![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
36 Cards in this Set
- Front
- Back
|
What is hypoxia? |
A state of too little oxygen - occurs if the diffusion of gases between the alveoli and blood is impaired or oxygen is inadequate. |
|
|
What is Hypercapnia? |
State of excess CO2 in the blood. |
|
|
What are the different types of hypoxia? Briefly describe each. |
1. Hypoxic - low arterial PO2 2. Anemic - Decreased total O2 bound to Hemoglobin 3. Ichemic - Reduced blood flow 4. Histotoxic - Failure of cells to use oxygen due to poisoning |
|
|
What mechanisms does the body have to avoid hypoxia? |
Body avoids hypoxia through arterial blodo composition sensors: 1. Oxygen sensors 2. CO2 sensors 3. pH sensors |
|
|
What is the main negative effect of excess CO2 in the blood. |
High levels depress the CNA and induce acidosis via the production of HCO3-: CO2 + H2O <> H2CO2 <> H+ + HCO3- |
|
|
Why must plasma pH be monitored? |
prevent denaturation of proteins. |
|
|
What are the three main categories which influence alveolar gas exchange? |
1. Amount of O2 reaching the alveoli 2. Gas diffusion between alveoli and blood 3. Adequate perfusion of alveoli |
|
|
How is the oxygen which reaches the alveoli influenced? |
1. Composition of the inspired air 2. Alveolal ventilation |
|
|
What influences alveolar ventilation? |
1. Lung compliance 2. Airway resistance 3. Rate and depth of breathing |
|
|
What influences gas diffusion between alveoli and blood? |
1. Surface area 2. Diffusion distance |
|
|
What influences the diffusion distance between an alveoli and a capillary? |
1. Barrier thickness 2. Amount of fluid |
|
|
What is the most extreme influence on diffusion efficiency? |
Distance of diffusion. Diffusion is inversely proportional to Surface Area times by barrier permeability, divided by distance squared D ¬ SA * BP/Di^2 |
|
|
What is the typical diffusion distance range of an alveoli and a blood vessel? |
0.1 - 1.5 micrometers (um) |
|
|
What diseases affect diffusion deficiency and why? |
1. Emphysema 2. Fibrotic lung disease 3. Pulmonary Edema 4. Asthma |
|
|
How does emphysema affect diffusion efficiency? |
Causes alveolar destruction which decreases the surface area available for gas exchange. |
|
|
How does Fibrootic lung disease affect diffusion efficiency? |
Causes a thickened alveolar membrane and a loss of lung compliance. This increases the distance for diffsion and lowers alveolar ventilation by causing less oxygen to reach the lungs. |
|
|
How does pulmonary edema affect diffusion efficiency? |
Causes a build up of fluid in the interstitial space which greatly increases the diffusion distance AND pCO2 increases as it dissolves in the interstitial fluid - unlike O2 |
|
|
Why is oxygen so sensitive to diffusion distance? |
Because it has a very low water solubility and so is not carried in the plasma. |
|
|
How can you work out cellular O2 consumption (QO2)? (Mass balance) |
Arterial O2 transport - Venous O2 transport = QO2 |
|
|
How can you work out the net oxygen transport (mass flow)? |
O2 transport = cardiac output (CO) * Oxygen concentration |
|
|
What is the Fick equation? |
The Fick equation determines the rate at which a person uses oxygen in their body. It is a combination of the mass flow and mass balance equations: QO2 = Cardiac Output * (arterial [O2] - venous [O2]) |
|
|
How does hemoglobin act to increase oxygen transport? |
Only a small fraction of oxygen can dissolve in plasma (3ml O2 per liter of blood). Hemoglobin scoops up oxygen continually maintaining diffusion into plasma (by maintaining the concentration gradient) and allowing far more oxygen to be 'dissolved' in the blood.
|
|
|
At 100mg of Hemoglobin in the blood how much additional oxygen can be carried? |
200ml / O2 / L of blood. |
|
|
How does fetal hemoglobin differ in its O2 binding properties to adult hemoglobin? What is the effect of this? |
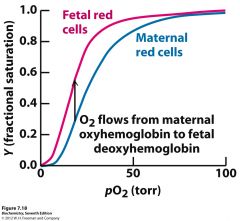
Fetal hemoglobin has a higher affinity for oxygen. This allows adequate oxygen content from simple oxygen diffusion from the maternal to fetal blood in the placenta. |
|
|
What is the effect of changing pH on hemoglobin saturation? |
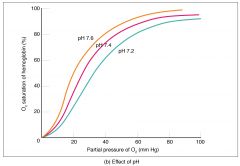
Lower pH = lower affinity for O2 (blue) and vice versa (yellow) |
|
|
What is the effect of changing temperature on hemoglobin? |
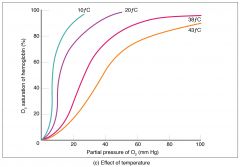
Higher temperature = lower affinity Lower temperature = higher affinity |
|
|
What is BPG? |
2,3 Bisphosphoglycerate - produced by erythrocytes - lowers oxygen binding affinity |
|
|
What is the path of carbon dioxide transport in the body? |
1. CO2 diffuses out of cells into the blood - some dissolves in the blood. 2. About a quarter of the blood binds to hemoglobin to form carbaminohemoglobin 3. Most of the CO2 is converted to bicarbonate (HCO3-) and H+ - Hemoglobin buffers the H+ (HbH) 4. HCO3- enters the plasma in exchange for Cl- 5. CO2 dissolved in plasma diffuses into lungs 6. CO2 unbinds from Hemoglobin by law of mass action 7. Carbonic acid reenters the cell in exchange for Cl-. 8 Carbonic acid combines with protons from HbH forming H2CO3. 9. H2CO3 breaks apart to form H2O and CO2 which then diffuse into the lungs. |
|
|
What is the central component of ventilation control? |
The medulla oblongata |
|
|
What sensors feed into the medulla oblongata & pons to change ventilation? |
1. Medullary chemoreceptors in the brain 2. Carotid and aortic chemoreceptors via afferent sensory neurons. |
|
|
How can emotions and voluntary control affect ventilation? |
Higher brain centres and the limbic system affect the medulla oblongata & pons. |
|
|
How does the medulla oblongata change ventilation? |
Somatic motor neuron excitation of inspiration and expiration muscles. |
|
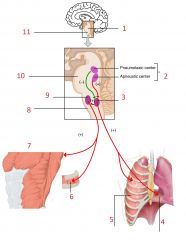
Label: |
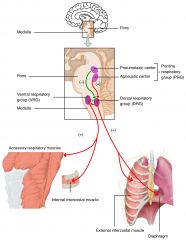
1 - Pons 2 - medulla 3 - Poutine Respiratory group 4 - Diaphragm 5 - external intercostal muscle 6 - Internal intercostal muscle 7 - Accessory respiratory muscles 8 - medulla 9 - Ventral respiratory group (VRG) 10 - Pons 11 - Medulla |
|
|
What is inspiration an example of in respect to homeostasis? |
A positive feedback loop which ceases when fully respired. |
|
|
How do Carotid Body Cells act to affect ventilation? |
1. Detect low pO2 which closes K+ channels 2. Depolarises cell 3. Voltage gated Ca2+ channel opens 4. Neurotransmitter release |
|
|
What do central chemoreceptors in the medulla respond to? |
High CO2 and H+ concentrations - (pH) |

