![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
22 Cards in this Set
- Front
- Back
|
What is the Rate limiting step for Heme synthesis?
What is an important cofactor for this step? |
Rate limiting = ALA synthase
converts Glycine + succinyl coA --> ALA (alpha amino levulinate). Cofactor = pyridoxal-phosphate (PLP) |
|
|
What is the function of heme in the body?
What are the 3 major components of Hemoglobin? |
Heme (F): globins (CO, O2, CO2), bile salts, oxidase/catalase, CYP-450 (ETC)
Heme + Iron + Globin = Hemoglobin = Life |
|
|
What toxic effects are caused by a build up of ALA and how is this prevented?
|
ALA is a neutrotoxin (similar to GABA). It also builds up ROS in cells.
Levels are controlled by rapid conversion into HEME precursors (PBG, Hydroxymethylbilane, etc.) |
|
|
Name a tetrapyrrole that is in a linear form (Hint: one of the intermediates in the heme synthesis pathway)?
What happens if Uroporphyrinogen III cosynthase enzyme is deficient? |
Hydroxymethylbilane (from the coming together of 4 PBGs).
If UPG III cosynthase is deficient, HMB will preferentially make UPG I and coprophrynogen I (which build up and lead to toxic effects) |
|
|
Each molecule of heme has how many molecules of Iron?
How is heme synthesis regulated? |
Each Heme --> 4 molecules of Iron
Heme synthesis regulated by Feedback Inhibition (heme suppresses feedback of ALA synthase). |
|
|
What are three examples of non-porphyria disease states?
|
1. X-linked sideroblastic anemia, 2. Lead poisonin, 3. Hepatorenal Tyrosenemia
|
|
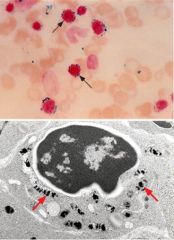
What is shown in the image above? What disease does it correspond to?
|
Ringed sideroblasts (mitochondria laden with iron the encircle nuclei of erythroid precursors).
Found in X-linked Sideroblastic anemia (ALA Synthetase II deficiency, causing buildup of precurosors and iron. MICROCYTIC, HYPOchromic anemia. |
|
|
What is the difference between ALA synthase I and ALA synthase II deficiency?
What is PLP deficiency treated with? |
ALA Synthase I = non-specific, in all cells and incompatible with life.
ALA Synthase II= erythroid specific, causes X-linked anemia syndrome. PLP= pyridoxal-6-Phosphate, cofactor for ALA synthase. Doesn't work well without it --> anemia. Treat with PYRIDOXINE. |
|
|
How does Lead Poisoning cause anemia?
What are signs of Pb poisoning? |
Causes MICROCYTIC anemia. Pb inhibits Ferrochelatase step (proto IX --> Heme). It can also inhibit ALA dehydratase (causing ALA to buildup and damage cells).
Signs = Abd cramping, neuropathy, cognitive dysfunction |
|
|
What is the defect in Hepatorenal Tyrosinemia?
|
AR mutations in fumarylacetoacetate hydrolase gene (enzyme important for tyrosine metabolism). Lack of enzyme leads to buildup of succinylacetone which INHIBITS ALA dehydratase.
Causes ALA to build up --> neurotoxic effects, can't reach dev. milestones, causes liver (jaundice, hepatomegaly) and kidney abnormalities. Patients smell like boiled cabbage. |
|
|
What is the result of overproduction of porphyrins in the Blood? In the Liver? Bone marrow?
What are the 2 most common symptoms associated with porphyrias? |
2 most common sxs = skin and nervous system (neuropathy, mental changes, absent reflexes)
↑ Porphyria in: Blood --> rxn with sunlight causing skin lesions. Liver & Bone marroq --> acute neurologic sxs |
|
|
You should be suspicious of porphyria in what type of patient?
|
Typically young/middle age women with multiple conditions that don't respond to conventional treatments (back pain, headache, GI problems). Histrionic personalities + drug seeking behavior. Can present later in life with seizures.
|
|
|
What is the most common pattern of inheritance in Porphyrias?
|
Most common =Autosomal dominant (most retain 50% of normal enzyme).
Less common = Auto recessive in which total loss of enzyme. |
|
|
What is the only type of porphyria in which you will not see elevated Porphobilinogen (PBG) in the urine?
|
ALAD (ALA Dehydratase deficiency Porphyria)
*Extremely rare and presents in CHILDHOOD (unlike the other Porphyrias). Acute intermittent attacks (abd pain, peripheral neuropathy, etc.) |
|
|
What is the only type of porphyria in which there is an Autosomal Recessive inheritance pattern?
What is the most prominent symptom? |
Congenital Erythropoietic Porphyria- rare, occurs in childhood.
life threatening. Defective UPG cosynthase cause HMB to shunt down UPG I pathway and accumulation of tetrapyrrole (which is found in pigment) is very reactive to light. Patients can have cutaneous skin lesions when exposed to light (photosensitivity). |
|
|
What is the second most common Porphyria overall?
What is the deficiency and how is it triggered? |
AIP (Acute Intermittent Porphyria). Deficiency in Porphobilinogen Deaminase (so PBG builds up).
Causes neurovisceral attacks (abd pain, peripheral neuropathy), triggered by drug rxn, starvation, or body stress. (also ETOH and smoking) |
|
|
What is the most common form of porphyria and what is it's inheritance pattern?
What sxs do patient's present with and how are they treated? |
PCT (porphyria cutanea tarda). Defect in Uroporphyrinogen decarboxylase (buildup in UPGIII).
Patients have blistering skin lesions (when exposed to sun). Improper heme formation causes Fe buildup in liver (like a hemochromatosis, these patients need phlebotomy treatment). *starts in mid-life, M > F |
|
|
What type of porphyria is thought to have been the artistic motivation for the creation of "vampires"? Why?
|
Hereditary coproporphyria. Deficiency of coproporphyrinogen oxidase (leads to buildup of CPIII).
Patients develop burns/scars related photosensititvity. They can become mentally unstable & have attacks (less frequent than AIP). Rx. phlebotomy and disease can be exacerbated by garlic. |
|
|
What is the defect in Variegate Porphyria? What region is it most seen in?
|
Variegate --> defect in Potoporpyrinogen oxidase (build up of a porphyria intermediate).
Associated with photosensitivity and/or Neuropsych manifestations. South Africa = high incidence (may have to do with Sickle Cell prevalence) |
|
|
What is the defect in Erythropoietic Protoporphyria?
What is it treated with? |
Inherited deficiency of ferochelatase. Build up of protoporphyrin IX.
Burning, itching, swelling with sun exposure. Treatment = beta carotene. |
|
|
How should you go about diagnosing porphyria?
|
Have a high index of suspicion.
Rule out other obvious medical causes. Obtain PBG level. If elevated, withdraw precipitating factors and being Heme therapy asap. During this time do confirmatory tests and genetic studies. Check blood, urine, and stool samples. |
|
|
What is the "gold standard" of diagnosing acute porphyrias?
What is the only known therapy available for Porphyria in the US? What does it NOT work for? |
Mutation analysis (also helps family know if they should be tested)
Panhematin (heme injection), addresses heme deficiency in these patients. Also decreases levels of ALA and PBG (by repressing ALA synthase)--less sxs. Not indicated in PCT! |

