![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
111 Cards in this Set
- Front
- Back
|
What are the most important disorders of white blood cells?
|
Malignancies
|
|
|
What are the categories of malignancies of white cells?
|
- Lymphoid neoplasms
- Myeloid neoplasms - Histiocytoses |
|
|
What are the origins of Lymphoid Neoplasms?
|
- B-cells (85-90%)
- T-cells (remainder) - NK-cells (rare) |
|
|
What is the phenotype of the neoplastic cells in Lymphoid Neoplasms?
|
Closely resembles that of a particular stage of normal lymphocyte differentiation
|
|
|
What are the origins of Myeloid Neoplasms?
|
Arise from hematopoietic progenitors
|
|
|
What are the types of myeloid neoplasms?
|
- Acute Myeloid Leukemias
- Myelodysplastic Syndromes - Chronic Myeloproliferative Disorders |
|
|
What is the main feature of Acute Myeloid Leukemias?
|
Immature progenitor cells accumulate in BM
|
|
|
What is the main feature of Myelodysplastic Syndromes?
|
Associated w/ ineffective hematopoiesis and PB cytopenias
|
|
|
What is the main feature of Chronic Myeloproliferative Disorders?
|
Increased production of one or more terminally differentiated myeloid elements (eg, granulocytes) which usually leads to increased PB counts
|
|
|
What kind of cells are affected by histiocytoses?
|
Macrophages and dendritic cells
|
|
|
What are Histiocytoses?
|
- Uncommon proliferative lesions of macrophages and dendritic cells
- Langerhans cells (type of immature dendritic cell) gives rise to a spectrum of neoplastic disorders called Langerhans Cell Histiocytoses |
|
|
What does the term lymphocytic leukemia mean?
|
- Leukemia is a neoplasm that presents w/ widespread involvement of the BM and usually, but not always, the peripheral blood
- Lymphomas occasionally have leukemic presentations |
|
|
What are the common features of virtually all Hodgkin Lymphomas and 2/3 of NHLs?
|
Non-tender lymph nodes (often >2cm)
|
|
|
What are the common features of the remaining 1/3 of NHLs?
|
Symptoms related to the involvement of extra-nodal sites (eg, skin, stomach, or brain)
|
|
|
What are the signs of lymphocytic leukemias?
|
Signs and symptoms related to suppression of normal hematopoiesis by tumor cells in bone marrow
|
|
|
What is the most common plasma cell neoplasm?
|
Multiple Myeloma
|
|
|
What are the characteristic signs of Multiple Myeloma?
|
Bony destruction of the skeleton and pain d/t pathologic fractures
|
|
|
Besides the physical presence of a lymphoid tumor, how else can they affect the patient? Which types have this characteristic?
|
- It can cause symptoms by secretion of circulating factors
- Plasma cell tumors (secretion of whole Abs or Ig fragments) - Hodgkin lymphoma (inflammatory cytokines cause fever) |
|
|
What do some plasma cell tumors release?
|
Secrete whole Abs or Ig fragments
|
|
|
What can Hodgkin Lymphoma release? Implications?
|
Inflammatory cytokines which often cause fever
|
|
|
What are the classes of lymphoid neoplasms?
|
- I: Precursor B-Cell Neoplasms
- II: Peripheral B-Cell Neoplasms - III: Precursor T-Cell Neoplasms - IV: Peripheral T-Cell and NK-Cell Neoplasms - V: Hodgkin Lymphoma |
|
|
What is the Lymphoid Neoplasm to know that is Class I?
|
Precursor B-Cell Neoplasm:
- B-cell Acute Lymphoblastic Leukemia / Lymphoma (B-ALL) |
|
|
What are the Lymphoid Neoplasms to know that are Class II?
|
Peripheral B-Cell Neoplasms:
- Chronic Lymphocytic Leukemia / Small Lymphocytic Lymphoma - Hairy Cell Leukemia |
|
|
What is the Lymphoid Neoplasm to know that is Class III?
|
Precursor T-Cell Neoplasm:
- T-cell Acute Lymphoblastic Leukemia / Lymphoma (T-ALL) |
|
|
What are the Lymphoid Neoplasms to know that are Class IV?
|
Peripheral T-Cell and NK-Cell Neoplasms
- Large Granular Lymphocytic Leukemia - Mycosis Fungoides / Sézary Syndrome - Adult T-Cell Leukemia / Lymphoma |
|
|
What is essential for a diagnosis of Lymphoid Neoplasia?
|
*Histologic examination of lymph nodes or other involved tissues is required for diagnosis
|
|
|
What are the characteristics of the daughter cells derived from the malignant progenitor?
|
Share the same antigen receptor gene configuration and sequence, and synthesize identical antigen receptor proteins (either Igs or TCRs) = MONOCLONAL
|
|
|
What are the characteristics of the cells derived from a normal immune response?
|
POLYCLONAL populations of lymphocytes that express many different antigen receptors
|
|
|
On what basis can you distinguish reactive and malignant lymphoid proliferations?
|
- Reactive = POLYCLONAL proliferation
- Malignant = MONOCLONAL proliferation |
|
|
How can you tell if there is any residual malignant lymphoid cells after therapy?
|
- Identify the unique DNA sequence for the antigen receptor gene rearrangement for the proliferation
- After therapy use it to detect if there is still a small number of residual malignant lymphoid cells |
|
|
What is the usual distribution of lymphoid tumors at diagnosis? Exceptions?
|
- Usually they are widely disseminated by spread through lymphatics and peripheral blood
- Hodgkin Lymphomas are sometimes restricted to one group of lymph nodes - Marginal Zone B-Cell Lymphomas are often restricted to sites of chronic inflammation |
|
|
How does the spread of Hodgkin Lymphoma compare to NHL?
|
- HL: spreads in orderly, contiguous pattern
- NHL: spreads widely early in course in less predictable fashion |
|
|
For what kind of lymphoma is staging most useful? Why?
|
More useful for Hodgkin Lymphoma because it spreads in an orderly, contiguous, predictable pattern
|
|
|
What antigens are primarily T-cell associated?
|
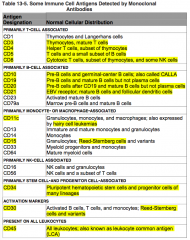
CD3, 4, 5, and 8
|
|
|
Where is CD3 normally distributed?
|
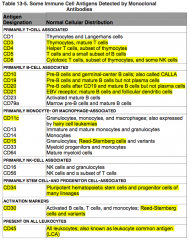
Primarily T-cell associated:
- Thymocytes - Mature T cells |
|
|
Where is CD4 normally distributed?
|
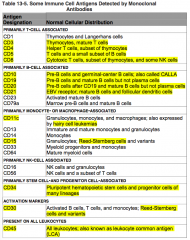
Primarily T-cell associated:
- Helper T cells - Subset of thymocytes |
|
|
Where is CD5 normally distributed?
|
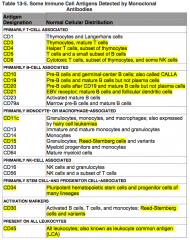
Primarily T-cell associated:
- T cells - Small subset of B cells |
|
|
Where is CD8 normally distributed?
|
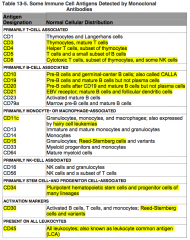
Primarily T-cell associated:
- Cytotoxic T cells - Subset of thymocytes - Some NK cells |
|
|
What antigens are primarily B-cell associated?
|

CD10, 19, 20, 21
|
|
|
Where is CD10 normally distributed?
|
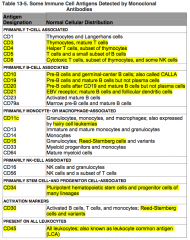
Primarily B-cell associated:
- Pre-B cells - Germinal-center B cells AKA CALLA = common acute lymphoblastic leukemia antigen |
|
|
Where is CD19 normally distributed?
|
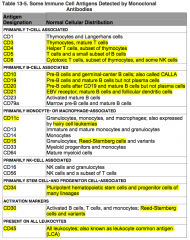
Primarily B-cell associated:
- Pre-B cells - Mature B cells NOT Plasma Cells |
|
|
Where is CD20 normally distributed?
|
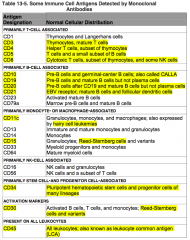
Primarily B-cell associated:
- Pre-B cells after CD19 - Mature B cells NOT Plasma Cells |
|
|
Where is CD21 normally distributed?
|
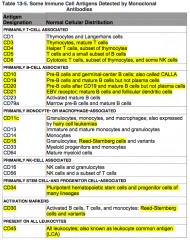
Primarily B-cell associated:
- EBV receptor - Mature B cells - Follicular Dendritic cells |
|
|
What antigens are primarily monocyte or macrophage associated?
|
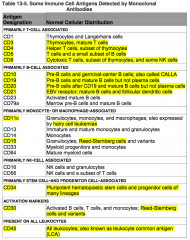
CD11c, CD15
|
|
|
Where is CD11c normally distributed?
|
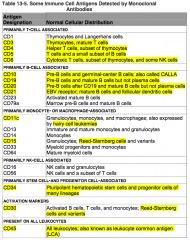
Primarily monocyte or macrophage associated:
- Hairy Cell Leukemias |
|
|
Where is CD15 normally distributed?
|

Primarily monocyte or macrophage associated:
- Reed-Sternberg cells |
|
|
What antigens are primarily stem-cell and progenitor cell associated?
|
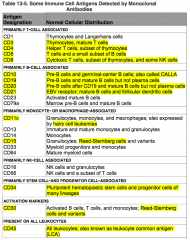
CD34
|
|
|
Where is CD34 normally distributed?
|
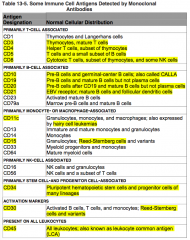
Primarily stem-cell and progenitor cell associated:
- Pluripotent hematopoietic stem cells and progenitor cells of many lineages |
|
|
What antigens are activation markers?
|
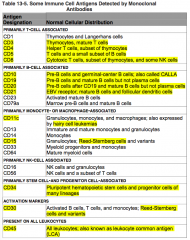
CD30
|
|
|
Where is CD30 normally distributed?
|
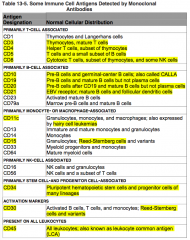
Activation Marker:
- Reed-Sternberg Cells and Variants |
|
|
What antigens are present on ALL Leukocytes?
|
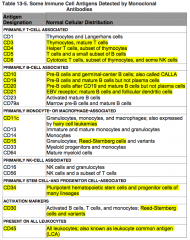
CD45
|
|
|
Where is CD45 normally distributed?
|
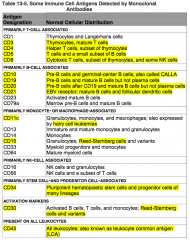
All leukocytes - also known as leukocyte common antigen (LCA)
|
|
|
B-cell Acute Lymphoblastic Leukemia / Lymphoma (B-ALL):
- Cell of origin - Genotype - Salient clinical features |
- Originate from bone marrow precursor B cells
- Diverse chromosomal translocations; t(12;21) involving CBFα and ETV6 (25%) - Predominantly children - Symptoms related to marrow replacement - Pancytopenia - Aggressive |
|
|
T-cell Acute Lymphoblastic Leukemia / Lymphoma (T-ALL):
- Cell of origin - Genotype - Salient clinical features |
- Originates from precursor T cell (often of thymic origin)
- Diverse chromosomal translocations, NOTCH1 mutations (50-70%) - Predominantly adolescent males - Thymic masses and variable BM involvement - Aggressive |
|
|
Hairy Cell Leukemia:
- Cell of origin - Genotype - Salient clinical features |
- Originates in Memory B cells
- No specific chromosomal abnormality - Older males with pancytopenia and splenomegaly - Indolent |
|
|
Small Lymphocytic Lymphoma / Chronic Lymphocytic Leukemia (SLL/CLL):
- Cell of origin - Genotype - Salient clinical features |
- Originates in naive B cells or memory B cells
- Trisomy 12, deletions of 11q, 13q, and 17p - Older adults - BM, lymph node, spleen, and liver disease - Autoimmune hemolysis - Thrombocytopenia in minority - Indolent |
|
|
Adult T-Cell Leukemia / Lymphoma:
- Cell of origin - Genotype - Salient clinical features |
- Originates in Helper T cells
- HTLV-1 pro-virus present in tumor cells - Adults - Cutaneous lesions - Marrow involvement - Hypercalcemia - Occurs mainly in Japan, West Africa, and Caribbean - Aggressive |
|
|
Mycosis Fungoides / Sézary Syndrome:
- Cell of origin - Genotype - Salient clinical features |
- Originates in Helper T cells
- No specific chromosomal abnormality - Adult patients - Cutaneous patches, plaques, nodules, or generalized erythema - Indolent |
|
|
Large Granular Lymphocytic Leukemia
- Cell of origin - Genotype - Salient clinical features |
- Two types: cytotoxic T cell and NK cell
- No specific chromosomal abnormality - Adult patients - Splenomegaly - Neutropenia - Anemia - Sometimes with auto-immune disease |
|
|
Which type of aggressive neoplasm is predominantly in children and the symptoms relate to the marrow replacement and pancytopenia? Cell of origin? Genotype?
|
B-cell Acute Lymphoblastic Leukemia / Lymphoma (B-ALL)
- Originate from bone marrow precursor B cells - Diverse chromosomal translocations; t(12;21) involving CBFα and ETV6 (25%) |
|
|
Which type of aggressive neoplasm is predominantly in adolescent males and presents with thymic masses and variable bone marrow involvement? Cell of origin? Genotype?
|
T-cell Acute Lymphoblastic Leukemia / Lymphoma (T-ALL)
- Originates from precursor T cell (often of thymic origin) - Diverse chromosomal translocations, NOTCH1 mutations (50-70%) |
|
|
Which type of indolent neoplasm is predominantly in older males and presents with pancytopenia and splenomegaly? Cell of origin? Genotype?
|
Hairy Cell Leukemia:
- Originates in Memory B cells - No specific chromosomal abnormality |
|
|
Which type of indolent neoplasm is predominantly in older adults and presents with lymph node, spleen, and liver disease? Cell of origin? Genotype?
|
Small Lymphocytic Lymphoma / Chronic Lymphocytic Leukemia (SLL/CLL):
- Originates in naive B cells or memory B cells - Trisomy 12, deletions of 11q, 13q, and 17p - Also can have auto-immune mediated hemolysis and thrombocytopenia in a minority |
|
|
Which type of aggressive neoplasm is predominantly in adults from Japan, W. Africa, and Caribbean and presents with cutaneous lesions, BM involvement, and hypercalcemia? Cell of origin? Genotype?
|
Adult T-Cell Leukemia / Lymphoma:
- Originates in Helper T cells - HTLV-1 pro-virus present in tumor cells |
|
|
Which type of indolent neoplasm is predominantly in adults and presents with cutaneous patches, plaques, nodules, or generalized erythema? Cell of origin? Genotype?
|
Mycosis Fungoides / Sézary Syndrome
- Originates in Helper T cells - No specific chromosomal abnormality |
|
|
Which type of neoplasm is predominantly in adults and presents with splenomegaly, neutropenia, and anemia, and sometimes accompanied by auto-immune disease? Cell of origin? Genotype?
|
Large Granular Lymphocytic Leukemia
- Two types: cytotoxic T cell and NK cell - No specific chromosomal abnormality |
|
|
What is the more common type of Acute Lymphoblastic Leukemia / Lymphomas (ALLs)? What is it composed of?
|
85% are B-ALLs which are composed of immature B (pre-B) cells
The rest are T-ALLs which are composed of immature T (pre-T) cells |
|
|
What is the common presentation of B-cell Acute Lymphoblastic Leukemia / Lymphomas (B-ALL)?
|
Childhood acute "leukemias"
|
|
|
What is the common presentation of T-cell Acute Lymphoblastic Leukemia / Lymphomas (T-ALL)?
|
Adolescent males with thymic "lymphomas"
|
|
|
What is the most common cancer of children?
|
Acute Lymphoblastic Leukemia / Lymphomas (ALLs)
|
|
|
Why must you distinguish ALL from AML? How do their symptoms compare? Treatments?
|
- Must distinguish d/t differing responses to chemotherapy
- They can cause identical signs and symptoms |
|
|
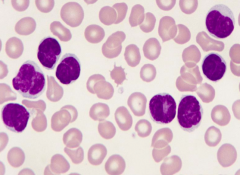
What is the morphological appearance of Acute Lymphoblastic Leukemia / Lymphoma (ALL)?
|
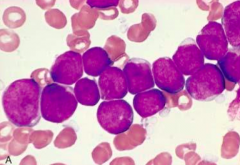
- Variably condensed chromatin
- Small nucleoli - Scant cytoplasm |
|
|
What are the favorable prognostic markers for Acute Lymphoblastic Leukemia / Lymphoma (ALL)?
|
- Age 2-10 y
- Low white cell count - Hyperploidy - Trisomy of chromosomes 4, 7, and 10 - Presence of t(12;21) |
|
|
What are the poor prognostic markers for Acute Lymphoblastic Leukemia / Lymphoma (ALL)?
|
- Age <2 y (assoc. of infantile ALL w/ translocations involving the MLL gene)
- Presentation in adolescence or adulthood - Peripheral blood blast counts > 100,000 (= high tumor burden) - t(9;22) = Philadelphia chromosome |
|
|
What are the implications of the t(9;22) translocation?
|
- Creates a fusion gene that encodes a constitutively active BCR-ABL tyrosine kinase
- Stronger activity than when seen in CML |
|
|
What is the immunophenotype of Chronic Lymphocytic Leukemia / Small Cell Lymphocytic Lymphoma (CLL/SLL)?
|
Pan-B cell markers:
- CD19 and CD20 - CD23 and CD5* *marker found on a small subset of normal B cells |
|
|
What are poor prognostic factors for Chronic Lymphocytic Leukemia / Small Cell Lymphocytic Lymphoma (CLL/SLL)?
|
- Tumors with unmutated Ig segments (putatively of naive B-cell origin) are more aggressive
- Presence of deletions of 11q and 17p - Lack of somatic hyper-mutation - Expression of ZAP-70 (protein that augments signals produced by Ig receptor) |
|
|
If a patient has CD5+ B cells, what is the diagnosis based on amount?
|
- High count: Chronic Lymphocytic Leukemia (CLL)
- Too low to merit diagnosis of CLL = "monoclonal B cells of undetermined significance" (MBUS) |
|
|
Besides poor prognostic factors, what can cause a decreased patient survival in patients with Chronic Lymphocytic Leukemia / Small Cell Lymphocytic Lymphoma (CLL/SLL)?
|
Tendency of CLL/SLL to transform to more aggressive tumors
|
|
|
What is the characteristic presentation of Hairy Cell Leukemia?
|
- Middle aged white males
- Median age of 55 y |
|
|
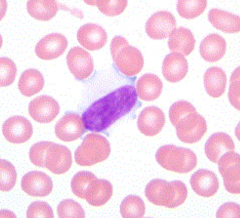
What is the reason for the name "Hairy Cell" leukemia?
|
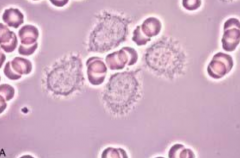
Leukemic cells have fine hair-like projections that are best recognized under the phase-contrast microscope
|
|
|
Which type of neoplasm is associated with a "dry tap"? What does this mean?
|
- Hairy cell leukemia
- These cells are enmeshed in an ECM composed of reticulin fibrils, therefore they can't be aspirated and are only seen in BM biopsies |
|
|
What are the immunophenotypical findings characteristic of Hairy Cell Leukemia?
|
Bright co-expression of CD11c and CD22
|
|
|
How do you treat Mycosis Fungoides?
|
- Topical therapy w/ steroids or UV light for early lesions
- Systemic chemotherapy for advanced lesions |
|
|
What is the variant of Mycosis Fungoides we should know?
|
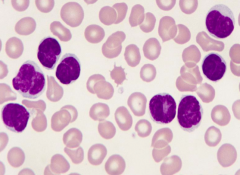
Sézary syndrome - lymphocytes have "cerebriform" nuclei w/ multiple delicate folds, causing the nucleus to have a "brain-like" morphology and distinct powdery chromatin
|
|
What neoplasm is characterized by lymphocytes that look like brains d/t their "cerebriform" nuclei w/ multiple delicate folds?
|
Sézary Syndrome - variant of Mycosis Fungoides
|
|
|
What are the predominant cell changes in Large Granular Lympocytic Leukemia?
|
- Neutropenia
- Anemia |
|
|
What are the variants/types of Large Granular Lymphocytic Leukemia?
|
- Cytotoxic T cell origin
- NK cell origin |
|
|
What disorders are in increased incidence with Large Granular Lymphocytic Leukemia?
|
Rheumatologic disorders
|
|
|
How severe of a disease is Large Granular Lymphocytic Leukemia? Cause of morbidity?
|
- Indolent course
- Associated cytopenias are the source of the most morbidity |
|
|
How severe of a disease is Adult T-Cell Leukemia / Lymphoma? Cause of morbidity?
|
Most:
- Rapidly progressive disease - Fatal within months to 1 year despite aggressive chemotherapy Less commonly, the tumor involves only the skin and follows a more indolent course like Mycosis Fungoides |
|
|
What infection can affect Adult T-Cell Leukemia / Lymphoma symptoms?
|
- HTLV-1 infection
- Sometimes give rise to a progressive demyelinating disease of the CNS and spinal cord |
|
|
What is a lymphocytosis?
|
Absolute lymphocyte count of >4000 / µL
|
|
|
What clues do you have to differentiate a benign (reactive) cause of lymphocytosis from a neoplastic lymphocytosis (>4000/µL)?
|
- Clinical scenario
- Morphology - Duration - WBC count - Peripheral blood smear |
|
|
What are the general features of benign / reactive lymphocytosis?
|
- Transient
- Usually do not exceed lymphocytes > 10,000 / µL - Heterogenous appearing lymphocytes (vary in size and cytoplasm) |
|
|
What are the general features of malignant lymphocytosis?
|
- Chronic (>6 months)
- Can have extremely elevated lymphocytes (>10,000/µL) - Monotonous appearing lymphocytes (similar size and cytoplasm) |
|
|
What conditions are associated with reactive lymphocytoses?
|
Infectious:
* Infectious mononucleosis d/t Epstein-Barr Virus (EBV) - Cytomegalovirus (CMV) - Hepatitis - Varicella - Adenovirus - Toxoplasmosis - Pertussis Transient stress lymphocytosis (may be most common cause of elevated lymphocytes in hospitalized patients; rapidly reverse within hours) - Trauma - Myocardial infarctions - Seizures |
|
|
What are the infectious causes of reactive lymphocytoses?
|
* Infectious mononucleosis d/t Epstein-Barr Virus (EBV)
- Cytomegalovirus (CMV) - Hepatitis - Varicella - Adenovirus - Toxoplasmosis - Pertussis |
|
|
What is the most common cause of elevated lymphocytes in hospitalized patients? Course?
|
Transient Stress Lymphocytoses:
- Trauma - Myocardial infarctions - Seizures (Rapidly reverses within hours) |
|
|
What are the features of lymphocytes in Infectious Mononucleosis?
|
Distinctive morphology and referred to as "atypical" or "variant" lymphocytes
- Heterogenous - Large - Abundant, lightly basophilic cytoplasm - Cell / cytoplasm encroaches on neighboring RBCs Scattered forms w/ more basophilic (blue) cytoplasm and dispersed chromatin, representing IMMUNOBLASTS, may also be observed |
|
|
What do immunoblasts represent?
|
- A lymphocyte that has been activated by an antigen, which will further undergo clonal expansion to increase the number of lymphocytes capable of binding to that antigen
- Seen in response to EBV-infected B cells |
|
|
How can you make a presumptive diagnosis of infectious mononucleosis?
|
Based on peripheral blood smear exam if it meets these 3 criteria:
1) >50% mononuclear cells in the differential (monocytes and lymphocytes) 2) marked lympcytic heterogeneity 3) >10% reactive lymphocytes (>10/100 leukocytes) |
|
|
How do you confirm a diagnosis of infectious mononucleosis?
|
Monospot test: identification of heterophil antibodies
|
|
|
What are the neoplastic proliferations of mature lymphocytes?
|
- Chronic Lymphocytic Leukemia (CLL)
- Hairy Cell Leukemia - Splenic Marginal Zone Lymphoma - Large Granular Lymphocytic Leukemia - Adult T-cell Leukemia (ATLL) - Sézary Syndrome (Some lymphomas may become peripheralized or leukemic and show a lymphocytosis) |
|
|
What are the similarities of these neoplasms?
- Chronic Lymphocytic Leukemia (CLL) - Hairy Cell Leukemia - Splenic Marginal Zone Lymphoma - Large Granular Lymphocytic Leukemia - Adult T-cell Leukemia (ATLL) - Sézary Syndrome |
- Neoplastic proliferations of mature lymphocytes
- Not all present with elevated lymphocyte counts, though abnormal lymphocyte morphology is certainly observed in the majority of these |
|
|
What should you do i there is unexplained lymphocytoses, particularly when persistent in nature?
|
Flow Cytometry
|
|
|
What is the function of flow cytometry in determining an unexplained lymphocytoses?
|
- It will identify what the predominant cell type is, as morphology does not allow a definite distinction between T cells, B cells, or NK cells
- By definition, it will show evidence of clonality either by immunphenotypic aberrancy or light chain restriction |
|
|
What would be a sign of clonality in flow cytometry?
|
- Immunophenotypic aberrancy: abnormal antigen expression, such as CD5 on B cells
- Light chain restriction: kappa or lambda-restricted populations |
|
|
What would a reactive expansion show on flow cytometry?
|

Admixture of kappa and lambda expressing B cells and CD4(+) and CD8(+) T cells
|
|
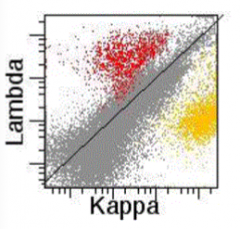
What does this histogram show?
|
Reactive, polyclonal B cell population in a lymph node
- Red = lambda-expressing B cells - Yellow = kappa-expressing B cells |
|

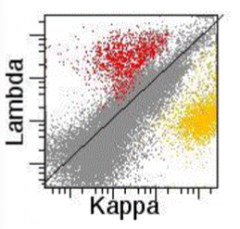
What does this histogram show?
|

Neoplastic, monoclonal B cell population in a lymph node
- Blue = lambda-expressing B cells - Red = T cells (which don't express light chains) |

