA/JE is...
|
...below the CEJ due to the loss of attachment
|
|
|
In periodontitis, the gingival margin...
|
...deepens
|
|
|
In recession, the EA/JE is...
|
...below the CEJ
|
|
|
In recession, the gingival margin is...
|
...apical to the CEJ
|
|
|
Is recession considered a disease process?
|
No, it is caused by trauma. There is attachment loss by root surface exposure
|
|
|
Primary function of cementum?
|
To attach the principal fibers to the root surface
|
|
|
Cementum is a product of....
|
...PDL
|
|
|
How does cementum form?
|
In layers or increments, cementoid is the initial layer and is not calcified, when it becomes 80-90% calcified a new layer of cementoid is made
|
|
|
True or False
Cementoid resists resorption |
True, when bone remodeling occurs via ortho it requires cementum to resist root resorption
|
|
|
Components of cementum
|
Somewhat permeable (some toxins can permeate the surface), avascular, and no nerve endings (only sensitive because of the hydrodynamic theory)
|
|
|
Relationship of cementum and enamel
|
- Cementum overlaps enamel 60%
- Meet 30% - Gap 10% (clinically this means to be careful when scaling) |
|
|
Explain acellular cementum
|
- No cementocytes
- Coronal 2/3 - 1/2 - 0.1 mm thick - 1st formed - Sharpey's fibers (more abundant) - Will not regenerate |
|
|
Explain Cellular cementum
|
- Cementocytes
- Apical 1/3 - Forms after tooth has erupted - Less calcified - Thickness increases with age (enamel is wearing down, therefore your body compensates by producing more cementum) - 0.5 mm thick |
|
|
The alveolar process constitutes? What are the parts of the alveolar process?
|
The part of maxilla and mandible that forms and supports the sockets or alveoli of teeth. 2 parts: alveolar bone proper (cribiform plate) and supporting bone
|
|
|
Explain Alveolar Bone Proper (cribiform plate)
|
- Hard, compact bone with openings that allow for passage of blood, nerves, and lymphatic
- Lamina dura (radiographicly) - Bundle bone (where Sharpey's fibers terminate) |
|
|
Explain Supporting Bone
|
2 parts
- Compact bone - Cancellous bone (trabecular) |
|
|
Where is the cortical plate thickest?
|
Mandible, thickest on the buccal area of the premolar and molar areas and thinnest in the incisor area
|
|
|
Where is the compact bone the thickest on the maxilla?
|
On the palatal than on the buccal surfaces
|
|
|
What is the bone called that forms the contour of bone? And what is it a good indicator of?
|
Interproximal, aka interdental septum
- contour is a good indicator of periodontal health - angular contour doesn't always mean periodontal disease |
|
|
Can you numb one side of the face ad not the other?
|
Yes, because the trigeminal nerve is split
|
|
|
How does the lymphatic drainage flow?
|
It follows the blood supply, primary drainage is the submandibular nodes
|
|
|
What are the changes occur with age to the periodontium?
|
- Gingiva thins with reduced keratinization
- Decrease in the number of cells in the lamina propria - Cementum increases in thickness - Cells within the periodontal ligament decrease in number - Attrition on the proximal surfaces of teeth causing teeth to migrate in a mesial direction (causes alveolar bone changes) |
|
|
True or False: The gingival fibers assist in anchoring the cementum to the alveolar bone?
|
False, periodontal ligament
|
|
|
Which is considered to be the attachment between 2 epithelial cells?
|
Desmosomes
|
|
|
What is the approximate length of the JE?
|
0.97 mm pg 60
|
|
|
The max compact bone is usually thicker on the?
|
Palatal surface
|

