![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
36 Cards in this Set
- Front
- Back
|
define kock henle postulates.
|
.
Kock-henle postulates is a way to identify a particular microbe as the cause of a particular disease. 1. Isolate the organism from every case 2. Propagate the organism in pure culture in vitro 3. Reproduce disease by injecting the organism into a suitable recipient 4. Re-isolate the organism This method is okay from major acute disases like plague, small pox and typhoid but not suitable for chronic or minor conditions, multiple causes, where pathogen can’t be grown. - - |
|
|
Describe koch’s postulate vs diagnosis.
|
Koch’s postulates state to first isolate the same organism from many patients whereas in diagnosis one or samples of organism are taken from one patient. Secondly, following koch’s postulates, the isolates are grown in vitro and injected into suitable recipient to see if disease is reproduced. Diagnostically, the isolates are identified, investigated to see if organism is a recognised pathogen for the disease affecting the patient at the relevant site. It is also investigated with the specific organism is always associated with disease and whether there are other recognised causes for the disease.
If disease is reproduced in model then there is a causal link according to koch’s postulates. Diagnosis takes the most probable explanation. |
|
|
Give examples of pathogens having different relationships with clinical disease.
|
1 organism causes 1 disease
- Clostridium tetani causes tetanus - Rabies virus causes rabies - Plasmodium ssp causes malaria Many organisms cause 1 disease. - Pneumonia is caused by strep pneumoniae, haemophilus influenza, legionella, Chlamydia, influenza virus, respiratory syncytial virus, SARS - Urinary tract infections are caused by e coli, proteus spp, staph. Saprophycticus, enterococcus spp - Meningitis – strep pneumonia, haemophilis influenza, neisseria meningitides (NHS), mycobacterium tuberculosis, Cryptococcus neoformans 1 organism causes many disease - Staphyloccus aureus – abscess, food poisoning, osteomyelitis - Escherichia coli – diarrhoea, UTI, septicaemia - HIV –immunodeficiency, seroconversion illness, opportunistic infections, encephalopathy, enteropathy |
|
|
Give examples of gram positive cocci.
|
Gram positive cocci have a thick cell wall and no outer membrane.
- Staphylococcus, streptococcus, enterococcus |
|
|
Give examples of gram negative cocci.
|
Gram negative cocci have a thin cell wall and an outer lipopolysacharide membrane.
- Neiserria - encapsulated bacteria –very bad in asplenic patients. |
|
|
Give examples of gram positive bacilli
|
Bacillus(fragilis), corynebacterium (dipheriae), clostridium
|
|
|
Give examples of gram negative bacilli
|
enterobacteriaceae
- Escherichia - Salmonella - Shigella - Vibrio - Haemophilus - Legionella - Bacteroides |
|
|
List organisms that can’t be classified with the gram stain, what other stains are used?
|
Mycobacterium – use acid fast stain, treponema- dark phase microscopy, Chlamydia, mycoplasia..
|
|
|
Outline the basic features in viral replication cycles
|
Viral replication cycles may be cytolytic or non cytolytic and n some cases may result in the agent remaining in the target cell.
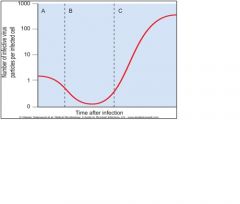
1. Attachment 2. Penetration – fusion with endosome and then fusion with acidic endosome membrane 3. Uncoating then eclipse phase 4. Nucleic acid and protein synthesis 5. Assembly of virions – viral protein 6. Release and re-infection: enveloped viruses are released by budding, non-enveloped viruses are released by lysis. PHASE A – absorption Phase b – eclipse phase: the time taken for the virions to gain control of host cells synthetic machinery and produce progeny virions. Phase c – assembly and release |
|
|
describe the routes of viral transmission and the stages in viral pathogenesis
|
.
Routes of transmission: faecal-oral, respiratory, mucosal, transcutaneous, vertical The stages in viral pathogenesis involve encounter & entry, primary replication, dissemination & tissue tropism, & often secondary multiplication with/without viraemia Viral infections may manifest as lytic infections, latent infections &/or chronic infections. |
|
|
Briefly explain the meaning and medical significance of the terms prion, defective virus, transforming virus and viroids.
|
Prions are infectious proteins with no DNA or RNA. They were originally normal body proteins that get converted into an alternate configuration by contact with other prion proteins. The main protein involved in human and mammalian prion diseases is called “PrP”. They are extremely robust proteinaceous infectious particles and are difficult to remove by disinfection.
- Prions form insoluble deposits in the brain and cause CJD- creutzfeld jakob disease and a number of other transimissible spongiform encephalopathies. Defective virus – A virus particle that contains insufficient nucleic acid to provide for production of all essential viral components, thus infection is not produced except under certain conditions. Eg hepatitis D virus requires the assistance of hepatitis B virus for its propagation. The hepatitis D virus nucelocapsid is encapsidated in HBsAg ( HBV antigen). Preventative measures for HBV can also protect against HDV. Transforming virus- viral genome remains in host cell nuclei and is capable of transforming the host Viroids –naked covalently closed (ss)RNA of less than 400 nucleotides . . - . |
|
|
Describe latent viruses.
|
Some viruses can enter the nervous system and remain dormant for years. The chickenpox caused by varicella zoster and reappear in the adult as shingles, a painful body rash
|
|
|
Outline the basic structural features of a bacterial cell
|
A bacterial cell is a prokaryote.
It has a peptidoglycan cell wall which maintains its shape and protects the cell from differences in osmotic pressure between the cell and the environment. It is the target for many antibiotics and lysozymes. Pili or fimbraie are thin projections which are sites of attachment to host cells. E coli has specialised fimbrae that binds to manose receptors on uretetic epithelial cells. Fimbrae antigens are often immunogenic but vary between strains so that repeated infections can occur eg neisseria gonorrhoea. Flagella allow locomotion of bacteria enabling them to find sources of nutrition and to penetrate host mucus. The flagella may be single or numerous and may be at one end –POLAR or at many points –PERITRICHOUS (peri itrikus). Slime is a polysaccharide material produced by some bacteria growing in biofilms that protects the organism from immune attack and eradication by antibiotics. The lipopolysaccharide outer membrane on gram negative bacteria protects from complement mediated lysic and is toxic, forming the endotoxins that can result in excessive cytokine release and lead to shock. The capsule is a loose polysaccharide structure which surrounds the bacterial cell from phagocytosis. |
|
|
Describe different manifestations of growth.
|
AGAR CULTURE
Colonies – agar cultures in petri dishes. The colonies can arise from a single bacterium and colony counts are used to enumerate live bacteria in a suspension BROTH CULTURE - Planktonic cells – individual free floating bacterial cells that are released from a biofilm - Biofilms – a thin layer of micro-organisms aggregating to a surface that may be organic or inorganic. The organisms secrete slime (extracellular polymeric substance) which protects them from immune attack and eradication by antibodies. Eg viridians streptococcis ( alpha haemolytic) forms a large biofilm called a vegetation around prosthetic heart valves causing endocarditis. |
|
|
Recognise key features in the growth, physiology and genetics of bacteria relevant to infection.
|
Bacteria multiply by binary fission to and if the conditions are appropriate they can multiply exponentially with a lag, exponential and stationary phase. When they in stationary phase, they are more difficult to treat with antibiotics and some may form highly resistant structures called spores. Spores are metabolically inert forms triggered by adverse environmental conditions. They are adapted for long term survival, allowing regrowth under suitable conditions
|
|
|
What about microbial growth is important to know in medicine.
|
It is important to know: The Locations where pathogens can multiply
- The Time taken for infective dose to develop or for symptoms to develop - For Sensitive diagnosis and identification of pathogens by laboratory isolation - As Some physiological growth (biofilms) or non-growth (stasis, dormant or latent) conditions are highly resistant to elimination. |
|
|
What are the Requirements for growth of bacteria
|
- Specific energy sources
- Specific building blocks - Specific atmosphere – anaerobic, microaerobic, aerobic The energy source and building blocks are specific to particular organisms and this allows the bacteria to be recognised by the growth characteristics on different culture media. |
|
|
What is a zoonosis and arthropod borne?
|
A zoonosis is an infection within an animal. Arthropod borne refers to an infection spread via insects.
|
|
|
Which organisms are the most susceptible to eradication?
|
Organisms which can only grow and survive inside the human body such as small pox are the most susceptible to eradication. Whereas organisms which have an environmental eg vibrio cholera or animal reservoir eg salmonella, eradication is impossible or have spores ( clostridium).
|
|
|
Describe methods of Antibiotic resistance.
|
- Intrinsic – part of genome, antibiotic concentration needed is too high or bacteria lack to appropriate site for the antibiotic action eg cell wall
- Intrinsic acquired – mutation - Extrinsic acquired – gene transfer There are many methods of antibiotic resistance - Cell wall/membrane impermeable to antibiotic - Increased efflux of antibiotic - Alteration of target of antibiotic - Enzymes which inactivate the antibiotic - Metabolic bypass eg methotrexate – bypassing folate synthesis |
|
|
Describe Intrinsic antibiotic resistance
|
1. Organisms may be clinically resistant as the levels needed to destroy the bacteria cannot be safely or realistically achieved in the body site.
Eg e.Coli is susceptible to penicillin only at very high concentrations. E coli is thus clinically resistant to penicillin however urinary tract infections caused by e coli can be treated by penicillin, as the penicillin concentrations in urine are extremely high. 2. Bacteria may be inherently resistant so some antibiotics because they do no posses the appropriate target of their action. Eg mycoplamas don’t have a cell wall and so cell wall based antibiotics cannot be used - the beta-lactam ring cannot be targeted. . . . |
|
|
Describe Acquired antibiotic resistance
|
Intrinsically acquired resistance: a mutation in a locus occurs which affects susceptibility to the antibiotic.
Extrinsically acquired resistance: transfer of genetic material between bacteria The spread of acquired resistance requires - The availability of genes which code for the proteins resulting in drug resistance - A method of transfer - A selective environment in which it is advantageous to be resistant – antibiotic selection. |
|
|
Describe the 3 main mechanisms of gene transfer between bacteria.
|
1. Transformation –uptake of naked DNA by a competent cell
2. Transduction – transfer of bacterial DNA via a bacteriophage. The phage head picks up some host DNA during assembly and if some plasmid DNA is picked up, resistance can be transmitted. 3. Conjugation (Bacterial sex) – transfer cell to cell contact. Plasmids carrying drug resistant genes are most common in gram negative bacilli. |
|
|
Define sterilisation, disinfection (cleaning) and antisepsis.
|
• Sterilisation: The inactivation of all self-propagating biological entities (e.g.bacteria, viruses, prions) associated with the materials or areas under consideration.
• Disinfection: The reduction of pathogenic organisms to a level where they no longer constitute a risk. • Antisepsis: Disinfection applied to human tissues Microbial death is never instantaneous and so to achieve sterility or disinfection (risk of transmitting infection is relatively zero) the number of microbes present and the rate at which their numbers are expected to decline must be taken into account. Bacterial spores, mycobacteria and prions are very difficult to inactivate. |
|
|
Describe the factors that may limit the capacity of the different microbes to survive.
|
Generally microbes will die in high temperature, dry conditions and in bright sunlight.
Fastidious bacteria die in the absence of supporting nutrients and strict non-sporing anaerobes die in the presence of oxygen |
|
|
Describe the means by which microbes may be inactivated or excluded to enable safe medical practice
|
Physical methods: filtration, ionzising radiation, heat
Chemical methods: liquid methods ( disinfectants and antiseptics), gaseous agents. |
|
|
What is an autoclave?
|
An autoclave is a closed apparatus delivering moist heat of high temperatures and pressures. It is used to sterilize surgical instruments
|
|
|
Define the terms endogenous infection, exogenous infection and coloniser.
|
An endogenous infection refers to an infection caused by a microbe that is already present on the body. The organism may be an opportunistic disease where a change in site has caused it to be pathogenic eg staphylococcus epidermis is part of the natural flora on skin but an IV line will disrupt the skin and may bring staphylococcus into the blood. In this new location the organism acts as a pathogen. The infection may also be caused if an individual is immunocompromised eg candida is natural flora in throat and vagina but can result in systemic infections in conditions such as neutropenia/long corticosteroid use/HIV.
An exogenogenous infection refers to an infection caused by a microbe that is not already in the body. The microbe may be transferred by sexual contact, fecal-oral, touch, sneezing etc. A coloniser is a bacterium that is able to live and grow in the body without body making any immune response; it can be pathogenic or non-pathogenic. Eg proteus may be found in chronic ulcers but it is not the cause of the ulcers however it is pathogenic in the urinary tract to cause infections. |
|
|
What is important to consider when diagnosing the causal pathogen of an illness?
|
- Where is the organism?
- Is it where it should be? - What is the situation of the host? eg immune compromised. |
|
|
Describe how patients’ specimens are processed to allow for detection of bacterial colonies?
|
A swab is taken from the patients and placed on different medias to test for different organisms. Different organisms have varying incubation periods so some will be checked up to 5 days. No petri dish is examined until after 24hrs.
Microscopy with gram stain can be done immediately classifying the bacterium as gram positive or negative and coci, bacilli, coccibacilli or spiral. The coagulase enzyme can then be checked for. It if is coagulase positive and catalase positive and gram positive it is staphloccus aureus |
|
|
Describe the recevoir, intermediate source and mode of transmission in infection
|
.
The reservoir is the natural habitat for the organism in which it must propagate. It then infects an intermediate source where the organism survives but may or may not propagate. By a certain mode of transmission it infects a susceptible host where multiplication occurs as well as damage to constitute infection. . . . |
|
|
List the common patterns of viral infection
|
Viral respiratory infections
Viral childhood exanthems ( viral rashes) – measles, rubella, chicken pox (VZV), exanthem subitum ( roseola - HHV6 & 7), erythema infectiosum (Parvovirus B19) Viral gastroenteritis – Rotaviruses, enteric adenoviruses, Norwalk virus/norovirus ( most likely cause of epidemic gastroenteritis, Norwalk-like viruses, Caliciviruses and Astroviruses Viral hepatitis – acute or chronic infection; food borne (HAV, HEV) or blood and body fluid (HBV, HCV, HDV, HGV) Human papillomaviruses – cutaneous and anogenital warts; ‘high-risk’ HPV types are believed to play a critical oncogenic role in the development of cervical cancer Herpes viruses – ubiquitous family of viruses giving rise to persistent latent infection; risk of reactivation months-years later – zoster (shingles); aetiological agents of common infections – • EBV – infectious mononucleosis • HHV6 – exanthem subitum – 2- 4 day pyrexia followed by rash • HSV1 and HSV2 – primary herpes gingivostomatitis ( infection of gums), primary herpes genitalis |
|
|
Describe less common viral infections
|
• Human immunodeficiency virus (HIV) – isolated in 1984; global pandemic affecting 30 million people; Retrovirus containing reverse transcriptase; replicates via a chromosomally integrated provirus; transmission through sexual contact.
• Arthropod-borne viruses (‘Arboviruses’) – epidemiology of vector, reservoir and human host; Togaviridae, Flaviviridae and many others; asymptomatic to life threatening; potential for dramatic epidemics • Viral zoonoses – numerous exotic viruses; geographic restriction; threat of emerging zoonoses; viral haemorrhagic fevers pose a major hazard |
|
|
List the different viral and bacterial patterns
|
• Toxin Mediated (Mainly bacteria) – endotoxins and exotoxins.
• Acute (acute viral syndrome/ Acute pyogenic (bacteria)) – symptoms occur in hours to days • Sub-acute (Many viral syndromes) • Chronic (chronic viral infection / Chronic Granulomatous (Bacteria, Fungi, Parasites) |
|
|
Describe endotoxins
|
Endotoxins are LPS on gram negative bacterial outer membranes. They are present to resist attack from antibodies and complement and phagocytes and to decrease permeability. They also allow for Antigenic variation which guarantees the existence of multiple serotypes of the bacterium, so that on secondary exposure to the bacterium the body will not be immune so will have to mount a primary response again. On lysis of the bacteria, endotoxins may be released and can lead to endotoxic shock by stimulating production of cytokines, leading to production of prostaglandins and leukotrienes causing vasodilation and thus inflammation. Endotoxins also stimulate the alternative complement pathway and the coagulation pathway and can result in disseminated intravascular coagulation.
LPS is recognised by TLR -4. |
|
|
Differentiate between endotoxins and exotoxins: chemical nature, relationship to cell, denatured by boiling, antigenic, form toxoid, potency, specificity, enzymatic activity, pyrogenicity.
|
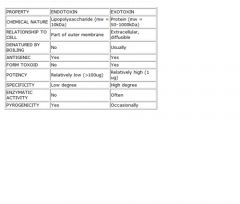
|

