![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
43 Cards in this Set
- Front
- Back
|
What does it mean to be a "don't touch" lesion?
|
Skeletal “don’t touch” lesions are those processes that are so radiographically characteristic that a biopsy or additional diagnostic tests are unnecessary. Not only does the biopsy result in unnecessary morbidity and cost, but in some instances, as discussed in this chapter, a biopsy can also be frankly misleading and lead to additional unnecessary surgery.
|
|
|
Why can myositis ossificans and avulsion injuries look like sarcoma on path?
|
Any area undergoing healing can have a high nuclear-to-chromatin ratio and a high mitotic figure count, thereby occasionally simulating a malignancy histologically.
|
|
|
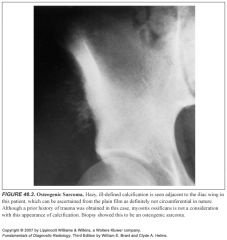
What does myositis ossificans look like on imaging? How can you tell it apart from a sarcoma?
|
-The typical radiologic appearance of myositis ossificans is circumferential calcification with a lucent center.
-This is often best appreciated on a CT scan. -A malignant tumor that mimics myositis ossificans has an ill-defined periphery and a calcified or ossific center. -Periosteal reaction can be seen with myositis ossificans or with a tumor. -Occasionally, the peripheral calcification of myositis ossificans can be too faint to appreciate; in these cases, a CT scan should help, or delayed films 1 or 2 weeks later are recommended. -Biopsy should be avoided when myositis ossificans is a clinical consideration. -MR can be misleading because the peripheral calcification is not as well seen, and edema in the soft tissues can extend beyond the calcific rim |
|
|
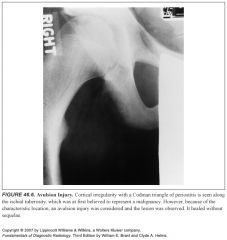
What does an avulsion injury look like on imaging? How can you tell it apart from a sarcoma?
|
-These injuries can have an aggressive radiographic appearance, but because of their characteristic location at ligament and tendon insertion sites (e.g., anteroinferior iliac spine or ischial tuberosity), they should be recognized as benign.
-As with myositis ossificans, delayed films of several weeks will usually allow the problem case to become more radiographically clear. -Biopsy can lead to the mistaken diagnosis of a sarcoma and should therefore be avoided. |
|
|
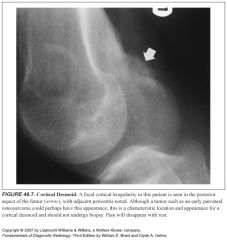
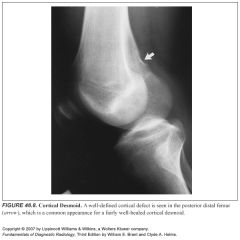
What is a cortical desmoid? What does it look like on imaging (including nucs)?
|
-Cortical desmoid is a process on the posteromedial supracondylar ridge of the distal femur that is considered by many to be the result of an avulsion of the adductor magnus muscle.
-It occasionally simulates an aggressive lesion radiographically and histologically -They might or might not be associated with pain and can have increased radionuclide uptake on a bone scan. -They might or might not exhibit periosteal new bone and usually occur in young people. -Painful cortical desmoids should become asymptomatic with rest. -They are often seen as an incidental finding on MR of the knee and have a characteristic appearance |
|
|
What's the name of the lesion of the posteromedial supracondylar ridge of the distal femur?
|
Cortical desmoid
|
|
|
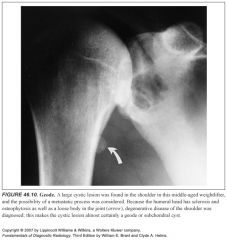
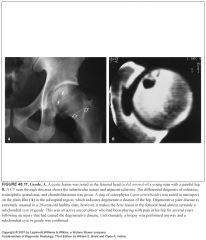
What should you think of if you see a cystic lesion near a joint with degenerative disease?
|
Subchondral cyst
Subchondral cysts can also occur in the setting of calcium pyrophosphate dihydrate crystal disease, rheumatoid arthritis, and avascular necrosis |
|
|
What characteristics of a vertebral body lesion would make you confident that it is degenerative in origin?
|
-Discogenic vertebral disease most often is sclerotic and focal.
-It is always adjacent to the endplate, and the associated disk space should be narrow. -Osteophytosis is invariably present. -It really is a variant of a Schmorl node and should not be confused with a metastatic focus. -On occasion it can be lytic or even mixed lytic-sclerotic. -Old films often confirm the benign nature of this process. |
|
|
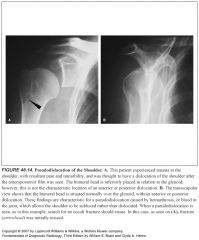
Describe pseudosubluxation of the humerus:
|
-This results from a fracture with hemarthrosis, which causes distension of the joint and migration of the humeral head inferiorly.
-An axial or transscapular view shows it is not anteriorly or posteriorly dislocated (the usual forms of shoulder dislocation) but merely inferiorly subluxated. -On an anteroposterior view, it can mimic a posterior dislocation in that the normal superimposition of the humeral head and the glenoid is missing. -If necessary, the joint can be aspirated to confirm the presence of a bloody effusion and to show the normal position of the humeral head when fluid has been removed from the joint. |
|
|
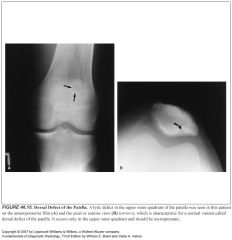
Describe the dorsal defect of the patella:
What does it look like on plain films and MR? |
-It is a normal developmental anomaly, however, and because of its characteristic location, it should not undergo biopsy.
-A lytic defect in the upper outer quadrant called a dorsal defect of the patella -On MR, it will have an appearance similar to that of many other bony lesions—that is, low signal on T1WIs and high signal on T2WIs |
|
|
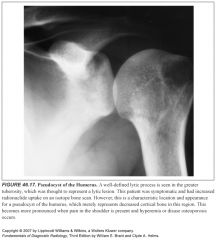
What is a pseudocyst of the humerus?
What does it look like on imaging (including nucs)? |
-This is merely an anatomic variant caused by increased cancellous bone in the region of the greater tuberosity of the humerus, giving this region a more lucent appearance on radiographs.
-With hyperemia and disuse caused by rotator cuff problems or any other shoulder disorder, this area of lucency may appear strikingly more lucent and mimic a lytic lesion. -Because of the associated hyperemia from the shoulder disorder (be it rotator cuff injury or another condition), a bone scan can show increased radionuclide uptake -Although other lesions, such as a chondroblastoma, an infection, or even a metastatic focus, could occur in a similar location, they do not have quite the same appearance as a pseudocyst of the humerus. |
|
|
What is an os odontoideum?
How can you tell it apart from a fracture? |
-Os odontoideum is a normal variant of the cervical spine that may, in fact, be posttraumatic.
-It is an unfused dens that may move anterior to the C2 body with flexion and can mimic a fractured dens. -Many of these require surgical fixation; some surgeons fuse every case, believing that they are all unstable. -Radiologists should recognize that this process is not acute, thus, saving the patient from halo fixation and possible immediate surgical intervention. -The radiologic signs of an os odontoideum are the smooth, often well-corticated, inferior border of the dens and the hypertrophied, densely corticated anterior arch of C1. -This latter finding presumably represents compensatory hypertrophy and indicates a long-standing condition. |
|
|
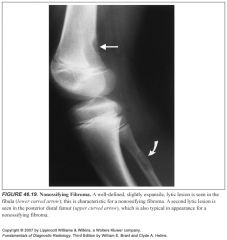
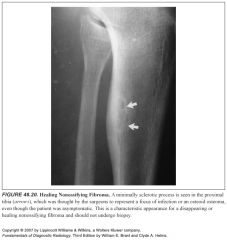
What does a nonossifying fibroma look like on imaging (including nucs)?
|
-They are, classically, lytic lesions located in the cortex of the metaphysis of a long bone and have a well-defined, often sclerotic, scalloped border with slight cortical expansion
-They are found almost exclusively in patients younger than the age of 30 years; hence, the natural history of the lesion is involution. -As they involute, they fill in with new bone, giving it a sclerotic appearance thus, they can have some increased radionuclide activity on bone scans. |
|
|
How can you tell a bone island apart from other sclerotic processes?
|
-Bone islands are not a radiographic dilemma when they are 1 cm or smaller.
-They are always asymptomatic. -Radiographically, two signs can be found to help distinguish giant bone islands from metastases. -First, bone islands usually are oblong, with their long axis in the axis of stress on the bone: for example, in a long bone they align themselves along the axis of the diaphysis. -Second, the margins of a bone island, when examined closely, will show bony trabeculae extending from the lesion into the normal bone in a spiculated fashion. -This is characteristic of a bone island and helpful in differentiating it from a more aggressive process. |
|
|
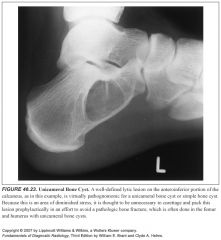
Where do unicameral bone cysts occur in the calcaneus?
|
They always occur in the anteroinferior portion of the calcaneus
|
|
|
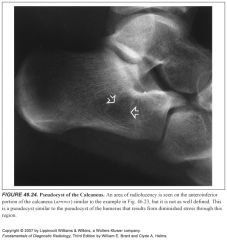
Where does pseudotumor of the calcaneus occur?
|
They always occur in the anteroinferior portion of the calcaneus, an area that does not receive undue stress.
|
|
|
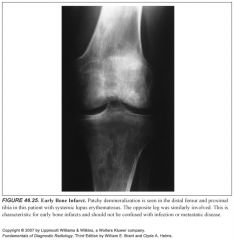
Describe the appearance of bone infarcts on imaging:
|
-Early in the course of its development, a bone infarct can have a patchy or mixed lytic-sclerotic pattern or even resemble a permeative process
-If this process can be noted to be multiple and in the diametaphyseal region of a long bone, especially if the patient has an underlying disorder such as sickle cell anemia or systemic lupus erythematosus, areas of early bone infarction should be considered. -Later on, irregular serpiginous sclerotic lines resemble "chinese characters" -In some cases, the characteristic MR appearance of an infarct may save a patient from biopsy when the plain films are equivocal -Serpiginous lines of decreased T1/T2 signal -characteristic "double line sign" of outer increased T2 signal, inner decreased T2 signal |
|

|
1
|
|

|
2
|
|
|
3
|
|

|
4
|
|

|
5
|
|
|
6
|
|
|
7
|
|
|
8
|
|

|
9
|
|
|
10
|
|
|
11
|
|

|
12
|
|

|
13
|
|
|
14
|
|
|
15
|
|

|
16
|
|
|
17
|
|

|
18
|
|
|
19
|
|
|
20
|
|

|
21
|
|

|
22
|
|
|
23
|
|
|
24
|
|
|
25
|
|

|
26
|

