![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
154 Cards in this Set
- Front
- Back
|
What are the layers of the epidermis from the surface to the base? |
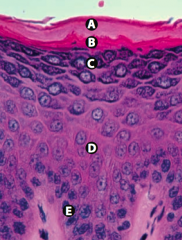
Californians Like Girls in String Bikinis: |
|
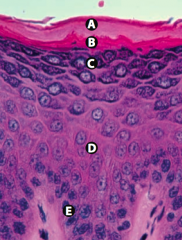
What is Layer A (epidermis)? |
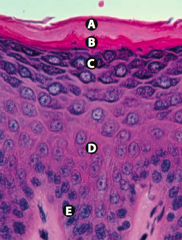
Stratum Corneum (keratin) |
|
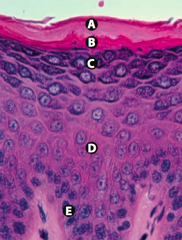
What is Layer B (epidermis)? |
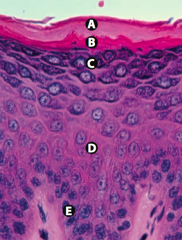
Stratum Lucidum |
|
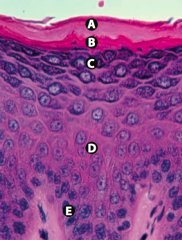
What is Layer C (epidermis)? |
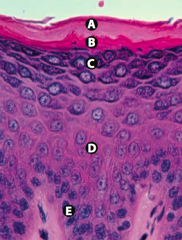
Stratum Granulosum |
|

What is Layer D (epidermis)? |

Stratum Spinosum (spines = desmosomes) |
|
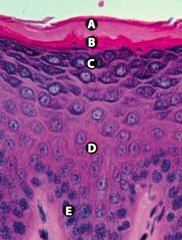
What is Layer E (epidermis)? |
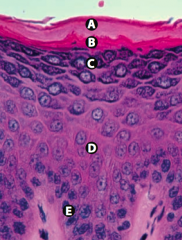
Stratum Basale (stem cell site) |
|
|
What are the types of junctions between epithelial cells? |
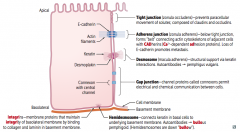
Lateral edge: |
|
|
Which type of epithelial cell junction prevents paracellular movement of solutes? What is it composed of? |
Tight Junctions / Zonula Occludens |
|
|
Which type of epithelial junction is located below the tight junctions, forming a "belt"? What is it composed of? |
Adherens Junctions / Zonula Adherens |
|
|
Which type of epithelial junction provides structural support? What is it composed of? |
Desmosomes / Macula Adherens |
|
|
Which type of epithelial junction permits electrical and chemical communication between cells? What is it composed of? |
Gap Junction |
|
|
Which type of epithelial junction connects keratin in basal cells to the underlying basement membrane? |
Hemidesmosomes |
|
|
Which type of epithelial junction binds to collagen and laminin in the basement membrane? |
Integrins |
|
|
What failure of epithelial cell junctions leads to metastasis? |
Loss of E-cadherin |
|
|
What failure of epithelial cell junctions leads to Pemphigus Vulgaris? |
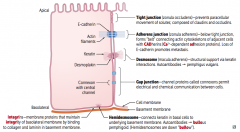
Desmosomes / Macula Adherens |
|
|
What failure of epithelial cell junctions leads to Bullous Pemphigoid? |
Hemidesmosomes (remember, they are down "bullow") |
|
|
What injury do you suspect in a patient with acute knee pain and an anterior drawer sign? |
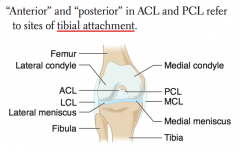
ACL Injury |
|
|
What injury do you suspect in a patient with acute knee pain and a posterior drawer sign? |
PCL injury |
|
|
What injury do you suspect in a patient with acute knee pain and abnormal passive abduction (valgus stress)? |
MCL injury |
|
|
What injury do you suspect in a patient with acute knee pain and abnormal passive adduction (varus stress)? |
LCL injury |
|
|
What injury do you suspect in a patient with acute knee pain and pain on external rotation (McMurray test)? |
Medial Meniscus injury |
|
|
What injury do you suspect in a patient with acute knee pain and pain on internal rotation (McMurray test)? |
Lateral Meniscus injury |
|
|
What is a common injury in contact sports due to lateral force applied to a planted leg? |
Unhappy Triad: |
|
|
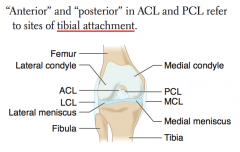
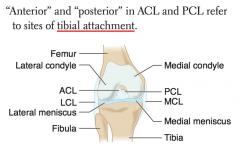
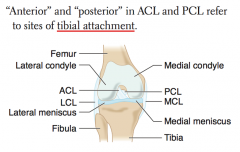
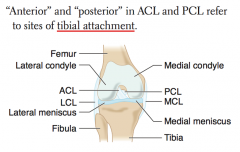
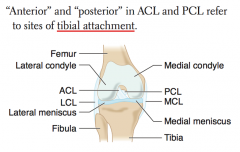
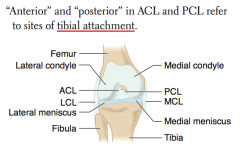
How do you determine which ligament is the ACL vs PCL? |
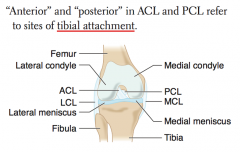
- ACL attaches anteriorly to TIBIA |
|
|
What important landmark can guide you when doing a pudendal nerve block? Function? |
- Ischial spines |
|
|
What is the classic location of the appendix? |
- 2/3 of the distance between the umbilicus and the anterior superior iliac spine (ASIS) |
|
|
What important landmark can guide you when doing a lumbar puncture? |
Iliac crests |
|
|
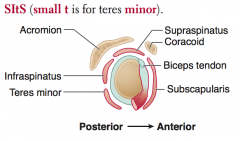
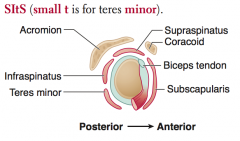
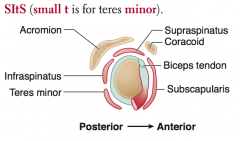
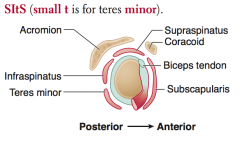
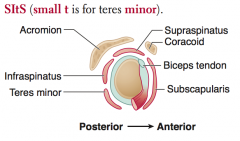
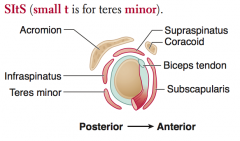
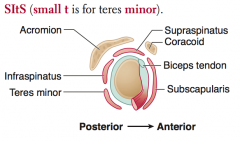
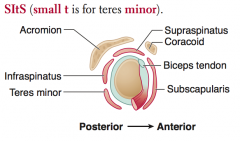
What are the rotator cuff muscles? |
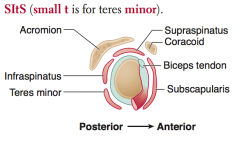
SItS (small t is for teres minor) |
|
|
Which nerves innervate the rotator cuff muscles? Nerve roots? |
- Supraspinatus: suprascapular nerve |
|
|
What is the action of the rotator cuff muscles? |
- Supraspinatus: abducts arm initially |
|
|
What is the action of the Supraspinatus? Innervation? Other? |
- Abducts arm initially (before action of deltoid) |
|
|
What is the action of the Infraspinatus? Innervation? Other? |
- Laterally rotates arm |
|
|
What is the action of the Teres Minor? Innervation? Other? |
- Adducts and laterally rotates arm |
|
|
What is the action of the Subscapularis? Innervation? Other? |
- Medially rotates and adducts arm |
|
|
What is the most common rotator cuff muscle injured? |
Supraspinatus (suprascapular nerve) |
|
|
What is the muscle classically injured in a pitching injury? |
Infraspinatus (suprascapular nerve) |
|
|
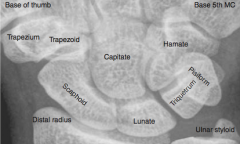
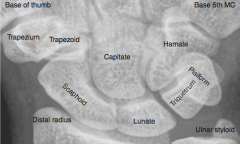
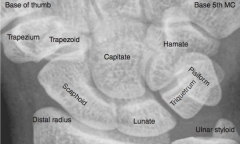
What are the bones in the wrist? |
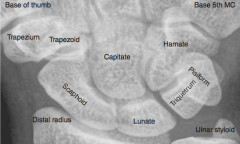
So Long To Pinky, Here Comes The Thumb |
|
|
What is the most commonly fractured carpal bone? |
Scaphoid (palpated in anatomical snuffbox) |
|
|
Which carpal bone is prone to avascular necrosis? Why? |
Scaphoid - owing to retrograde blood supply |
|
|
Dislocation of what bone may cause acute carpal tunnel syndrome? |
Lunate (medial bone closest to arm) |
|
|
A fall on an outstretched hand may damage which bone and cause damage to what nerve? |
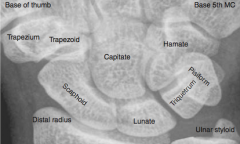
Can damage the hook of the hamate bone, which can cause ulnar nerve injury |
|
|
What happens in Carpal Tunnel Syndrome? |
- Entrapment of median nerve in carpal tunnel |
|
|
What happens in Guyon Canal Syndrome? |
- Compression of the ulnar nerve at the wrist or hand |
|
|
Which nerve syndrome is common in cyclists? Why? |
Guyon Canal Syndrome |
|
|
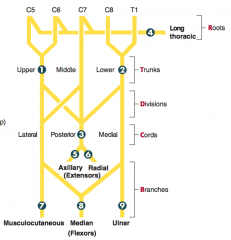
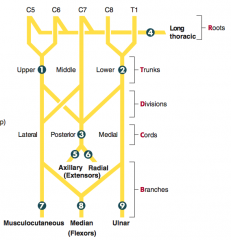
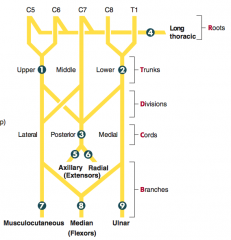
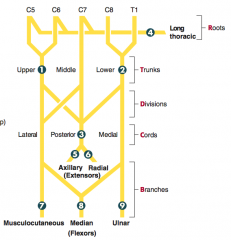
How can you remember the segments of the brachial plexus? |
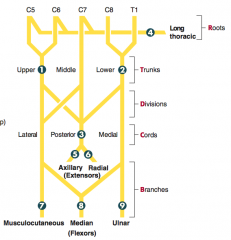
Randy Travis Drinks Cold Beer: |
|
|
What are the types of brachial plexus lesions? |
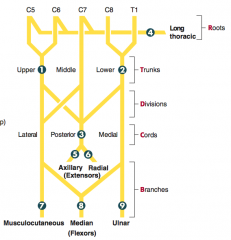
1. Erb palsy (waiter's tip) |
|
|
What injury is caused by traction or tear of the upper trunk (C5-C6 roots)? |

Erb Palsy (Waiter's tip): |
|

What causes Erb Palsy? |

- Traction or tear of upper ("ERB-er") trunk: C5-C6 roots |
|
|
What injury is caused by traction or tear of the lower trunk (C8-T1 roots)? |

Klumpke Palsy |
|

What causes Klumpke Palsy? |
- Traction or tear of lower trunk (C8-T1 roots) |
|
|
What injury is caused by compression of the lower trunk and subclavian vessels? |
Thoracic Outlet Syndrome |
|
|
What causes Thoracic Outlet Syndrome? |
- Compression of lower trunk and subclavian vessels |
|
|
What injury is caused by a lesion of the long thoracic nerve? |

Winged Scapula: |
|
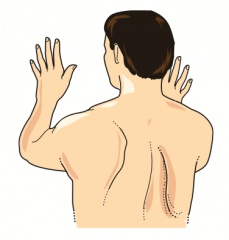
What causes Winged Scapula? |

- Lesion of long thoracic nerve |
|
|
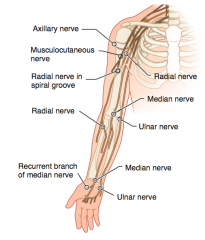
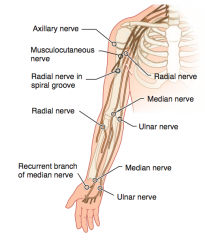
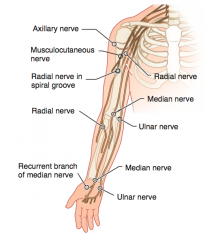
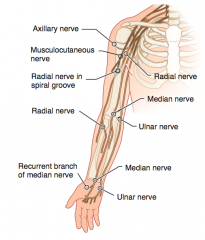
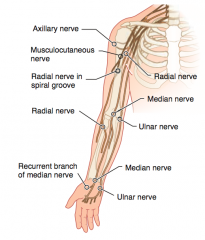
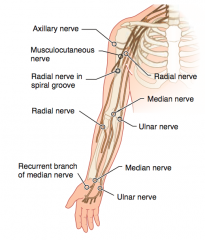
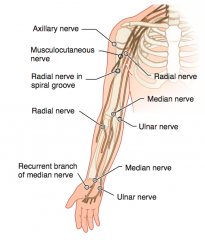
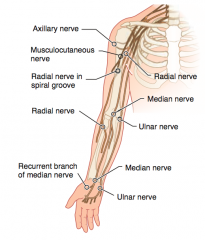
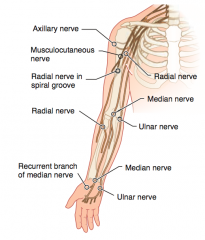
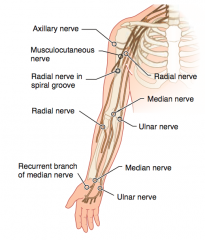
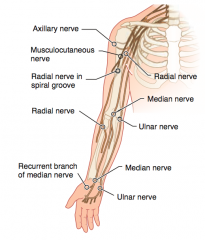
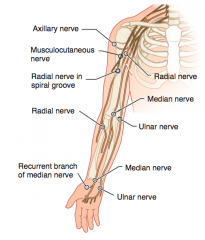
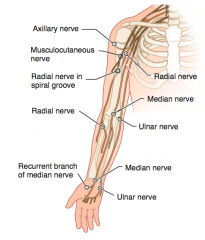
Which nerve roots supply the Axillary nerve? How can it be injured? Presentation of injury? |
- C5-C6 |
|
|
Which nerve roots supply the Musculocutaneous nerve? How can it be injured? Presentation of injury? |
- C5-C7 |
|
|
Which nerve roots supply the Radial nerve? How can it be injured? Presentation of injury? |
- C5-T1 |
|
|
Which nerve roots supply the Median nerve? How can it be injured? Presentation of injury? |
- C5-T1 |
|
|
Which nerve roots supply the Ulnar nerve? How can it be injured? Presentation of injury? |
- C8-T1 |
|
|
Which nerve roots supply the recurrent branch of median nerve? How can it be injured? Presentation of injury? |
- C5-T1 |
|
|
What kind of injury can cause flattening of the deltoid? |
- Fractured surgical neck of humerus or anterior dislocation of humerus |
|
|
What kind of injury can cause loss of arm abduction at the shoulder (>15 degrees)? |
- Fractured surgical neck of humerus or anterior dislocation of humerus |
|
|
What kind of injury can cause loss of sensation over the deltoid muscle and lateral arm? |
- Fractured surgical neck of humerus or anterior dislocation of humerus |
|
|
What kind of injury can cause loss of forearm flexion and supination? |
- Upper trunk compression |
|
|
What kind of injury can cause loss of sensation over the lateral forearm? |
- Upper trunk compression |
|
|
What kind of injury can cause a wrist drop (loss of elbow, wrist, and finger extension)? |
- Midshaft fracture of humerus or compression of axilla (eg, due to crutches or sleeping with arm over chair) |
|
|
What kind of injury can cause decreased grip strength? |
- Midshaft fracture of humerus or compression of axilla (eg, due to crutches or sleeping with arm over chair) |
|
|
What kind of injury can cause loss of sensation over the posterior arm / foream and dorsal hand? |

- Midshaft fracture of humerus or compression of axilla (eg, due to crutches or sleeping with arm over chair) |
|
|
What kind of injury can cause the hand to give the "Pope's blessing"? |
- Supracondylar fracture of humerus (proximal lesion) |
|
|
What kind of injury can cause loss of wrist and lateral finger flexion, thumb opposition, and movement of lumbricals on 2nd and 3rd digits? |
- Supracondylar fracture of humerus (proximal lesion) |
|
|
What kind of injury can cause loss of sensation over the thenar eminence and dorsal and palmar aspects of the lateral 3.5 fingers? |

- Supracondylar fracture of humerus (proximal lesion) |
|
|
What kind of injury can cause the Tinel sign (tingling on percussion)? |

- Carpal tunnel syndrome (distal lesion) |
|
|
What kind of injury can cause the "ulnar claw" on digit extension? |
- Fracture of medial epicondyle of humerus "funny bone" (proximal lesion) |
|
|
What kind of injury causes radial deviation of the wrist upon flexion? |
- Fracture of medial epicondyle of humerus "funny bone" (proximal lesion) |
|
|
What kind of injury causes loss of flexion of wrist and medial fingers, abduction and adduction of fingers (interossei), and actions of medial 2 lumbrical muscles? |
- Fracture of medial epicondyle of humerus "funny bone" (proximal lesion) |
|
|
What kind of injury causes loss of sensation over the medial 1.5 fingers including the hypothenar eminence? |

- Fracture of medial epicondyle of humerus "funny bone" (proximal lesion) |
|
|
What kind of injury causes loss of thenar muscle group movement (opposition, abduction, and flexion of thumb)? |
- Superficial laceration of palm |
|
|
What nerve is commonly injured in a fracture of the surgical neck of the humerus? Presentation? |
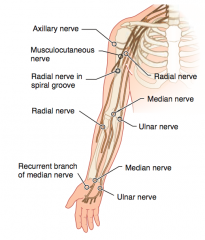
Axillary Nerve (C5-C6) |
|
|
What nerve is commonly injured in an anterior dislocation of the humerus? Presentation? |
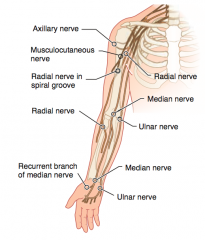
Axillary Nerve (C5-C6) |
|
|
What nerve is commonly injured in an upper trunk compression? Presentation? |
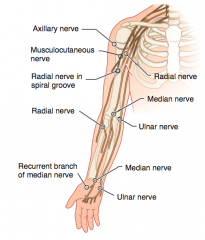
Musculocutaneous nerve (C5-C7) |
|
|
What nerve is commonly injured in a midshaft fracture of the humerus? Presentation? |

Radial nerve (C5-T1) |
|
|
What nerve is commonly injured by using crutches or by sleeping with ones arm over a chair? |

Radial nerve (C5-T1) |
|
|
What nerve is commonly injured by a suprocondylar fracture of the humerus? |

Median nerve (C5-T1) = proximal lesion |
|
|
What nerve is commonly injured by carpal tunnel syndrome and wrist laceration? |

Median nerve (C5-T1) = distal lesion |
|
|
What nerve is commonly injured by a fracture of the medial epicondyle of the humerus? |

Ulnar nerve (C8-T1) = proximal lesion at funny bone |
|
|
What nerve is commonly injured by a fractured hook of hamate? |

Ulnar nerve (C8-T1) = distal lesion |
|
|
What nerve is commonly injured by a superficial laceration of the palm? |
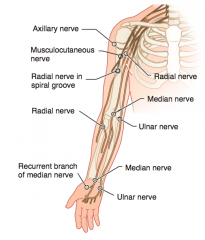
Recurrent branch of the median nerve (C5-T1) |
|
|
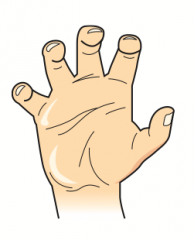
At rest, what kind of balance exists in the hand? |
Balance between the extrinsic flexors and extensors of the hand, as well as the intrinsic muscles of the hand - particularly the lumbrical muscles (flexion of MCP, extension of DIP and PIP joints) |
|
|
What most commonly causes "clawing" of the hand? |
Distal lesions of median or ulnar nerves |
|
|
What are the implications of a lesion in the distal ulnar nerve? |

"Ulnar Claw" sign: occurs when extending fingers / at rest |
|
|
What are the implications of a lesion in the distal median nerve? |

"Median Claw" sign: occurs when extending fingers / at rest |
|
|
What are the implications of a lesion in the proximal ulnar nerve? |

"OK gesture" (w/ digits 1-3 flexed): occurs when making a fist |
|
|
What are the implications of a lesion in the proximal median nerve? |

"Pope's Blessing": occurs when making a fist |
|

What can cause this hand presentation? |

- Lesion of distal ulnar nerve: occurs when extending fingers / at rest (Ulnar claw) |
|

What can cause this hand presentation? |

- Lesion of distal median nerve: occurs when extending fingers / at rest (Median claw) |
|
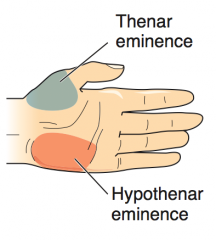
What causes atrophy of the thenar eminence (unopposable thumb)? |
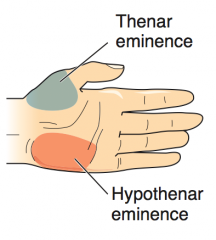
Median nerve lesions |
|
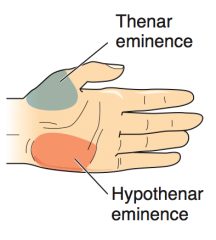
What causes atrophy of the hypothenar eminence? |
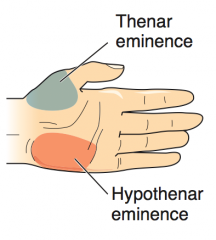
Ulnar nerve lesions |
|
|
What are the Thenar muscles? What innervates them? |
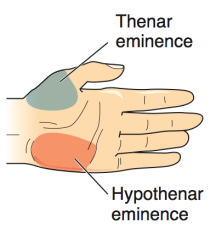
- Opponens pollicis |
|
|
What are the Hypothenar muscles? What innervates them? |
- Opponens digiti minimi |
|
|
What are the types of interosseous muscles? Actions? |
- Dorsal interosseous muscles: ABduct the fingers = DAB |
|
|
What is the action of the lumbrical muscles? |
- Flex at MCP joint |
|
|
What are the nerves in the lower extremity? Nerve roots? |
- Obturator (L2-L4) |
|
|
What nerve roots supply the Obturator nerve? What can classically cause injury to this nerve? Presentation? |
- L2-L4 |
|
|
What nerve roots supply the Femoral nerve? What can classically cause injury to this nerve? Presentation? |
- L2-L4 |
|
|
What nerve roots supply the Common Peroneal nerve? What can classically cause injury to this nerve? Presentation? |
- L4-S2 |
|
|
What nerve roots supply the Tibial nerve? What can classically cause injury to this nerve? Presentation? |
- L4-S3 |
|
|
What nerve roots supply the Superior Gluteal nerve? What can classically cause injury to this nerve? Presentation? |
- L4-S1 |
|
|
What nerve roots supply the Inferior Gluteal nerve? What can classically cause injury to this nerve? Presentation? |
- L5-S2 |
|
|
Which nerve is commonly injured by pelvic surgery? Presentation? |
Obturator Nerve (L2-L4) |
|
|
Which nerve is commonly injured by pelvic fracture? Presentation? |
Femoral Nerve (L2-L4) |
|
|
Which nerve is commonly injured by trauma or compression of the lateral aspect of the leg? Presentation? |
Common Peroneal Nerve (L4-S2) |
|
|
Which nerve is commonly injured by a fibular neck fracture? Presentation? |
Common Peroneal Nerve (L4-S2) |
|
|
Which nerve is commonly injured by knee trauma? Presentation? |
Tibial Nerve (L4-S3) |
|
|
Which nerve is commonly injured by a Baker cyst? Presentation? |
Tibial Nerve (L4-S3) |
|
|
Which nerve is commonly injured by tarsal tunnel syndrome? Presentation? |
Tibial Nerve (L4-S3) |
|
|
Which nerve is commonly injured by a posterior hip dislocation? Presentation? |
Superior Gluteal Nerve (L4-S1) |
|
|
Which nerve is commonly injured by polio? Presentation? |
Superior Gluteal Nerve (L4-S1) |
|
|
What are the characteristics of Trendelenburg sign / gait? |
- Pelvis tilts because weight-bearing leg cannot maintain alignment of pelvis through hip abduction |
|
|
What nerve roots supply the Sciatic nerve? Function? |
- L4-S3 |
|
|
How are nerves and arteries classically named? |
Nerves are arteries are frequently named together by the bones / regions with which they are associated |
|
|
What are the names of the nerve and artery that supply the axilla / lateral thorax? |
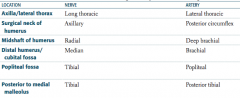
- Long thoracic nerve |
|
|
What are the names of the nerve and artery that supply the surgical neck of the humerus? |
- Axillary nerve |
|
|
What are the names of the nerve and artery that supply the midshaft of the humerus? |
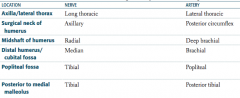
- Radial nerve |
|
|
What are the names of the nerve and artery that supply the distal humerus / cubital fossa? |
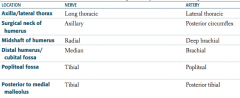
- Median nerve |
|
|
What are the names of the nerve and artery that supply the popliteal fossa? |
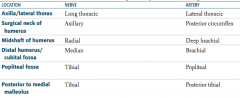
- Tibial nerve |
|
|
What are the names of the nerve and artery that supply the posterior to medial malleolus? |
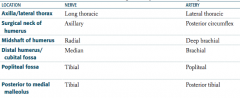
- Tibial nerve |
|
|
What are the steps in muscle contraction? |
1. AP depolarization → opens Ca2+ channels → NT release |
|
|
What is the first step in muscle contraction? |
Action potential depolarization opens presynaptic voltage-gated Ca2+ channels, inducing NT release |
|
|
What is the second step in muscle contraction, after NT release? |
Post-synaptic ligand binding, leads to muscle cell depolarization in the motor end plate |
|
|
What is the third step in muscle contraction, after depolarization of the motor end plate? |
Depolarization travels along the muscle cell and down the T tubule |
|
|
What is the fourth step in muscle contraction, after depolarization of the T tubule? |
Depolarization of the voltage-sensitive Dihydropyridine Receptor, mechanically coupled to the Ryanodine Receptor on the Sarcoplasmic Reticulum, inducing a conformation change, causing Ca2+ release from SR |
|
|
What is the fifth step in muscle contraction, after Ca2+ release from SR? |
Released Ca2+ binds to Troponin C, causing a conformational change that moves Tropomyosin out of the Myosin-Binding groove on Actin filaments |
|
|
What is the sixth step in muscle contraction, after Ca2+ binds Troponin C? |
- Myosin releases bound ADP and subsequently, inorganic PO4(3-) → displacement of myosin on the actin filament (power stroke) |
|
|
A sarcomere is between what boundaries? |
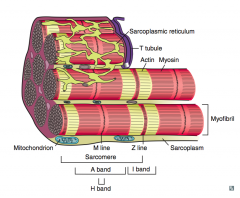
From Z line to Z line |
|
|
What are the contents of the sarcomere? |
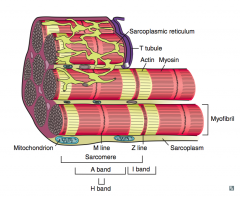
- In the middle: M line |
|
|
What are the types of muscle fibers? |
- Type 1: slow / red ("one slow red ox") |
|
|
What are the characteristics of Type 1 muscle fibers? |
- Slow twitch |
|
|
What are the characteristics of Type 2 muscle fibers? |
- Fast twitch |
|
|
Which muscle fibers are necessary for weight training? |
Type 2 muscle fibers: |
|
|
What are the steps of smooth muscle contraction? |

1. Action potential |
|
|
What are the steps of smooth muscle relaxation? |

1. Nitric Oxide stimulates Guanylate Cyclase |
|
|
How are the uses of myosin light chain kinase and phosphatase different? |

- MLCK used for contraction of smooth muscle by phoshporylating myosin |
|
|
What are the types of bone formation? |
- Endochondral ossification |
|
|
What bones use endochondral ossification? |
Bones of axial and appendicular skeleton, and base of skull |
|
|
What type of bone formation occurs in the axial and appendicular skeleton and the base of the skull? How is it made? |
Endochondral Ossification: |
|
|
What bones use membranous ossification? |
Bones of calvarium and facial bones |
|
|
What type of bone formation occurs in the calvarium and facial bones? How is it made? |
Membranous Ossification |
|
|
What kind of bone formation occurs after fractures and in Paget disease? |
Woven bone formation (endochondral ossification) |
|
|
What are the cells in the bone? |
- Osteoblasts |
|
|
What is the function of Osteoblasts? Source? |
- Build bone by secreting collagen and catalyzing mineralization |
|
|
What is the function of Osteoclasts? Source? |
- Multinucleated cells that dissolve bone by secreting acid and collagenases |
|
|
What hormones act on the bone? |
- Parathyroid Hormone |
|
|
What is the action of PTH on bones? |
- At low, intermittent levels, exerts ANABOLIC effects (building bone) on osteoblasts and osteoclasts (indirect) |
|
|
What is the action of Estrogen on bones? |
- Estrogen inhibits apoptosis in bone-forming osteoblasts and induces apoptosis in bone-resorbing osteoclasts |

