![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
146 Cards in this Set
- Front
- Back
|
Before placing a line for pulmonary angiogram what 2 things should be done first
|
Check for LBBB (need pacer), check Doppler for groin clot (IJV approach)
|
|
|
What type of catheters are used for pulmonary angiography
|
Use standard diagnostic catheter (pigtail, Grollman) via R femoral vein or R IJ vein
|
|
|
What should be done if the patient has V-tach
|
If patient has Vtach, reposition catheter/wire
If sustained, 100 mg lidocaine bolus then 2 mg/min |
|
|
Before injecting contrast what should always be done first
|
Check PA pressures before injecting
If very high (> 70 mm Hg) decrease contrast dose to lessen risk of right heart failure |
|
|
What are the 2 MCC of lower GI bleed
|
diverticular disease, angiodysplasia
|
|
|
What is angiodysplasia
|
dilated submucosal veins and capillaries in bowel wall. angiodysplasia is a small vascular malformation of the gut. It is a common cause of otherwise unexplained gastrointestinal bleeding and anemia. Lesions are often multiple, and frequently involve the cecum or ascending colon, although they can occur at other places.
|
|
|
What are other less common causes of LGIB
|
post biopsy or polypectomy, tumors, polyps, IBD, ischemia
|
|
|
If a pt has a positive RBC scan what is the next step
|
Pts w/positive RBC scan should undergo angio
|
|
|
What is the sensitivity for detection of bleeds for both angios and Tc RBC
|
Angio can detect 0.5 cc/min
Tc RBC can detect 0.1 cc/min |
|
|
What is the sequence of injection for suspected LGIB
|
Suspected LGIB inject SMA then IMA, and if both negative, celiac
|
|
|
What are the angiographic findings of LGIB
|
Hallmark is extravasation of contrast into bowel
Occasionally extravasation is curvilinear and mimics a vascular structure (pseudovein sign) |
|
|
Does diverticula dz have a characteristic bleed
|
No characteristic appearance unless contrast fills the diverticulum
|
|
|
What are the angiographic findings in a pt with bleeding from angiodysplasia
|
Bleeding vessel usually not seen
Early venous drainage from one portion of bowel, or tram track sign from simultaneous opacification of feeding artery and draining vein |
|
|
What is the procedure for using vasopressin to stop a LGIB
|
Vasopressin: 0.2 U/min repeat angio after 30 min if persists, increase to 0.4 U/min and repeat angio in 30 min if still bleeding, pursue other tx; if working, continue for 12-24 h and taper over 12-48 h
|
|
|
How effective is vasopressin in stopping a LGIB
|
60-90% effective, rebleeding is common
|
|
|
What are 5 contraindications of LGIB
|
Contraindications: severe CAD, severe HTN, dysrhythmias, bleeding at sites with dual blood supply, bleeding directly from large artery, after embolotherapy
|
|
|
What are the potential complications of vasopresin therapy
6 |
bowel ischemia, angina, arrhythmia, HTN, bradycardia, allergy
|
|
|
What is a 2ndary method of treatment for a lower GI bleed
|
embolectomy
|
|
|
How effective is embolectomy for angiodysplasia
|
Usually does not work long term for angiodysplasia or AVM (require surgery)
|
|
|
What is the mainstay of embolization of LGIB
|
Macrocoils, microcoils
|
|
|
Where is the proper placement of coils for LGIB
|
Coils placed distally in arcades proximal to bleeding vasa recta to minimize intestinal ischemia
|
|
|
How much coiling should be done
|
Continue embolizing until bleeding stops
Embolize collaterals if contributing to bleeding |
|
|
How effective is embolization of LGIB
|
60-100% effective acutely, recurrence is uncommon except with AVM, angiodysplasia
|
|
|
What are the contraindicaitons of LGIB embolization
|
poor collateral blood flow, prior gastric or bowel surgery or radiation
|
|
|
What is the main complication of LGIB coiling
|
Complications: bowel infarct < 20%
|
|
|
What are 2 causes of acute SMA occlusion
|
embolism
thrombosis |
|
|
Where do embolisms from the heart normally occlude the SMA
|
Usually from heart, lodge in SMA below origin of middle colic artery
|
|
|
Do SMA embolisms sometimes go into the distal SMA or branches
|
yes
|
|
|
What sometimes happens to the vessels distal to the SMA occlusion
|
Arteries beyond occlusion undergo vasoconstriction
|
|
|
What are the angiographic findings of an acute SMA embolus
|
discrete filling defect, no collaterals
|
|
|
What are the findings of an SMA thombus
|
Usually involves most proximal portion of SMA and is superimposed on chronic atherosclerotic narrowing
|
|
|
What is a major distinguish feature of an acute and chronic occlusion
|
Usually well-developed collaterals
|
|
|
|
|
|
|
|
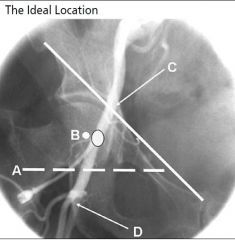
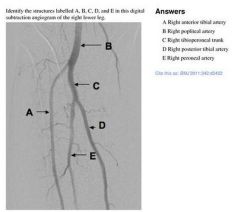
The outlined dot marks the sheath entry site into the CFA at the medial aspect
of the femoral head in the midline. (A) Inferior border of the femoral head. (C) Line demarcating inguinal ligament running from the anterior superior iliac spine to the pubic symphysis. (D) Bifurcation of CFA into superficial femoral artery and profunda. *with permission from Abbott Vascular |
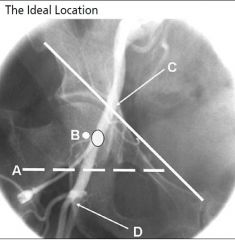
The outlined dot marks the sheath entry site into the CFA at the medial aspect
of the femoral head in the midline. (A) Inferior border of the femoral head. (C) Line demarcating inguinal ligament running from the anterior superior iliac spine to the pubic symphysis. (D) Bifurcation of CFA into superficial femoral artery and profunda. *with permission from Abbott Vascular |
|
|
What should you suspect if there is retrograde filling of the SMA when injecting the IMA
|
Sometimes SMA occlusion can be demonstrated on IMA injection when it fills retrograde
|
|
|
What is the tx of an SMA occlusion
|
: surgical embolectomy for large proximal clot, anticoagulation and vasodilators for distal smaller clots, thrombolysis
|
|
|
What is the indication of percutaneous transhepatic cholaniogram
|
Used to dx and tx proximal biliary obstruction, and occasionally for nonsurgical tx of bile leaks from duct injury
|
|
|
What should be done 1 hour prior to this procedure
|
Antibiotics to include gram negative coverage routinely administered one hour prior
|
|
|
What are 4 complications of PTC
|
sepsis, cholangitis, bile peritonitis, hemorrhage
|
|
|
What is an occasional tx done during PTC
|
occasionally for nonsurgical tx of bile leaks from duct injury
|
|
|
What are the 2 approaches of PTC
|
right and left
|
|
|
What is the technique for insertion of the needle during PTC
|
22G Chiba needle, right lateral midaxillary approach below 10th rib (to avoid pleura) under fluoroscopy
|
|
|
What is a chiba needle
|
22 gauge thin-walled needle with a sharp inner mandrin originally designed at the University of Chiba, Japan, for fine needle puncture (FNP) and for percutaneous transhepatic cholangiography PTC . Today it is also used for many other access punctures such as percutaneous nephrostomy PCN , fluid collections,
|
|
|
What is the landmark that the chiba needle should be directed toward
|
Needle passed over rib, directed in a plane parallel to table top aimed toward T11
|
|
|
How far should you advance the chiba needle
|
Stop advancing needle when you reach midclavicular area
|
|
|
After reaching the midclavicular region what should be done next
|
Remove stylet and inject 0.1 cc 60% contrast while slowly retracting the needle
|
|
|
How do you know if you are in a bile duct
|
When contrast fills a tubular structure and stays there, you are likely in a bile duct
|
|
|
What is the next step once you are in the bile duct
|
Remove 5-10 cc of bile and send for Gram stain and culture
Inject additional 5-10 cc contrast to confirm |
|
|
What is the region of insertion of the needle for a left sided PTC
|
Left subcostal approach in the epigastrium
US used to access a bile duct while avoiding artery and portal vein |
|
|
What is the general difference between benign and malignant biliary strictures
|
benign strictures tend to taper, where as, malignant will be abrupt
|
|
|
What is the radiographic difference in appearance of AIDS cholangitis and PSC
|
PSC and AIDS cholangitis are indistinguishable: multifocal strictures with scattered normal areas +/- diverticula
|
|
|
What is the appearance of the biliary ducts in a pt with a klatskin tumor
|
usually located near hilum (Klatskin), abrupt and possibly nodular, dilated intrahepatic ducts
|
|
|
What is the appearance of the biliary ducts in a patient with pancreatic or ampullary Ca
|
abrupt occlusion at distal CBD with a beaked appearance
|
|
|
What is the general sequence of exchange of wires in a pt with a stenosis or stricture
|
Pass 0.018 in wire through Chiba for PTC
Exchange for 0.038 in wire and advance catheter over wire Dominant proximal stricture can be angioplastied |
|
|
What type of pts will get biliary stents
|
Stents can be used for malignancy or nonsurgical candidates
|
|
|
What are 3 ways to drain
|
3 types of drainage: internal, external, both
|
|
|
What are the surgical options for a traumatic AVF
|
surgical ligation; catheter embolization.
|
|
|
What is the angiographic findings in a patient with an AVF
|
on arteriogram, filling of a larger vascular structure, less densely opacified, adjacent to artery
|
|
|
What type vessels are effected by takayasu arteritis
|
Large artery vasculitis
|
|
|
What specific vessels are effected by takayasu arteritis
|
Primarily involves aorta, great vessels, pulmonary arteries
|
|
|
What is the demographics that are effected by takayasu
|
Usually young to middle-aged women
|
|
|
What are the angiographic findings in a patient with takayasuu
|
Dilation or irregularity of ascending aorta, narrowing of descending aorta, long stenoses or occlusions of arch vessels
|
|
|
What are the findings in a patient with takayasu
|
CT/MR: enhancement of artery wall in acute phase
|
|
|
When is there enhancement of the arterial wall in takayasu
|
acute phase
|
|
|
What is the first stage of Takayasu
|
stenoses of arch and branch vessels
|
|
|
How many stages of takayasu are there
|
4
|
|
|
What is the second stage of Takayasu
|
descending thoracic and abdominal aorta + abdominal branches
|
|
|
What is the 3rd stage of takayasu
|
aortic arch plus abdominal aorta
|
|
|
What is the 4th stage of takayasu
|
pulmonary artery and aorta
|
|
|
What are the 4 stages of takayasu
|
1: stenoses of arch and branch vessels
2: descending thoracic and abdominal aorta + abdominal branches 3: aortic arch plus abdominal aorta 4: pulmonary artery and aorta |
|
|
When is treatment of takayasu delayed until
|
angioplasty and stent delayed until disease is inactive if possible
|
|
|
What occurs in the 4th stage of takayasu
|
pulmonary artery and aorta
|
|
|
What demographic is most commonly effected by giant cell arteritis
|
older women
|
|
|
What artery is giant cell arterititis known for
|
Usually involves the temporal artery
|
|
|
Takayasu will effect young and middle age women and what age group of women does giant cell arteritis effect
|
older women
|
|
|
What vessels does giant cell arteritis effect
|
Involves distal subclavian or axillary arteries,
|
|
|
What do the lesions of giant cell arteritis look like
|
Lesions are long and smooth
|
|
|
What vessels are not effected by giant cell arteritis
|
not the brachiocephalic, common carotids, or proximal subclavians
|
|
|
What is the treatment for a staghorn calculus
|
percutaneous nephrolithotomy
|
|
|
What is done on the first and second day when removing a staghorn calculus
|
Single or 2-stage (initial access on one day, and then stone extraction on another day)
|
|
|
What is the location of the approach when accessing the kidney for removal of a staghorn calculus
|
Posterolateral approach below 12th rib
|
|
|
What are 2 potential ways to guide access into the collecting system in a patient with a staghorn calculus
|
w/US guidance or opacification of collecting system w/fluoro guidance
|
|
|
Once an 18G needle is advanced into the collecting system what is the next step in tx of a patient with staghorn calculus
|
0.038 in guidewire is advanced to bladder
|
|
|
Why is a nephrostogram done 24-48h after removal of a stone
|
Nephrostogram 24-48 h after stone extraction to detect residual fragments or obstruction
|
|
|
When is the nephrostomy catheter removed
|
Only remove percutaneous nephrostomy catheter after documenting forward flow on a gravity nephrogram through the tube
|
|
|
What are potential complications of percutaneous nephrolithotomy
|
Bleeding, sepsis, perforation of collecting system or ureter (usually heals spontaneously if allowed to drain externally)
|
|
|
Besides the renal arteries where does FMD tend to affect
|
MC renal arteries, can also involve ICAs, usually mid to distal portion
|
|
|
How often is FMD bilateral
|
Bilateral in 2/3,
|
|
|
What percent are associated with intracranial aneurysms
|
25% assoc w/intracranial aneurysms
|
|
|
What are the 5 types of FMD
|
Medial fibroplasia (MC, 60-70%, string of beads)
Perimedial fibroplasia (15-25%, irregular beaded narrowing) Medial hyperplasia (5-15%, tubular smooth narrowing) Intimal fibroplasia (1-2%, focal, smooth) Adventitial fibroplasia (< 1%, tubular smooth |
|
|
What is the treatment of FMD
|
PTA
|
|
How big for lithotripsy
|
How big for percutaneous nephrolithomy
|
|
|
What are the indications for percutaneous lithothomy
|
|
|
THIS IS THE FIRST CHOICE FOR AVF. Hemodialysis access. Endogenous radiocephalic
arteriovenous fistula. Note the inflow radial artery (upper right arrow), efferent radial artery (arrowhead), and outflow cephalic vein (curved arrow). |
YES
|
|
|
What is the preferred type of graft for dialysis
|

Synthetic loop graft from the distal brachial artery
to the cephalic vein. Crossed catheters are in place for pulse-spray thrombolysis. |
|
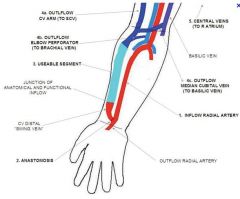
radiocephalic AVF
|
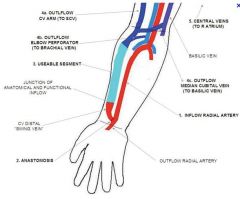
Inflow Vs outflow in radiocephalic AVF
|
|

upper ext venous anatomy
|
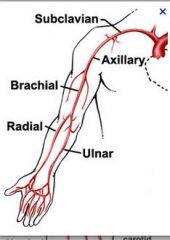
upper ext art anatomy
|
|
|
What is the MCC of mesenteric insufficiency
|
atherosclerotic dz of the mesenteric vessels
|
|
|
What is the MC demographic to have mesenteric ischemia
|
elderly women
|
|
|
In order for mesenteric ischemia to take place what must occur
|
2 of the 3 vessels must have significant stenoses or occlusions
|
|
|
What are other causes of mesenteric ischemia
|
thrombus, embolus, extrinsic compression dissection, vasculitis, vasoconstricting drugs (diffuse stenosis), shock/hypotension (nonocclusive)
|
|
|
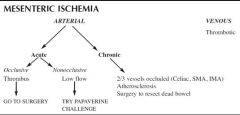
What is the tx of mesentric vascular insufficiency
|
Acute: occlusive surgery; nonocclusive papaverine
Chronic: PTA/stent |
|
|
What are causes of extrinisic compression that may lead to mesenteric ischemia
|
tumor, inflammatory mass, median arcuate ligament syndrome
|
|
|
What is the typical finding of drug related mesenteric ischemia
|
diffuse stenosis from vasoconstricting drugs
|
|
|
Can hypotension cause vascular insufficiency
|
yes
|
|
|
What are the findings of shock or hypotension leading to vascular insufficiency
|
Diffuse narrowing or segments of alternating spasm and dilation
Poor filling of vasa recta |
|
|
What is the appearance of the vasa recta in patients with hypotension
|
`Poor filling of vasa recta
|
|
|
When do you find slow flow w/contrast persisting in intestinal branches for > 2 s after injection has ended
|
shock/hypotension
|
|
|
What is the work up for a patient with mesenteric insufficiency
|
|
|
|
What is considered a special case of celiac stenosis
|
median arcuate ligament syndrome
|
|
|
What is the cause of median arcuate ligament syndrome
|
Superior aspect of celiac compressed by median arcuate ligament ( which is connected to the crura of the diaphragm)
|
|
|
What is the common demographic and symptoms of median arcuate ligament syndrome
|
Usually occurs in thin young women
Abdominal pain, weight loss, nausea |
|
|
When are the symptoms worse in median arcuate ligament syndrome
|
Symptoms worse during exhalation (may be seen during expiration)
|
|
|
What is another name for leriche syndrome
|
infrarenal aortic occlusion
|
|
|
What are the SS of leriche syndrome
|
claudication and impotence
|
|
|
What is a major predisposing factor to leriche syndrome
|
smoking
|
|
|
What is the tx of leriche syndrome
|
aortobifemoral graft, endovascular stent graft (possibly subintimal)
|
|
|
What is the ddx of leriche syndrome
|
Williams syndrome, Takayasu arteritis, giant cell arteritis, dissection, neurofibromatosis
|
|
|
If the aorta is completely occluded in leriche syndrome how does blood get to the lower extremities
|
collateral circulation
|
|
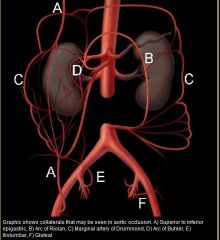
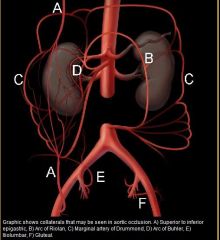
collaterals
|
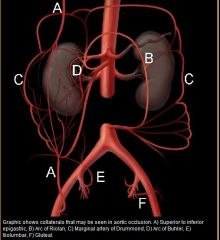
collaterals
|
|
|
Where is the arc of riolan
|
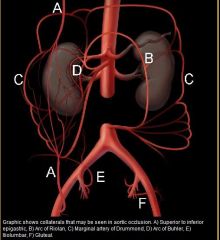
|
|
|
Can williams syndrome, takayasu, and giant cell arteritis affect the aorta and make it appear small
|
yes
|
|
|
What is the pathway of the internal mammary to the external iliac
|
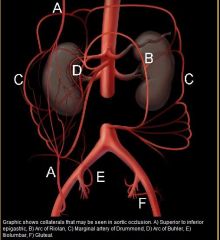
internal mammary to the superior epigastric to the inferior epigastric to the external iliac
|
|
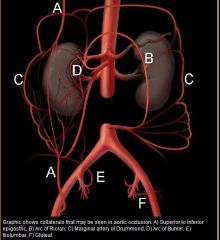
Intercostals, subcostal, and lumbar arteries iliolumbar, lateral sacral, and superior gluteal branches of posterior division of internal iliacs
|
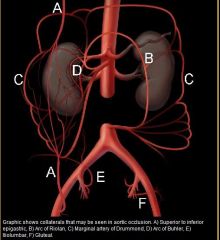
Intercostals and lumbars deep circumflex iliac external iliac
|
|
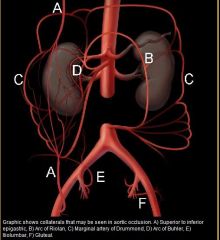
SMA IMA superior and middle hemorrhoidals internal iliac external iliac
|
|
|
|
Why are the internal iliac arteries prone to transection
|
Internal iliac artery and branches run close to bones and ligaments of pelvis
|
|
|
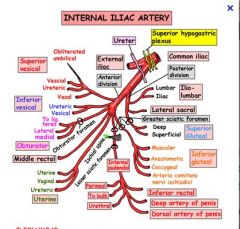
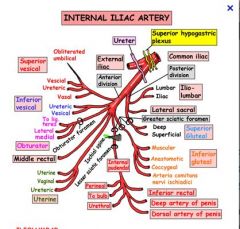
What are the branches of the internal iliac arteries
|
Internal iliac artery: anterior branchesWhat Bill admitted to Hilary: "I Milked Our Insatiable Intern's Udders Under the Desk": Inferior gluteal Middle rectal Obturator Inferior vesical artery Internal pudendal artery Umbilical U/D=Uterine artery (female)/ Deferential artery (male)
|
|
|
|
|
|
What are the common causes of bleeding of the internal iliac arteries
|
Frequently injured in MVAs, falls, crush injuries
|
|
|
What percent of pelvic fx will have an associated bleed
|
10% pelvic fxs have bleeds requiring embolization, mostly AP or lateral compression type injuries
|
|
|
What branches MC have bleeding after a fx
|
MC sources are superior gluteal and internal pudendal
|
|
|
What is the tx of a internal iliac bleed
|
selective embolization w/Gelfoam, coils
|
|
|
What part of the esophagus will an abberant right subclavian artery be located
|
posteriorly
|
|
|
What is the MC aortic arch anomaly
|
the right abberant subclavian (2%)
|
|
|
Does an abberant right subclavian pass behind the trachea and esophagus
|
yes
|
|
|
What is the dilated portion of the aortic arch arise from
|
diverticulum of kommerel
|
|
|
If there is a clinical symptom what is the most common SS
|
dysphagia
|
|
|
Is the abberant vessel in abberant right subclavian artery proximal or distal
|
distal (more posterior)
|
|
|
What happens to the bronchial arteries in a patient with cystic fibrosis
|
they will hypertrophy
|
|
|
Do cystic fibrosis patients sometimes have hemoptysis
|
yes
|
|
|
What artery is most commonly responsible for hemorrhage in patients with CF
|
the bronchial arteries
|
|
|
What is the common cause of hemoptysis in patients with TB
|
pulmonary arteries
|
|
|
Besides CF what are some other causes of hemoptysis
|
Rasmussen aneurysm, AVM, or traumatic PA pseudoaneurysm and TB (other infections)
|
|
|
What are the causes of massive hemopthysis
|
infection (aspergilloma, TB), bronchiectasis, CF, tumor
|
|
|
What is the definition of massive hemoptysis
|
over 500ml in 24h
|

