![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
79 Cards in this Set
- Front
- Back
|
Blood pH volume and components |
pH 7.35-7.45 5-6 liters (7-8% of BW) Plasma (55% of blood) Formed elements (45% of blood) |
|
|
Plasma is mostly_ contains __ and __ |
Mostly water (92%) Dissolved solutes Plasma protiens |
|
|
Dissolved solutes in plasma |
Electrolytes Nutrients Gases Hormones Waste Etc |
|
|
Plasma protiens are made in the __ and diffusibility |
Non-diffusible Made in liver |
|
|
Four types of plasma protiens |
Albumin Alpha and beta globulins Gamma globulins Fibrinogen |
|
|
Albumin |
Most abundant plasma protien Maintains colloid Osmotic pressure of the blood (blood volume and BP) Transports Ca2+ and bilirubin |
|
|
Alpha and Beta globulins |
Transport non-polar substances in plasma Alpha transports steroids and other lipids Beta transports iron |
|
|
Gamma globulins |
Antibodies made by plasma cells |
|
|
Fibrinogen |
Forms fibrin mesh found in blood clots |
|
|
Formed elements |
Erythrocytes Leukocytes Platelets |
|
|
Erythrocytes ratio of whole blood, functions, contain, main energy path |
5million/mm3 whole blood Transport oxygen and carbon dioxide and to buffer blood Contain no organelles, mitochondria, or ribosomes Anaerobic |
|
|
Leukocytes ratio of whole blood + 2 types |
5-10,000/mm3 Granulocytes and agranulocytes |
|
|
Granulocytes are ____ and contain ___ and ___ + types |
Motile, move by amoeboid action Contain mitochondria and organelles
Neutrophils Eosinophils Basophils |
|
|
Agranulocytes |
Lymphocytes Monocytes |
|
|
Lymphocytes make up __% of WBC in circulation and are ___ cell types |
20-30 B and T cell types |
|
|
Monocytes % WBC |
3-9 |
|
|
Platelets ratio whole blood + reserves + role |
250,000-450,000/mm3 Additional 1/3 found as reserve in spleen Important role in blood clotting |
|
|
Neutrophils % WBC inflammation involvement and lifespan |
60-70 Acute inflammation Short life hours-few days |
|
|
Hemoglobin |
RBC are just packets of hemoglobin Heme- four per hemoglobin, each contain one iron Globin- protien portion |
|
|
Erythropoiesis |
Formation of RBC |
|
|
Erythropoietin secreted by in response to + effect |
Secreted by kidneys in response to hypoxia Increases rate of erythropoiesis |
|
|
RBC form from |
Hematopoietic stem cells in the red bone marrow |
|
|
Fetal hemoglobin |
Contain 2 alpha and 2 gamma globins Has a higher affinity for oxygen than adult hemoglobin |
|
|
Hemoglobin A |
Major type in adults Contains 2 alpha and 2 beta globins |
|
|
Erythropoiesis requires |
B12 Folate B6 Riboflavin Panthothenic acid Niacin Ascorbic acid Vitamin E Etc |
|
|
Reticulocytes are + time + contains |
Immature RBC in circulation Matures into RBC 24-48Hr after realease in circulation Still has ribosomes and mitochondria so it can still make hemoglobin |
|
|
RBC lifespan +removed by |
120 days Macrophages located in liver and spleen |
|
|
RBC recycling |
Hemoglobin is for the main part recycled; Globin- broken down into amino acids Iron is removed from heme and recycled Porphyrin of heme>billrubin> moved to liver> conjugated> bile > urobilinogen > urine and stool |
|
|
Jaundice |
Yellow coloration ^ levels bilirubin |
|
|
Causes of jaundice (4) |
Excess deconstruction of RBC Impaired uptake of bilirubin by liver Decreased conjunction of billrubin Obstruction of bile flow |
|
|
Unconjugated billrubin is ___ because __ |
Toxic It is lipid soluable and can therefore cross cell membranes |
|
|
Oxygen transport: of the O2 that diffuses from the alveoli into the blood of pulmonary capillaries; __% does __ and __% does __ |
97% combines with iron in hemoglobin 3% dissolves in plasma |
|
|
Deoxyhemoglobin |
O2 loads or unloads with hemoglobin due to PO2 gradient Oxygen diffuses from high to low |
|
|
Oxygen saturation |
Amount of hemoglobin bound to oxygen is relative to total hemoglobin Normally Sao2 is 95-100% Normally Svo2 is 60-80% |
|
|
Oxygen/Hb dissociation curve |
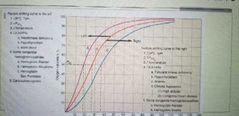
At a given partial pressure of oxygen, what percentage of your hemoglobin will be oxyhemoglobin |
|
|
Oxygen Hb affinity |
An increase in affinity hemoglobin has for oxygen shifts curve to left A decrease in affinity hemoglobin has for oxygen shifts curve to right |
|
|
Increase affinity means +fetal |
At a given Po2 there will be a higher Saturation Fetal Hb has higher affinity for O2 than maternal, left shift, oxygen tends to go from maternal Hb to Fetal Hb |
|
|
Increase in affinity caused by (6) |
1. Decrease H+, increase pH 2. Decrease Pco2 3. Decrease temp 4. Decrease 2,3-DPG 5. Some congenital hemoglobinopathies 6. Carboxyhemoglobin |
|
|
Decrease in 2,3 deficiency caused by |
Hexokinase deficiency Hypothyroidism Bank blood |
|
|
Congenital hemoglobinopathies that cause Increase affinity |
Hemoglobin Rainier Hemoglobin Hiroshima Hemoglobin San Francisco |
|
|
Decrease in affinity means |
At a given Po2 there will be a lower percent saturation |
|
|
Factors that cause decrease affinity (5) |
1. Increase H+, decrease pH 2. Increase Pco2 3. Increase temp 4. Increase 2,3-DPG 5. Some congenital hemoglobinopathies |
|
|
Increase 2,3-DGP caused by (4) |
Pyruvate kidney disease Hyperthyroidism Anemia Chronic hypoxia |
|
|
Congenital hemoglobinopathies that cause decrease in affinity |
Hemoglobin Kansas Hemoglobin Seattle |
|
|
Three dorms CO2 is transported in blood |
Plasma (5%) Carbaminohemoglobin (20%) HbCO2 Bicarbonate ion (75%) HCO3- in plasma |
|
|
In carbaminohemoglobin co2 binds to |
Globin portion of hemoglobin |
|
|
Bicarbonate ion reaction is catalyzed by |
Anhydrase found in RBC |
|
|
The extra H+ ion from bicarbonate ion reaction binds with __ forming __. Therefore ___ serves as ___ |
Hb Reduced hemoglobin (HHb) Hemoglobin serves as pH buffer |
|
|
Chloride shifts occur when |
Cl- ion moves into or out of RBC to maintain electrical neutrality as HCO3- diffuses in or out |
|
|
Anemia is __, due to __ or __, can cause __ |
Decreased oxygen carrying capacity Decrease in RBC or Hb Can cause tissue hypoxia |
|
|
4 types of anemia due to decrease in RBC production |
1. Aplastic anemia 2. Chronic renal failure 3. Pernicious anemia 4. Iron deficiency |
|
|
Etiology pathogenesis if aplastic anemia (5) |
°stem cell disorder °due to reduction of hematopoietic tissue in bone marrow °caused by toxins, radiation, immunologic injury to bone marrow °causes pancytopenia °chloramphenicol, benzene have history of causing this |
|
|
Pancytopenia |
Decrease in all types of blood cells |
|
|
Tx of Aplastic Anemia (3) |
Withdraw causative agent Support care, transfusion Drugs to stimulate bone marrow or marrow transplant |
|
|
Chronic renal failure etiology and pathogenesis (2) |
°Due primarily from decreased erythropoietin production from kidney °failure of renal excretion and elevation of waste products in blood contributes by causing hemolysis and bone marrow depression |
|
|
Tx chronic renal failure (3) |
°Synthetic erythropoietin °provide necessary elements for RBC production °dialysis and transfusions |
|
|
Pericious anemia etiology and pathogenesis (5) |
°lack of intrinsic factor from stomach parietal cells which causes inability to absorb vitamin B12 °causes abnormal DNA synthesis in bone marrow cells °low RBC, WBC, platelet counts but not as much as Aplastic Anemia °macrocytic anemia (large RBC) °Folate deficiency causes a similar condition |
|
|
Tx pericious anemia |
Replacement of vitamin B12 or folate |
|
|
Iron deficiency etiology and pathogenesis (7) |
°most common nutritional deficiency in the world °most common cause of anemia °lron not available to make adequate amounts of Hb °lack of iron due to low intake, impaired absorption, increased requirements such as pregnancy, excessive iron loss due to chronic hemorrhage °causes hypochromic, microcytic anemia °most are asymptomatic °may be weak with fatigue |
|
|
Tx iron deficiency |
Iron in diet |
|
|
Anemia due to inherited disorders (3) |
Thalassemia sickle cell anemia Hereditary Spherocytosis |
|
|
Thalassemia etiology and pathogenesis (6) |
°Group of diseases caused by mutant genes that suppress the synthesis of globin chains in Hb °autosomal recessive genetic disorder °caused by an imbalance of alpha and beta globin that leads to an overall decrease in Hb ° the normal globins accumulate in cytoplasm and precipitate in RBC, the RBC becomes more fragile, which causes a decreased survival rate of RBC (type of hemolytic anemia) °some live to adult, some rarely past teens or 20s |
|
|
Tx thalassemia |
Transfusions, bone marrow transplants |
|
|
Sickle cell anemia etiology (8) |
°Genetically caused defect in hemoglobin synthesis °most common heritable hematologic disease in the world °under low oxygen situations the abnormal Hb polymerizes causing RBC to form sickle shape °sickle cells have a decreased survival causing anemia °sickle cells also cause vascular occlusions °homozygous for sickle cell produces only abnormal type hemoglobin and the full blown sickle cell anemia °hsterozygous produce both normal and abnormal types of hemoglobin- a selective force for this gene was malaria °higher incidents of sickle cell Anemia in African-Americans |
|
|
Treatment for Sickle cell Anemia |
Stem cell transplant, supportive, transfusions |
|
|
Hereditary Spherocytosis etiology and pathogenesis |
RBC have abnormal cytoskeleton attached to cell membranes °cells form sphere (ball) shape which decreases their survival time °autosomal dominant disorder °mosy common hereditary hemolytic anemia of European descent |
|
|
Tx hereditary Spherocytosis |
Splenectomy decreases destruction of RBC by Macrophages in the spleen |
|
|
Anemia due to extrinsic RBC destruction or loss (hemolytic) |
Hemolytic disease of newborns Acute blood loss |
|
|
Hemolytic disease of newborns (HDNB) etiology |
°Rh or ABO incompatibility °ABO incompatibility is most common cause but Rh incompatibility is most important clinical because of the severity of the hemolysis in newborn °when fetal RBC cross placenta at the time of birth, they may stimulate the production of maternal Abs some of which may be able to cross the placenta and destroy the fetal RBC °Rh neg mother with Rh pos. Child °second child most vulnerable °causes hemolysis and jaundice in child |
|
|
Tx hemolytic disease of newborns |
Prevention with RhoGAM shot Contains antibodies that attach to Rh Antigens. Destroy fetal blood cells before they can cause the mothers immune system to recognize the Rh blood cells and prevent her from producing her own anti-Rh antibodies |
|
|
Acute blood loss etiology |
Trauma or secondary to some other diseases |
|
|
Acute blood loss Tx |
Blood volume replacement |
|
|
Relative anemia is |
Normal total RBC amount but with excess plasma fluid |
|
|
Dilutional anemia during pregnancy |
°Average plasma volume increases over 40% during pregnancy but RBC don't Increase proportionally °Hematocrit will be low due to excess plasma not from decreased RBCs °Hematocrit is the % of blood composed of RBC |
|
|
Polythemia is |
Increased RBCs Increased blood viscosity which leads to hypertension |
|
|
Types of polycythemia |
Polycythemia Vera Secondary polycythemia Relative polycythemia |
|
|
Polycythemia Vera |
°overproduction of all blood cells but problems caused by too many RBC °usually symptoms appear around 60y. More common in males °no cure °try to reduce blood volume and viscocity by phlebotomy |
|
|
Secondary polycythemia |
Increase RBC due to increased stimulation of erythropoiesis such as in high altitudes |
|
|
Relative polycythemia |
Increased Hematocrit although normal or decreased RBC Can occur with severe dehydration -Hematocrit high because there is less plasma |

