![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
152 Cards in this Set
- Front
- Back
- 3rd side (hint)
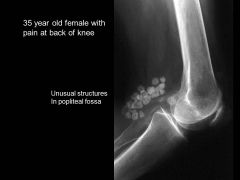
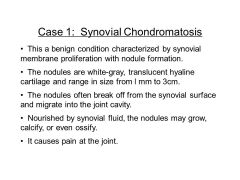
VERY TOUGH QUESTION
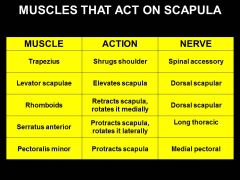
What are the 5 muscles that act directly on the scapula? Hints: 1. shrugs shoulders 2. levitates scapula 3. retracts scapula (medially rotate) winding up for punch 4. often stabbed/ injured during knife fights, then cant reach forward (protract/ lateral rotate) 5. only one PECTORAL muscle attach to scapula. |

|
|
|
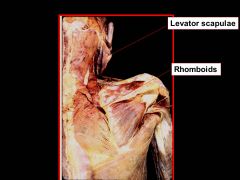
The LEVATOR SCAPULAE, TRAPEZIUS, and RHOMBOIDS all ELEVATE the scapula (Shrugs/ hangcleans) . What innervates them?
|
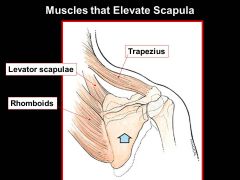
TRAPS= CRANIAL NERVE 11 (SPINAL ACCESSORY NERVE)
Levator scapulae= DORSAL SCAPULAR Rhomboids= DORSAL SCAPULAR N |
|
|

The SUPERIOR & INFERIOR TRAPEZIUS and SERRATUS ANTERIOR muscles ELEVATE & LATERALLY ROTATE (abduct) the scapula (swing your shoulder joint around and up like you're about to spike a ball) What innervates them?
|
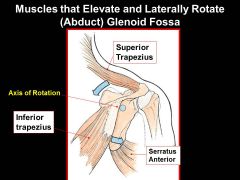
Trapezius= SPINAL ACCESSORY NERVE
Serratus anterior= LONG THORACIC NERVE |
|
|
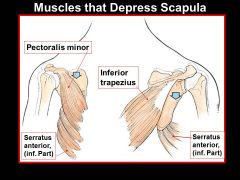
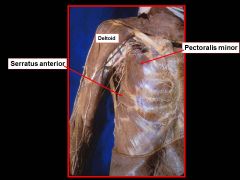
The PECTORAL MINOR, INFERIOR TRAPEZIUS, and SERRATUS ANTERIOR all DEPRESS the scapula. What nerve innervate these?
|

pec minor= medial pectoral nerve
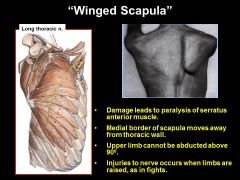
traps= spinal accessory nerve XI ser. ant.= LONG THORACIC NERVE ** damage to serratus anterior= winged scapula |
|
|
|
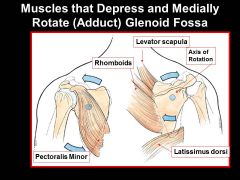
Which muscles DEPRESS & MEDIALLY ROTATE (ADDuct) the glenoid fossa? Which nerve is related to that?
|
|
|
|

The PEC MINOR and SERRATUS ANTERIOR muscles PROTRACT the scapula. (Like you are throwing a PUNCH/ protract forward) Nerve?
|
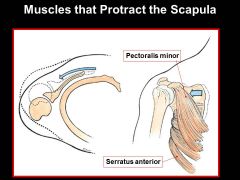
pec minor= MEDIAL PECTORAL NERVE only!!
(pec major has 2... medial and lateral nerve) Serratus anterior= LONG THORACIC NERVE |
|
|
|
The RHOMBOIDS, middle TRAPEZIUS, and LATISSIMUS DORSI all RETRACT the scapula. Which nerves innervate these?
|
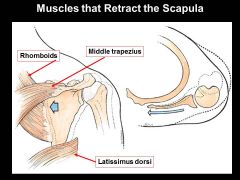
rhomboid= DORSAL SCAPULAR (C5)
trapezius= SPINAL ACCESSORY NERVE (CN XI) latissimus dorsi= THORACODORSAL* |
|
|

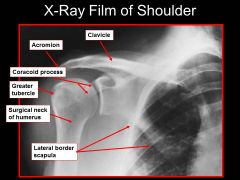
On this xray, where is the lateral border of the scapula? What else can you ID?
|
|
|
|
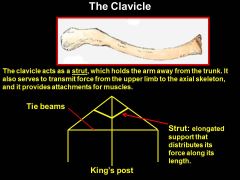
The clavicle is the most frequently broken bone in the body. What happens if you fracture your clavicle? Why?
|
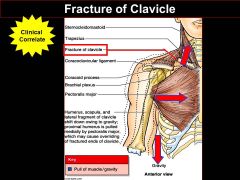
Tenting occurs & upper limb is brought in to trunk of body. Muscles always maintain certain tone, even at rest. With no opposing force from clavicle, position of arm and distal clavicle are still acted on by muscles.
|
|
|
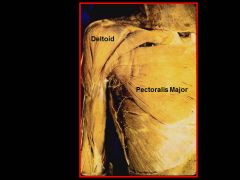
The pec major does NOT ACT ON SCAPULA!!! What does? (that is directly behind it?)
|
can depress, medially rotate (adduct), and PROTRACT
|
|
|
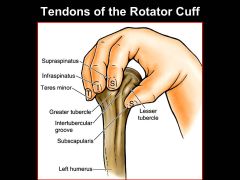
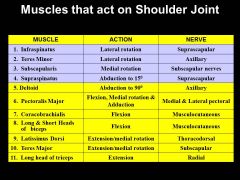
Based on where the:
1. Subscapularis ("subscap" n.) 2. Suprascapularis ("SUPRAscap" n.) 3. Infraspinatus, (also suprascapular n.) 4. Teres Minor (axillary n.) of the rotator cuff are all located, predict the actions based on where they are pulling from... |
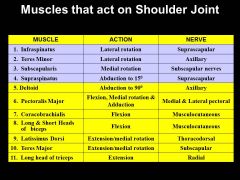
1. sub= medial rot.
2. supra= abduction to 15* (deltoid does to 90*) 3. infra= lateral rot. 4. teres minor= lateral rot. |

|
|
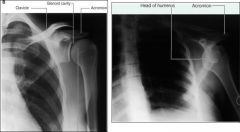
What sort of motion can cause this xray on the right?
|
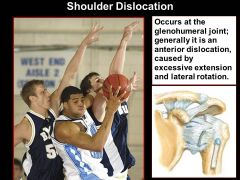
DISLOCATED SHOULDER
|
|
|
|
If you have bursitis in your shoulder, which movement becomes painful? (happens to baseball pictures a lot)
|
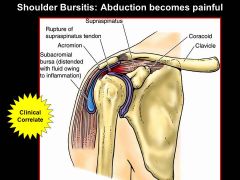
|
|
|

Shoulder separation and shoulder dislocation are two separate things. Which ligament can be torn during a shoulder separation?
|
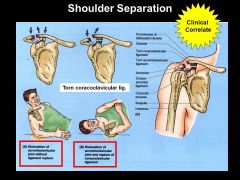
in shoulder separation, articulation between ACROMION and CLAVICLE are compromised
|
|
|
|
Which three muscles FLEX the shoulder joint, and which three EXTEND the shoulder joint?
|

|
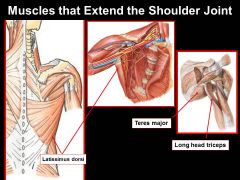
**NOTE only the LONG HEAD of TRICEP extends to the scapula & works on shoulder joint**
|
|
|
Which major muscle ABDucts the the shoulder joint, and which ADDucts the shoulder joint?
|

|

|
|

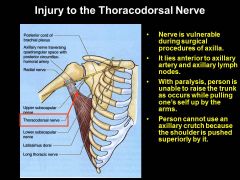
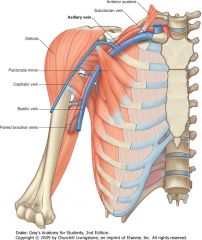
Why do you need to be really careful when removing lymph nodes for breast cancer surgery?
|
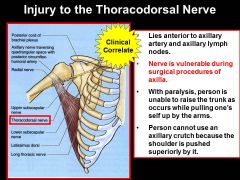
thoracodorsal nerve innervates lat dorsi (unable to extend upper limb) and long throacic nerve innervates serrates anterior (unable to lift arm above horizonatl). BE CAREFUL NOT YO DAMAGE THESE!!
|
|
|
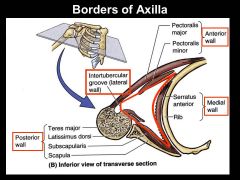
Most of the area inside the axilla (aka armpit) consists of fat to protect which two structures? (1. main innervation, 2. primary source of blood to upper limb)
|
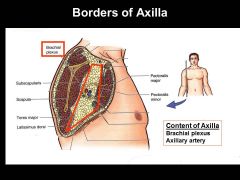
Brachial plexus and axillary artery
|
|
|
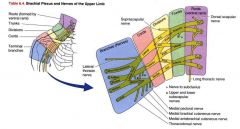
brachial plexus is innervated from C5-8, and T1 supplies motor & sensory info to the upper arm. What is the only exception to the upper arm & chest & back muscles that are not innervated by the brachial plexus?
|
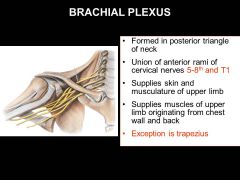
THE TRAPEZIUS
|
|
|
|
What is the primary source of blood to the upper limb?
|
AXILLARY ARTERY
|
|
|
|
WHat type of information do the ventral rami and dorsal rami contain? Where do they come from?
|
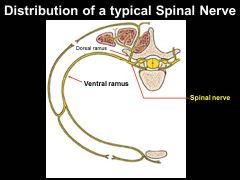
The contain mixed SENSORY & MOTOR information since the combine at the spinal nerve and both originate from the dorsal(sensory) rootlet and ventral(motor) rootlet,
|
|
|
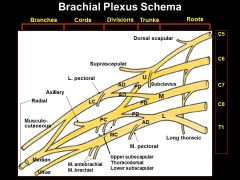
Where are the:
roots, trunks and divisions located? Chords located? Branches (nerves) located? |
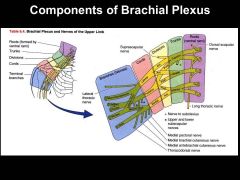
1. Neck
2. AXILLA 3. arm |
|
|

If someone just had this type of injury, why would you check to see if they can:
1) ABDUCT / LATERALLY ROTATE their arm, and 2.) FLEX& SUPINATE their elbow? Why might you see them with a medially rotated and partially hyperextended limb after a wipeout? |
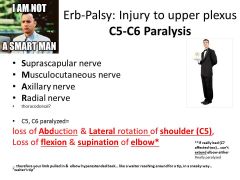
Superior brachial plexus injury!
Testing the myotomes! Action of opposite muscles are left unchecked with C4-C5 paralysis |

Injuries to the upper roots of the brachial plexus (C5 and C6) are the most common types of injuries--resulting in a condition known as Erb-Duchenne Palsy. It affects especially the suprascapular, axillary, and musculocutaneous nerves, which causes paralysis of the rotator cuff muscles, biceps, brachialis, coracobrachialis, and deltoid. It also knocks out the upper and lower subscapular nerves, denervating subscapularis and teres major. It knocks out most of the lateral pectoral nerve, but the majority of pect major is innervated by medial pectoral nerve, so it is only weakened. After this injury, the upper limb hangs limply, medially rotated by an unopposed latissimus and pectoralis major muscles, and pronated due to a loss of biceps. So, the limb is constantly adducted and medially rotated. However, the limb can no longer be abducted because both supraspinatus, which initiates abduction, and deltoid, which allows for complete abduction, have been denervated.
As far as extension and flexion go: Extension occurs through the actions of the triceps which is innervated by the radial nerve. This nerve should still be intact. Flexion of the arm is not totally lost if biceps brachii and coracobrachialis are denervated, because pectoralis major is not completely lost. |
|

Why would you make sure Stallone can make a fist, and still have feeling in his hand, after a violent yank on his arm upwards? |
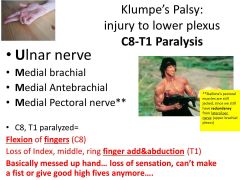
Inferior brachial plexus nerve injury! |

|
|
|
Injury to which nerve would lead to:
-inability to extend forearm & digits -"Wrist Drop" - typically happens with damaged to spiral groove of humerus - looks like a flexed wrist due to unapposed tonus of flexor muscles/ gravity |
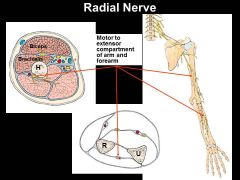
INJURY TO RADIAL NERVE!!
|

|
|
|
Injury to which nerve would lead to:
-paralyzed serratus anterior muscle - "winged scapula" --> medial border moves away from thoracic wall -often injured during knife fights -upper limb cant be lifted higer than 90* |
INJURY TO LONG THORACIC NERVE!
|
|
|
|
Injury to which nerve is related to:
-fractures of surgical neck of humerus or shoulder dislocations -inability to ABDuct the upper limb, wasting of shoulder contour, area of anesthesia - paralyzed deltoid muscle |
INJURY TO AXILLARY NERVE!
|

|
|
|
Injury to which nerve is related to:
-paralyzed lattisimus dorsi - surgical procedures of armpit -unable to use crutches, since they can't pull themselves up -near axillary artery and axillary lymph nodes |
INJURY TO THORACODORSAL NERVE!
|
|
|
|
Why is the profunda brachial artery useful during surgery?
|

can tie off brachial artery during surgery and still get bloodflow.
|
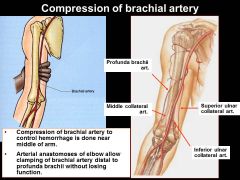
note: location of how subclavian artery transitions from axilla--> brachial--> once it passes teres major
|
|
|
Which artery in the upper arm is an important point for shoulder surgery, where blood can still travel/ anastamosis as long as the ligation is above it?
|
SUBscapular artery
|

|
|
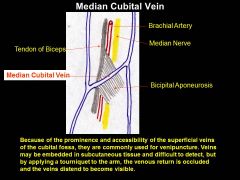
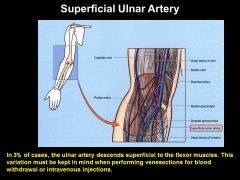
Most of the time, blood draws are from the median cuboidal vein... If you try to draw blood from someone's forearm, and they start bleeding like crazy, what happened?
|
You might have hit the SUPERFICIAL ULNAR ARTERY by accident
|
|
|

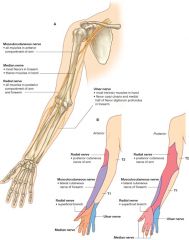
Which nerve senses pain in the tip of the fingers?
|
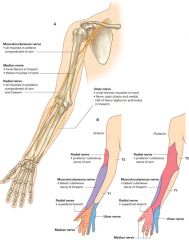
Median Nerve!
|
|
|
Which three nerves can be damaged with certain fractures of the humerus?
|
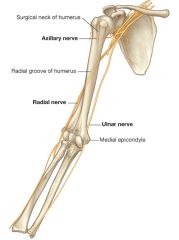
Axillary, Radial, and Ulnar
*posterior circumflex humeral artery can be damaged at surgical neck as well |
Axillary- deltoid
Radial- all posterior muscles Ulnar- hand, flexor carpi ulnaris, medial half of flexor digitorum profundus |
|

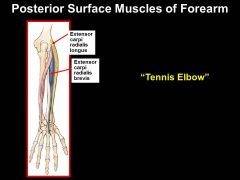
Radial Nerve Entrapment and "Tennis Elbow" both cause pain on supination. What are the differences between the two causes?
|
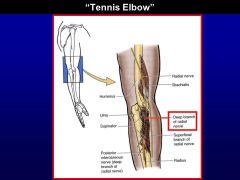
Radial nerve entrapment – deep branch that does all extensors of the forearm
- hard to extend the wrist, also impacts grip because the tendons for gripping/shaking someones hand more efficient when your hand is extended than flexed Tennis elbow – inflammation of the tendons of the extensor carpi radialis longus and brevis no impact on the radial nerve, while radial nerve entrapment is more serious and involves the nerve – supinator (inflammation deep to the supinator) the motion that causes these are very similar repetitive motions |
|
|

Why might cyclists have trouble picking up a credit card in between their fingers? What happens when the ULNAR nerve is compressed/ damaged on the medial side of the forearm?
|
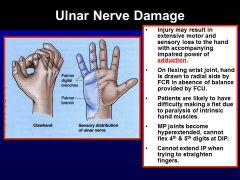
Clawed hand
Thumb is fine, cannot adduct, can flex pointer and middle, lost ability to abduct and adduct the digits, test this by holding a credit card between their fingers Can be caused by cyclists, compressing against the handle bars |
|
|

Median nerve injury in ELBOW region results in what?
|
PAPAL sign hand!!
loss of flexion of the PIP and DIP joints of the 2nd and 3rd digits: FDS and FDP affected. Ability to flex MP joints of these digits is also affected: lumbricals 1 & 2 affected. |

|
|

The traps muscles can help evaluate for the ACCESSORY NERVE (XI) function by checking for which motion?
|
(hang-cleans/ shoulder shrugs) can check fxn of accessory nerve XI.
It attaches to spine of scapula |
|
|
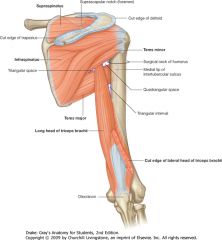
Which two important structures go through the quadrangular space & triangular interval space?
** Think about what would happen if you IMPINGE on any of these structures... |
|
Quadrangular space syndrome
Hypertrophy of the quadrangular space muscles or fibrosis of the muscle edges may impinge on the axillary nerve. Uncommonly, this produces weakness of the deltoid muscle. Typically it produces atrophy of the teres minor muscle, which may affect the control that the rotator cuff muscles exert upon shoulder movement. |
|
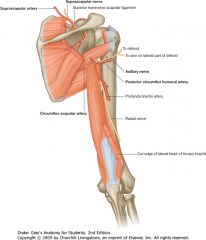
Note relation of Axillary artery braches to the pec minor.
What are the six different branches of the AXILLARY ARTERY? |

|
In the clinic
Imaging the blood supply to the upper limb When there is clinical evidence of vascular compromise to the upper limb, or vessels are needed to form an arteriovenous fistula (which is necessary for renal dialysis), imaging is required to assess the vessels. Ultrasound is a useful tool for carrying out a noninvasive assessment of the vessels of the upper limb from the third part of the subclavian artery to the deep and superficial palmar arteries. Blood flow can be quantified and anatomical variants can be noted. Angiography is carried out in certain cases. The femoral artery is punctured below the inguinal ligament and a long catheter is placed through the iliac arteries and around the arch of the aorta to enter either the left subclavian artery or the brachiocephalic trunk and then the right subclavian artery. Radiopaque contrast agents are injected into the vessel and radiographs are obtained as the contrast agents pass first through the arteries, then the capillaries, and finally the veins. page 698 0 page 699 In the clinic Trauma to the arteries of the upper limb The arterial supply to the upper limb is particularly susceptible to trauma in places where it is relatively fixed or in a subcutaneous position. Fracture of rib I As the subclavian artery passes out of the neck and into the axilla, it is fixed in position by the surrounding muscles to the superior surface of rib I. A rapid deceleration injury involving upper thoracic trauma may cause a first rib fracture, which may significantly compromise the distal part of the subclavian artery or the first part of the axillary artery. Fortunately, there are anastomotic connections between branches of the subclavian artery and the axillary artery, which form a network around the scapula and proximal end of the humerus; therefore, even with complete vessel transection, the arm is rarely rendered completely ischemic (ischemia is poor blood supply to an organ or a limb). Anterior dislocation of the humeral head Anterior dislocation of the humeral head may compress the axillary artery resulting in vessel occlusion. This is unlikely to render the upper limb completely ischemic, but it may be necessary to surgically reconstruct the axillary artery to obtain pain-free function. Importantly, the axillary artery is intimately related to the brachial plexus, which may be damaged at the time of anterior dislocation. In the clinic Subclavian pinch-off syndrome There are a number of routes through which central venous access may be obtained. The "subclavian route" and the jugular routes are commonly used by clinicians. The subclavian route is a misnomer that remains the preferred term in clinical practice. In fact, most clinicians enter the first part of the axillary vein. There are a number of patients that undergo catheterization of the subclavian vein/axillary vein. Entering the subclavian vein/axillary vein is a relatively straightforward technique. The clavicle is identified and a sharp needle is placed in the infraclavicular region aiming superomedially. When venous blood is aspirated, access has been obtained. This route is popular for long-term venous access, such as Hickman lines, and for shorter-term access where multiple-lumen catheters are inserted (e.g., intensive care unit). The subclavian vein/axillary vein is also the preferred site for insertion of pacemaker wires. There is, however, a preferred point of entry into the vein to prevent complications. The vein should be punctured in the midclavicular line or lateral to this line. The reason for this puncture site is the course of the vein and its relationship to other structures. The vein passes anterior to the artery, superior to the first rib and inferior to the clavicle as it courses through the thoracic inlet. Beneath the clavicle is situated the subclavius muscle. Should the puncture of the vein enter where the subclavius muscle is related to the axillary vein, the catheter or wire may become kinked at this point. Moreover, the constant contraction and relaxation of this muscle will induce fatigue in the line and wire, which may ultimately lead to fracture. A fractured pacemaker wire or a rupture in a chemotherapy catheter can have severe consequences for the patient. |
|
WHY is it so important we understand the anastamosis of the axillary artery, and which one is the biggest? Who the hell cares? Why do I need to memorize this?
|
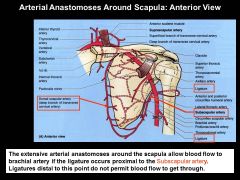
this is why you're not screwed and don't lose your arm if your shoulder is injured.
|
|
|
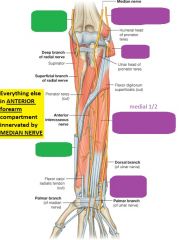
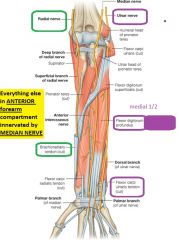
DONT FU*K THIS UP!!!!
VERY VERY IMPORTANT!!! ***All muscles in the ANTERIOR (aka flexor) compartment of the FOREARM are innervated by the MEDIAN nerve EXCEPT for which three? |
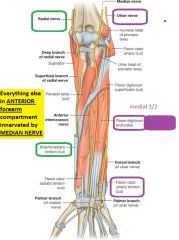
Ulnar nerve:
1. FLEXOR CARPI ULNARIS 2. FLEXOR DIGITORUM PROFUNDUS (medial 1/2 of forearm aka outside closest to body) Radial nerve: 3. BRACHIORADIALIS (in posterior compartment techincally) but located anterior laterally and acts as accessory flexor of of elbow joint when mid pronated*** lol handjobs... lol. |
|
|

VERY VERY IMPORTANT! DON'T F*CK THIS UP OR F*CKING FORGET IT!!! Which very important nerve innervates all the POSTERIOR compartments of the arm and forearm? and would be really bad with this type of injury? Why would you see WRIST DROP?
|
***THE RADIAL NERVE INNERVATES ALL OF THE MUSCLES IN THE POSTERIOR COMPARTMENTS OF THE ARM AND FOREARM. ***
Remember the radial nerve innervates the extensors! |
Radial nerve injury in the arm
The radial nerve is tightly bound with the profunda brachii artery between the medial and lateral heads of the triceps brachii muscle in the radial groove. If the humerus is fractured, the radial nerve may become stretched or transected in this region leading to permanent damage and loss of function. This injury is typical (Fig. 7.70) and the nerve should always be tested when a fracture of the midshaft of the humerus is suspected. The patient's symptoms usually include wrist drop (due to denervation of the extensor muscles) and sensory changes over the dorsum of the hand. |
|
|
Which very important nerve allows for you to have opposable thumb movement?
|
Recurrent branch of the median nerve. it innervates the thenar eminance of the thumb!
|
|
|
|
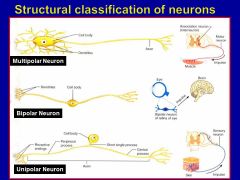
Dorsal ROOTLETS & dorsal root ganglia are always made of this type of neuron?
|
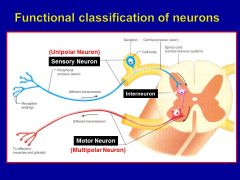
Unipolar!! (sensory)
**RAMI on the other hand, are MIXED MOTOR AND SENSORY |
|
|
|
Cancer of the nervous system, tic doloreux ("Suicide disease"/ trigeminal neurolagia/ extreme pain of face) and MS are all associated with pathology of what type of nervous tissue?
|
SUPPORT CELLS of PNS and CNS.
**know that they are there and they are important |
|
|
|
Whats the difference between:
-nerve -nerve fiber -neuron |
Neuron= cover by ENDOneurium
Nerve fiber= cover by PERIneurium/ fascicle Nerve= cover by EPIneurium |

|
|
|
Which dermatones are involved with?
Top of shoulders? Nips? xiphoid process? Belly button? Groin/ "speedo bathing suit" area? |

|
The supraclavicular nerves (lateral, intermediate, and medial) arise from the cervical plexus and cross the clavicle (where they may be rolled against the bone). They supply the skin over the shoulder and, because they arise from the same roots (C3, 4) as the phrenic nerve, diaphragmatic inflammation is one cause of pain referred to the shoulder.
|
|
|
Which ligament provides the strength and support for the axis?
|
Transverse ligament of axis!
|
|
|
|
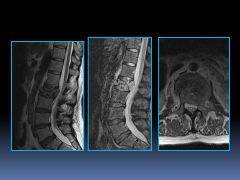
The outer ANNULUS FIBROUS is made out of what type of collagen that is the tough outer layer? and the inner NUCLEUS PULPOSUS is what type of collagen that provides the shock absorption?
|
Annulus fibrous= TYPE I
Nucleus propulsus= TYPE II (proteoglycans)+ no |
|
|
|
Which layer of the spinal chord contains the CSF? (used for Dx: of menigitis via spinal tap)
|
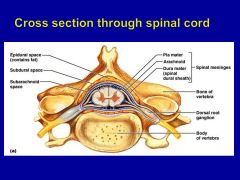
The SUB-ARACHNOID SPACE!
|
|
|
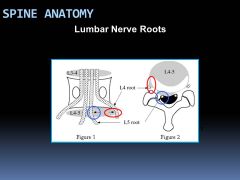
What is special about disc herniations in the LUMBAR spine?
|

Disc herniations at the LUMBAR spine injure the nerve passing by , NOT the nerve leaving Remember that at the T and L levels, the nerve leaving corresponds to the SUPERIOR vertebral level. (cauda equana at certain point)
|

** at cervical level, spinal nerve corresponds to INFERIOR disc level of the vertebrae, but since there are 8 spinal chords with only 7 vertebrae, once you hit T1 vertebrae, the spinal nerve leave out T1/T2 foramen
|
|

A woman riding a mountain bike on a rough trail hits a rut and is thrown from the bike. Her upper arm hits a tree, fracturing the humerus just above the insertion of the teres major muscle. Later, during examination, it is noted that she cannot extend her forearm at the elbow or hand at the wrist. Which nerve must have been injured?
|
The radial nerve spirals around the posterior surface of the shaft of the humerus in the radial groove. It is endangered by humeral fractures distal to the surgical head of the humerus, which is a pretty good description of this patient's injury. The loss of extension at the elbow and wrist also implies damage to the radial nerve--remember, the radial nerve innervates the extensors!
The axillary nerve is damaged by humeral fractures at the surgical neck--an injury to this nerve would lead to an inability to abduct the arm. The median nerve is located near the distal end of the humerus--if this nerve was injured in an accident, a patient might have trouble flexing the wrist. The ulnar nerve is located near the medial epicondyle of the humerus--an injury to this nerve would lead to muscular deficits in the hand. Finally, the musculocutaneous nerve is not usually damaged with humeral fractures. |
|
|
|
A football player suffers a herniated (ruptured) intervertebral disk in his neck. The disk compresses the spinal nerve exiting through the intevertebral foramen between the 5th and 6th cervical vertebrae. Which spinal nerve is affected?
|
C6 spinal nerve
|
There are 7 cervical vertebrae and 8 pairs of cervical nerves. So, the nerve from the C1spinal cord segment emerges above the C1 vertebra, the nerve from the C2 region of the spinal cord emerges above the C2 vertebra, and so on. This means that if a disk presses the nerve between the C5 and C6 vertebrae, it will be compressing the C6 nerve, which emerges above the C6 vertebra. So, what happens with the C8 nerve? Since there is no 8th cervical vertebra, the C8 nerve emerges above the T1 vertebra. Then, the nerve that comes out below theT1 vertebra is the T1 spinal nerve, and the nerve that emerges below the T2 vertebra is the T2 spinal nerve. The same holds true for the lumbar and sacral regions. Just remember: In the cervical region, a spinal nerve comes out above the vertebra of the same number, but in the thoracic, lumbar, and sacral regions, the spinal nerve comes out below the vertebra of the same number.
|
|
|
A man has a herniated intervertebral disk between the fourth and fifth lumbar vertebrae. If this disk compresses the spinal nerve in the intervertebral foramen immediately posterior to this disk, which spinal nerve would be affected?
|
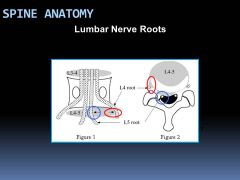
L5
|
This question asks you to think about the lumbar region where the spinal nerve comes out below the vertebra of the same number. If a disc herniates between L4 and L5, it will be impinging on the L5 spinal nerve. This is because the L4 nerve lies immediately below the L4 pedicle, above the herniating disc. However, the L5 nerve roots are already proceeding laterally toward the L5 intervertebral foramen, so it is usually caught by the herniating L4/5 disc. In the cervical region, the spinal nerves emerge above the vertebrae of the same number, while in the thoracic, lumbar and sacral region the spinal nerves emerge below the vertebrae of the same number. As well, cervical roots course nearly directly laterally to exit. So, although the result is similar (herniating discs compress the lower numbered vertebrae of the pair), the reasons are different for cervical regions and lower levels. Make sure to keep this difference straight, because it's an important one to remember!
|
|
|
Kyphosis is an accentuated or abnormal curvature of which region of the spine?
|
Thoracic spine
|
Kyphosis is an abnormal increase in the thoracic curvature of the vertebral column. An abnormal increase in lumbar curvature due to anterior sway of the pelvis is called lordosis. (Women develop temporary lordosis during pregnancy to compensate for the change in their normal line of gravity.) Finally, scoliosis is an abnormal lateral curvature of the spine accompanied by a rotation of vertebrae.
|
|

During a spinal tap, as the spinal needle is being inserted, which ligaments would it pass through on its way to the subarachnoid space?
|
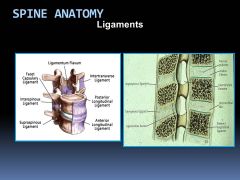
To insert a needle into the subarachnoid space, the needle must pass through three ligaments: the supraspinous ligament, interspinous ligament, and ligamenta flava.
|
To insert a needle into the subarachnoid space, the needle must pass through three ligaments: the supraspinous ligament, interspinous ligament, and ligamenta flava. The anterior longitudinal ligament is located along the anterior surfaces of all vertebral bodies--it lies directly posterior to the thoracic and abdominal viscera. The denticulate ligaments are paired ligaments that separate the dorsal and ventral rootlets. They are not disturbed during a lumbar puncture. Ligamentum nuchae is located at the nape of the neck--not even close to where you would perform a spinal tap. The posterior longitudinal ligament is a ligament on the posterior surfaces of the vertebral bodies. Although it is located in the vertebral canal, it is not penetrated by the needle during a spinal tap.
It's important to know the anatomy involved with a lumbar puncture! Look at the clinical case for further information about this important topic. |
|
|
According to Dr. Kalantar, what is the most important muscles you need to move out of the way for surgery?
|
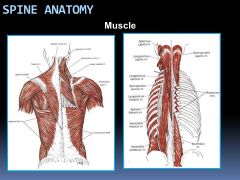
Maltifidous
|
|
|

Because of their structure and interconnections, which veins are especially important in the metastatic spread of cancer?
|
Internal vertebral venous plexus
|
|
|
|
In the lumbar spine, the L4 nerve root sleeve exits ______(above or below?) the pedicle of L4 and at the _________ (top or bottom?) of the intervertebral foramen.
|
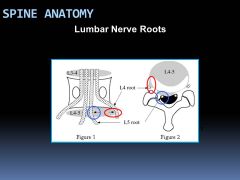
BELOW the pedicle of L4 and at the TOP of the intervertebral foramen
Remember, in the lumbar region, spinal nerves exit below the vertebra with the same number. So, the L4 nerve exits below the L4 vertebra. The spinal nerves also exit at the top of the intervertebral foramen. |
|
|

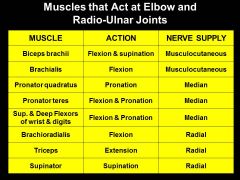
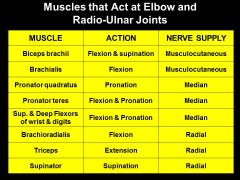
The BICEPS BRACHII and BRACHIALIS muscles FLEX the elbow (and SUPINATE radio-ulnar joint). Which nerve innervates both of these muscles in the ANTERIOR (flexor) compartment?
|
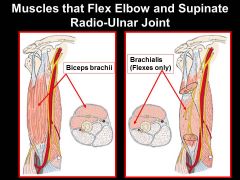
Biceps brachi= MUSCULOCUTANEOUS NERVE
brachialis= MUSCULOCUTANEOUS NERVE |
|
|

Young teenage boys probably have very well developed forearm muscles for certain activities...
The 1. BRACHIORADIALIS 2. PRONATOR TERES 3. SUPERFICIAL FLEXORS 4. DEEP FLEXORS all responsible for FLEXing elbow and PRONATing radio-ulnar joint. What are they all innervated by? (remember brachioradialis is special) |
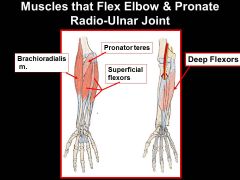
Brachioradialis= RADIAL NERVE**
pronator teres= median nerve sup & deep flexors of wrist & digits= median nerve |

|
|

The PRONATOR QUADRATUS pronates the radio-ulnar joint (lower forearm). Which nerve should the inglorious bastards severe so pronation of the wrist is no longer possible?
|
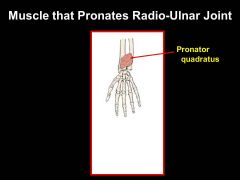
pronator quadratus= MEDIAN nerve
|
|
|
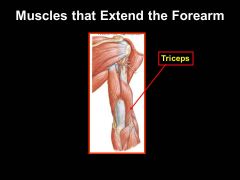
The TRICEPS are responsible for EXTENDING the forearm. What nerve innervates them?
|
Triceps= RADIAL NERVE
|
|
|
The SUPINATOR muscle supinates (omg!) the radio-ulnar joint. ("righty tighty"). What nerve innervates this muscle?
|
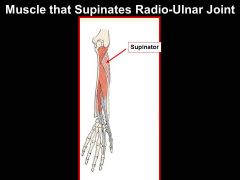
supinator= RADIAL NERVE
|

|
|

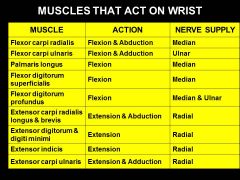
There are a SHITLOAD of muscles that FLEX the wrist joint (these are only the top two layers). Which ones are innervated by something OTHER THAN the MEDIAN NERVE that help to FLEX the WRIST joint?
|
1. Brachioradialis
2. Flexor Carpi Ulnaris 3. Flexor digitorum profundus |

|
|
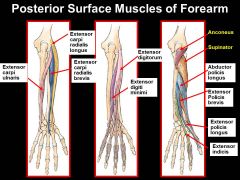
Out of all these muscles on the posterior forearm (all innervated by the RADIAL NERVE BTW), which ones are the tendons involved in a condition that make it painful to supinate your wrist when their tendons get irritated?
|
|
|
|
The flexors of the wrist (mostly median nerve) are in which compartment of the forearm, and the extensors are in what compartment (radial nerve)?
|

|
|
|
|
What's the difference between INTRAMEMBRANEOUS OSSIFICATION and ENDOCHONDRAL OSSIFICATION? Which one is in areas for flat bones?
|
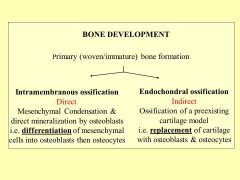
Differentiation vs. replacement
IM= short bones/ flat bones/ skull |
|
|
This type of growth occurs pre-natally. What type of ossification is this describing?
|
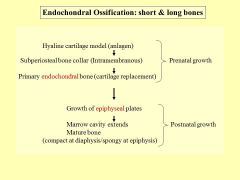
ENDOCHONDRAL OSSIFICATION
|

|
|
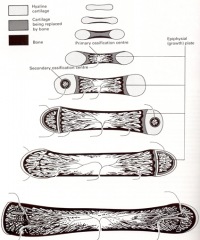
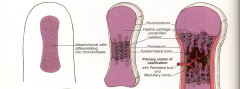
What type of ossification is this?
How is the PRIMARY ENDOCHONDRAL BONE formed and where is the primary ossification center? |
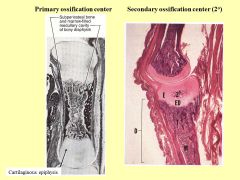
Endochondral (indirect ossification)
|
Endochondral (indirect ossification)
i. Occurs by ossification and eventual replacement of hyaline cartilage ii. Steps 1. Embryonic mesenchymal condensation; differentiate into chondrocytes 2. Small hyaline cartilage molecule = analgen 3. Extracellular matrix calcifies (chondrolcalcin) this forms a “subperiosteal bone collar” a. So this means that this process is dependent upon intramembranous ossification to begin ossification 4. Diffusion of nutrients to cartilage tissue is interrupted 5. Chondrocytes undergo hypertrophy until they burst 6. Cartilage undergoes degeneration-creates a cavity 7. Blood vessels appear at this site of degenerating cartilage (Angiogenic Inhibiting Factor removed!) a. This is known as a periosteal bud bringing osteoprogenitor cells, bone marrow cells, and osteoclasts 8. Degenerating cartilage is resorbed (removed by chondroclasts) but leaves collagen matrix behind 9. Pervascular mesenchymal cells become osteogenic (BMP or Osteogenin) 10. Osteoblasts deposit osteoid remnants on collagen 11. Osteoid becomes mineralized (osteonectin and osteocalcin). a. THIS IS PRIMARY ENDOCHONDRAL BONE 12. The space created by cartilage resorption is now the primary marrow cavity 13. Primary endochondral bone is soon resorbed by osteoclasts and chondroclasts 14. New or secondary (adult) bone is laid in ways similar to intramembranous development and the resultant marrow space is now called a secondary (adult) marrow cavity. iii. While these series of events occur near the site of endochondral ossification center, cartilage tissue further away from this center continues to proliferate, grow interstitially (CGF, Growth Hormone) and add to the endochondral cartilage model. iv. Diaphysis is the primary ossification center. |
|
|
Where do we see INTRAMEMBRANEOUS (direct ossification/ mineralization of matrix by osteoblasts) occurring?
|
Occurs in areas of vascularized mesenchyme including:
1. Flat bones (membrane bones) 2. Growing short bones 3. Periosteal bone collar of long bones (bone thickening) |
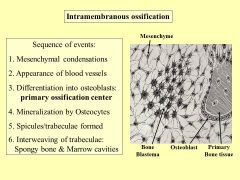
ii. Steps:
1. Mesenchymal cells aggregate 2. Blood vessels appear in this aggregate 3. Ostegenicity is invoked and osteoblast are formed 4. Osteoblasts secrete osteoid which soon mineralizes 5. Matrix lamellae are formed and these fuse to form trabeculae and spicules 6. Trabeculae interweave to form spongy bone, or go on to form the elaborate compact bone architecture |
|
|
When the growth plate closes, what is the only remaining cartilage left?
|
Articular cartilage
|
|
|
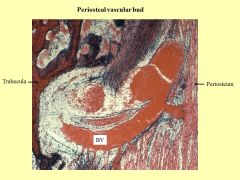
Periosteal buds are an important part of developing what part of the long bones?
|
The DIAPHYSEAL (middle)
aka Primary ossification center occurs prenatally |

|
|
|
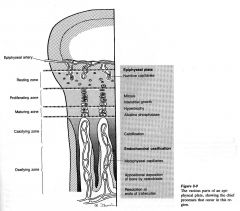
Growth plates (regulated by GH/IGF1) are also called what?
|

|
|
|
|
How do growth plates close? Which cartilage is no longer present in adult bone?
|

|
|
|

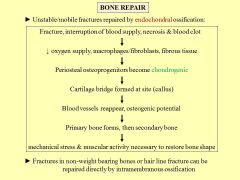
How would the Fx repair be different between a hairline or non weightbearing fx versus a displaced fracture?
|
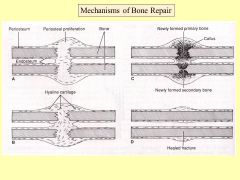
Unstable= ENDOCHONDRAL OSSIFICATION (chondrogenic)
hairline= INTRAMENBRANEOUS ossificaiton |
|
|
|
What are the three types of (more or less) immoveable joints?
|

|
|
|
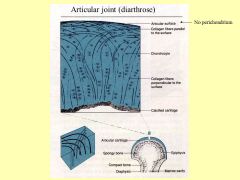
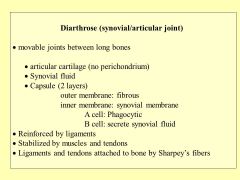
For Diarthrose (synovial/articular) joints, what do the A cells do and what do the B cells do? What type of collagen is the articular cartilage made from?
|
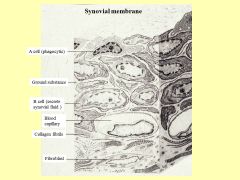
A phagocytose
B secrete proteoglycans TYPE II collagen!! |
|
|
|
Whats the difference between a tendon and ligament?
|

|
|
|
|
How do adult long bones grow in diameter?
|
subperiosteal (intramembraneous) deposition of bone tissue.
|
|
|
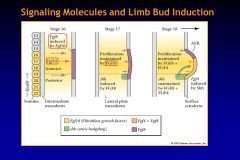
How does Fgf10 work to signal limb bud induction?
|

|

|
|
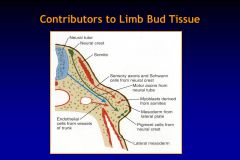
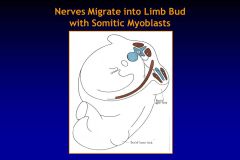
think about how nerves get into each muscle... how the hell does that happen?
|
hypomere is what forms the muscles of the limbs.
|
There are 3 key tissues that come together to form the limb: (1) Somatopleuric lateral plate
mesoderm forms bones, tendons, ligaments and vasculature, (2) somites form muscle and (3) neural crest cells form pigment cells and Schwann cells. Remember that somites differentiate into four types, the hypomere comes from myotome and hypomere is what forms the muscles of the limbs. As groups of muscles diverge from hypomere, their motor innervation will follow, which results in complicated plexuses of nerves that supply our limbs. |
|
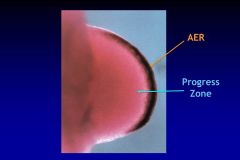
Maintaing limb development and actually forming the limb tissues are the result of two Mesenchymal-Epethelial Rxns. What is the APICAL ECTODERMAL RIDGE and the PROGRESS ZONE, and what are they responsible for?
|
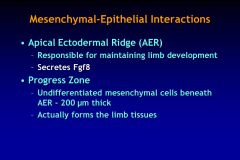
AER maintains limb development and tells us which segment of the limb needs to be formed, while
mesenchyme in the progress zone determines if a forelimb or hindlimb forms. |
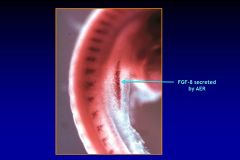
The length of time cells spend in the progress zone determines if they will form proximal or distal components of the limb
|
|
|
Which genes control the proximal/ distal development of limb buds?
|
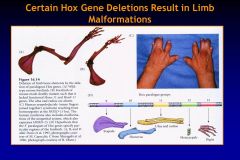
HOX GENES!!
|

|
|
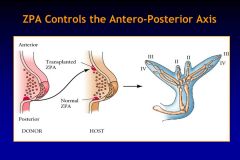
What da faq does ZPA mean?!?
|

|
|
|
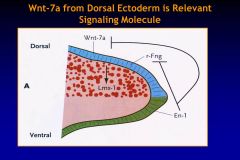
What da faq does Wnt-7a from the dorsal ectoderm do?
|

|

|
|

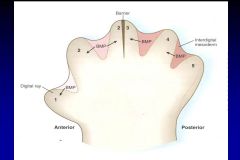
How do we make fingers?!?!? weeee!
|
APOPTOSIS-- induced by gradient of Bone Morphogenetic Protein (BMP)
|
|
|
|
Why do our knees and elbows bend in different directions?
|
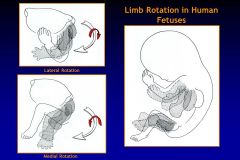
upper limb rotates 90 LATERALLY
lower limb rotates 90 MEDIALLY |
|
|
|
What does it mean when your lymph nodes are enlarged and tender?
What if they were enlarged and hard, but not painful?! |
tender/painful= lymph full of bacteria
hard= CANCEROUS |
|
|
|
Tricky: Where would edema/ lymph fluid from the RIGHT leg eventually drain in to?
|
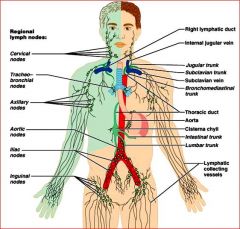
THORACIC DUCT--> all the way --> between L subclavian artery & L jugular vein
|
|
|
|
If Dr. Suarez asks you for the radial nerve and profunda brachii artery, then WHAT FU*KING SPACE SHOULD YOU LOOK FOR THEM?
WHAT IF HE ASKS FOR AXILLARY NERVE AND POSTERIOR CIRCUMFLEX HUMERAL ARTERY AND VEIN?@??! |
?
|
|
|
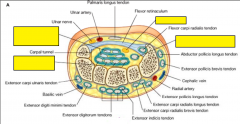
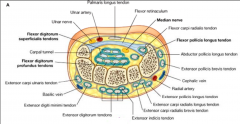
Stare at this for a while... what goes through the carpal tunnel? (Hint 9 tendons and one nerve
|
|
|
|

Which intrinsic muscle of the hand is Neo using to signal you to come closer?
|
LUMBRICALS!
* intrinsic muscle of hand all MEDIAN NERVE remember? |
Originate from tendons of FLEXOR DIGITORUM PROFUNDUS... FLEX MP joint while EXTENDING PIP joint (striaghtening out)
|
|
|
Ventral interossei (and ADDUCTOR POLLICIS) of the hand do what?
|
Ventral/ anterior/ palmar all ADDUCT
|
|
|

Dorsal interossei do what?
|
ABDUCT HAND so you dont cut yoself
|
|
|
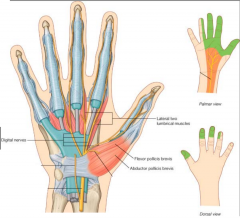
Which nerve in the hand is associated with:
-MOTOR: Thenare eminanace muscles and first two lumbricals -SENSORY: 3 1/2 fingers |
Median nerve
|
Damage to median nerve
• Lesions of median n. occur in two places: forearm and wrist. Most common is where nerve passes through carpal tunnel. • Carpal tunnel syndrome results from any lesion that reduces size of tunnel, e.g., fluid, infection, excessive exercise. • Accidental laceration of the wrist often causes median n. injury. • Paresthesia, hypothesthesia, or anesthesia may occur in lateral three and a half digits. • Progressive loss of coordination and strength in the thumb may occur if cause of syndrome not alleviated. • Person with median n. compression unable to oppose thumb (Thenar eminence muscles affected). • As condition progresses, sensory changes radiate into the forearm and axilla. • Median n. injury in elbow region results in loss of flexion of the PIP and DIP joints of the 2nd and 3rd digits: FDS and FDP affected. • Ability to flex MP joints of these digits is also affected: lumbricals 1 & 2 affected. |
|

Which nerve is associated with:
• Motor via its deep branch to most muscles of hand • Motor to third and fourth lumbricals • Motor to hypothenar muscles • Motor to adductor pollicis muscle • Motor to all interossei muscles • Sensory to one and a half fingers |
ULNAR NERVE
|
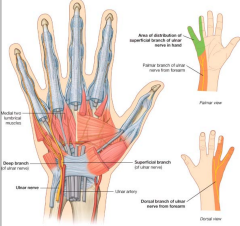
Damage to ulnar nerve.
• Injury usually occurs at four places: 1. Posterior to medial epicondyle of humerus (trauma). 2. Cubital tunnel formed by tendinous arch connecting humeral and ulnar heads of the flexor carpi ulnaris (OT Hazard). 3. At the wrist (trauma). 4. At the hand (cyclist’s palsy). • Injury may result in extensive motor and sensory loss to the hand with accompanying impaired power of adduction. • On flexing wrist joint, hand is drawn to radial side by FCR in absence of balance provided by FCU. • Patients are likely to have difficulty making a fist due to paralysis of intrinsic hand muscles. • MP joints become hyperextended, cannot flex 4th & 5th digits at DIP. • Cannot extend IP when trying to straighten fingers. |
|
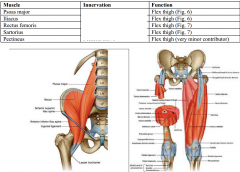
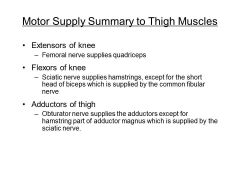
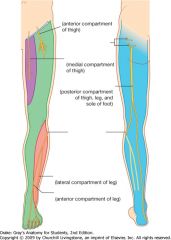
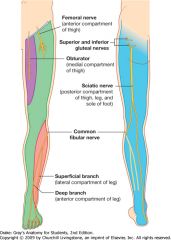
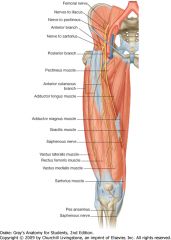
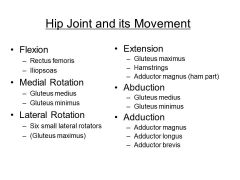
The muscles in the front of your thigh all help lift your thigh for the next step... What are they innervated by?
|
FEMORAL NERVE (for psoas, ant. rami of L1-3)
|
|
|

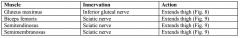
Squats yo... which nerves innervate the Gluteus Maximus, Biceps femoris, semitendonous and semimembranous?
|
SCIATIC NERVE, and (inferior) gluteal NERVE for the maximus
|
|
|

The gluteus maximus helps extend the thigh, however the medial and minimus have another function important for walking... What is going on with someone that "waddles" or has "a dipping gait" when they walk?
|
medius and minumus help ABDUCT the femur at hip joint.
|
Both innervated by GLUTEAL NERVE.
Maximus= inferior |
|
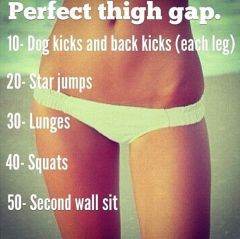
THe muscles on the inside of your thigh gap (Gracilis, Pectineus, Adductor longus, Add. Brevens & Add. magnus) all ADDUCT thigh, and are innervated by what nerve?
|
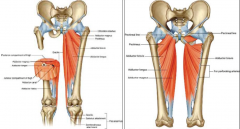
All OBTURATOR NERVE
(except Pectineus= femoral nerve) |
|
|
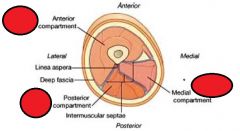
Very important/ easy to remember once you know it! What is the motor supply to the thigh muscles
|
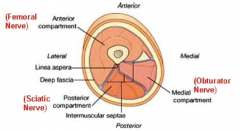
the anterior compartment of thigh contains muscles that mainly extend the leg at the knee joint;
the posterior compartment of thigh contains muscles that mainly extend the thigh at the hip joint and flex the leg at the knee joint; the medial compartment of thigh consists of muscles that mainly adduct the thigh at the hip joint. |
|
|
|
When giving an intramuscular injection in the butt, which area of the butt should you aim for to AVOID HITTING THE SCIATIC NERVE
|
upper left or upper right quadrant of the butt
|
|
|
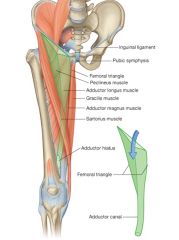
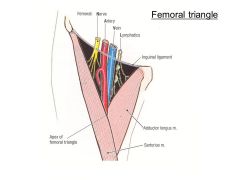
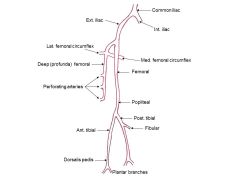
What type of **** will you find inside femoral triangle?
|
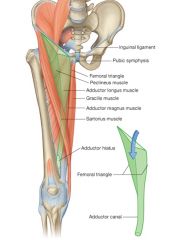
• Femoral sheath: a funnel shaped sleeve of fascia that is continuous superiorly with the transversalis
fascia and the iliac fascia of the abdomen. The sheath is divided into three compartments and contains the following: • Femoral artery: its pulse can be palpated inferior to inguinal ligament, midway between the ASIS and pubic symphysis it is often used by cardiologists to place catheters in vessels around the arch of the aorta and into the coronary arteries to perform angiography and angioplasty • Femoral vein: medial to the artery Catheters can be inserted into the vein to maneuver into the renal veins, the gonadal veins, the right atrium, and the right side of the heart, including the pulmonary artery and distal vessels of the pulmonary tree. It is also possible to access the superior vena cava and the great veins of the neck • Femoral canal: It is an empty space located medial to the location of the vein and mainly contains lymphatic vessels. Femoral hernias are found in this space. • Femoral nerve: is not the sheath, it is located lateral to the sheath. |
Why type of sh*t are you not supposed to find in your groin?Skin and soft tissue – lipoma, sebaceous cyst, sarcoma
Artery – aneurysm of the femoral artery Vein – varix (dilation) of the great saphenous vein or its branches Nerve – neuroma of femoral nerve or its branches Femoral canal – femoral hernia – more common in women Inguinal canal – inguinal hernia (direct or indirect) Psoas sheath – psoas abscess Lymph node enlargement – drains lower abdominal wall, superficial aspects - front and back; lower vagina; part of uterus (cancer); external genitalia; under surface of big toe; anal canal; possibly breast these nodes are often enlarged since minor sepsis and abrasions of the leg are common |
|
|
Which knee ligament is attached to the lateral meniscus? Medial Mensicus?
|

|
There are two menisci in the knee joint: c-shaped cartilages
Medial menisci is attached to capsule of joint and to tibial collateral ligament (medial collateral ligament) Menisci are interconnected anteriorly by a transverse ligament of the knee Lateral meniscus is connected to the tendon of the popliteus muscle Synovial membrane (Fig. 4) The synovial membrane of the knee joint attaches to the margins of the bony articulations and to the superior and inferior margins of the menisci This particular arrangement of the synovial membrane allows for the formation of pouches within the knee joint, i.e., the bursa Bursa are filled with synovial fluid that acts as a “lubricant” around the knee joint; largest is suprapatellar This synovial membrane is separated anteriorly from the patellar ligament by the infrapatellar fat pad The cruciate ligaments hold the femur and tibia together Other bursa around the knee: Subcutaneous prepatellar bursa Deep and subcutaneous infrapatellar bursa Numerous other bursae associate with tendons and ligaments |
|

A sh*itload of muscles flex the knee joint. What are they all innervated by?
|

|
|
|
|
What does the super awesome POPLITEUS MUSCLE in the back of the knee do?
|
UNLOCKS the knee joint by laterally rotating the FEMUR on fixed tibia
|
|
|

When skiing with super tight boots on... you may loose feeling between toe and second digit... what nerve would be compromised in this situation?
|
Deep fibular nerve and/or common nerve is comprimised
|
Other stuff that can happen:
Clinical Correlate of nerves of the leg: • Tibial nerve: it is rarely injured; if it is cut (deep knife wound), there will be motor loss to all flexor muscles in leg and the intrinsic muscles in the sole of the foot; sensory loss on sole of foot • Common fibular nerve: May be damaged as it winds around fibular neck – tight casts; tight bandages; adduction injuries of knee; fibular neck fractures (car bumper); motor loss in anterior and lateral compartments of leg – foot is plantar flexed (foot drop); sensory loss over anterior and lateral sides of leg and dorsum of foot. Accessible for local anesthesia at fibular neck. • Superficial fibular nerve: Chronic ankle sprains may stretch sensory part of nerve and lead to pain on the dorsum of the ankle and foot • Deep fibular nerve: Nerve may be compressed in front of ankle during sports (skiing, running, dancing) and lead to pain in the anterior compartment; “ski boot syndrome”; also from tight fitting running shoes (runners and soccer players). It becomes cutaneous between the toe and second digit. Absence of sensation in this area may indicate that the deep fibular and/or common fibular nerve is compromised. |
|
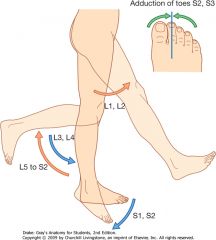
VERY IMPORTANT. Which levels of spinal nerves correlate with what actions?
|

|

Neurological examination of the legs
Some of the commonest conditions that affect the legs are peripheral neuropathy (particularly associated with diabetes mellitus), lumbar nerve root lesions (associated with pathology of the intervertebral discs), fibular nerve palsy, and spastic paraparesis. Look for muscle wasting-loss of muscle mass may indicate loss of or reduced innervation. Test the power in muscle groups-hip flexion (L1, L2-iliopsoas-straight leg raise); knee flexion (L5 to S2-hamstrings-the patient tries to bend the knee while the examiner applies force to the leg to hold the knee in extension); knee extension (L3, L4-quadriceps femoris-the patient attempts to keep the leg straight while the examiner applies a force to the leg to flex the knee joint); ankle plantarflexion (S1, S2-the patient pushes the foot down while the examiner applies a force to the plantar surface of the foot to dorsiflex the ankle joint); ankle dorsiflexion (L4, L5-the patient pulls the foot upward while the examiner applies a force to the dorsal aspect of the foot to plantarflex the ankle joint). Examine knee and ankle reflexes-a tap with a tendon hammer on the patella ligament (tendon) tests reflexes at the L3-L4 spinal levels and tapping the calcaneal tendon tests reflexes at the S1-S2 spinal levels. Assess status of general sensory input to lumbar and upper sacral spinal cord levels-test light touch, pin prick, and vibration sense at dermatomes in the lower limb. |
|
|
|
|
|

Which nerve was the Ravens player aiming for in his tackle, and why is this packers player going to have foot drop?
|
COMMON FIBULAR NERVE INJURY: May be damaged as it winds around fibular neck – tight casts; tight
bandages; adduction injuries of knee; fibular neck fractures (car bumper); motor loss in anterior and lateral compartments of leg – foot is plantar flexed (foot drop); sensory loss over anterior and lateral sides of leg and dorsum of foot. Accessible for local anesthesia at fibular neck. |

|
|

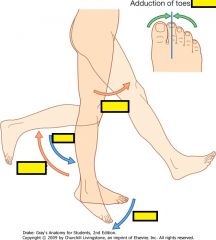
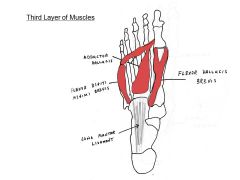
The quadratus planate (lateral plantar nerve/ tibial nerve) pulls on the Flexor digitorum longus to perform what action?
|

Curl your toes in the sand!
|
The second layer of muscles include the 2 long tendons coming down from the leg. Note that 2 small foot muscles (lumbricals and quadratus plantae) originate from the tendons of the flexor digitorum longus. It is the quadratus plantae that is often a test question in our lab practical exam.
|
|

Valley girls have knees bent in (VALGUS KNEES)/ "knock kneed". What does this do to the tracking of the patella?
|
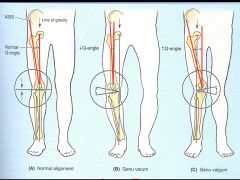
GENU VALGUS promotes LATERAL DISLOCATION of patella in women. Greater LATERAL PULL by quads on the patella - due to wider hips.
|
GENU VARUS= Bow legged, like cowboy (ya dang varmit!!)
|
|
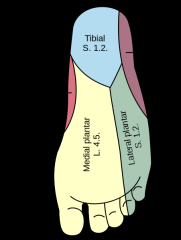
The medial and lateral plantar nerves arise from which nerve?
|
Tibial nerve!
|
|
|

This first later of muscles in the bottom of the foot do what?
|
Spread out your toes!
|
|
|
The muscles that perform the ADDUCTION action lie in which area of the foot?
|
NEXT TO PHALANGES IN DISTAL HALF OF FOOT
|
|
|
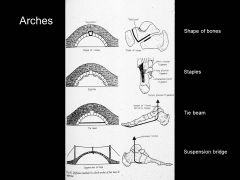
There are lot of ways that the foot is supported and able to bear the weight of our entire body. Think about how some common problems can occur....
What is the cause of most common foot problem in runner (heal pain)? Whats wrong with flat footed people (Pes Planus)? Bunions (Hallux valgus)? |

-Plantar Facititis,
-Pes Planus = calcaneoavicular no longer supports talus - Hallux Valgus= lateral deviation of big toe at 1st metatarsal-phalangeal joint |

|
|
Da faq is going on here?
|
|
|
|
|
|
|
|
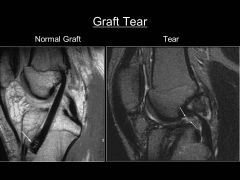
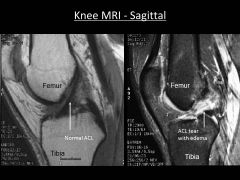
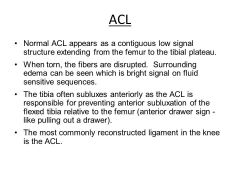
What can fu*k up and ACL graft and cause you to need a secondary ACL reconstruction?
|

|

|
|
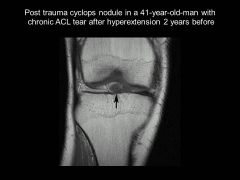
What is the CYCLOPS EYE/ Cyclops syndrome? Why can't this guy extend his knee anymore, and why does he hear "clunking"
|
Cyclops Syndrome after ACL tear.
Cyclops syndrome is one of the specific causes of loss of extension of the knee following anterior cruciate ligament (ACL) reconstruction. The syndrome is manifested by progressive loss of extension associated with pain and an audible clunk at terminal extension caused by a nodule of fibrovascular proliferative tissue usually arising from the graft. The entity has been described recently and has been reported exclusively as a complication of ACL reconstructions. |
|
|
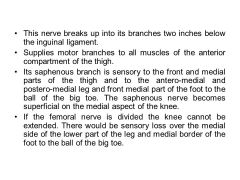
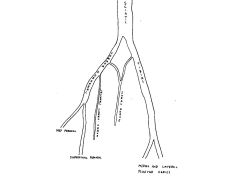
Which nerve is this?
|
Femoral nerve! (L2-L4)
|

Femoral L2 to L4 All muscles in the anterior compartment of thigh; in the abdomen, also gives rise to branches that supply iliacus and pectineus Skin over the anterior thigh, anteromedial knee, medial side of the leg, and the medial side of the foot
|
|

|

Obturator Nerve (L2-L4)
|
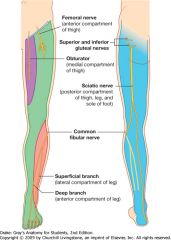
Obturator L2 to L4 All muscles in the medial compartment of thigh (except pectineus and the part of adductor magnus attached to the ischium); also innervates obturator externus Skin over upper medial aspect of thigh
|
|

|
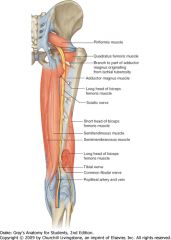
Sciatic Nerve
|
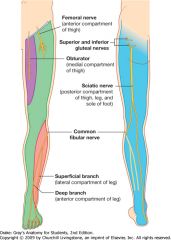
Sciatic L4 to S3 All muscles in the posterior compartment of thigh and the part of adductor magnus attached to the ischium; all muscles in the leg and foot Skin over lateral side of leg and foot, and over the sole and dorsal surface of foot
|
|
|
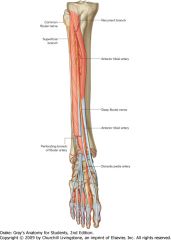
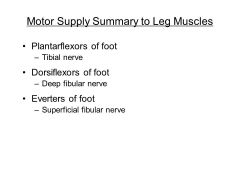
Tibial Nerve
Plantarflex foot |

|
|

|
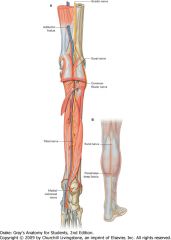
Common Fibular Nerve
|

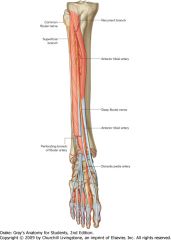
The common fibular nerve originates from the sciatic nerve in the posterior compartment of thigh or in the popliteal fossa (Fig. 6.87A), and follows the medial margin of the biceps femoris tendon over the lateral head of the gastrocnemius muscle and toward the fibula. Here it gives origin to two cutaneous branches, which descend in the leg:
the sural communicating nerve, which joins the sural branch of the tibial nerve and contributes to innervation of skin over the lower posterolateral side of the leg; the lateral sural cutaneous nerve, which innervates skin over the upper lateral leg. The common fibular nerve continues around the neck of the fibula and enters the lateral compartment by passing between the attachments of the fibularis longus muscle to the head and shaft of fibula. Here the common fibular nerve divides into its two terminal branches: the superficial fibular nerve; the deep fibular nerve. |
|
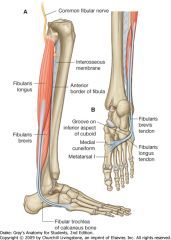
Make Sure you Dissect the cutaneous branches between the 1st and 2nd toes
|
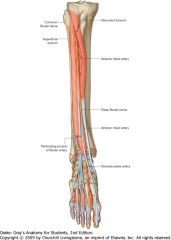
Deep Fibular Nerve! (L5, S1)
(Tibialis Anterior, Extensor Hallucis Longus, Extensor Digitorum Longus, Fibularis Tertius) dorsiflex foot, extend toes |

four muscles in the ANTERIOR COMPARTMENT of the leg-the tibialis anterior, extensor hallucis longus, extensor digitorum longus, and fibularis tertius (Fig. 6.88 and Table 6.9). Collectively they dorsiflex the foot at the ankle joint, extend the toes, and invert the foot. All are innervated by the deep fibular nerve,
|
|
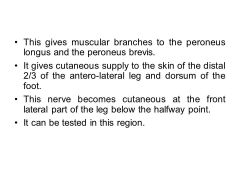
Make Sure you Dissect the cutaneous branch as it piernces in to deep fascia at the front lateral part of the leg below the halfway point
|
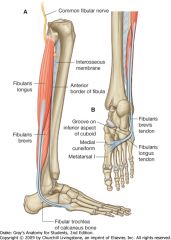
Superficial Fibular nerve! (L5, S1, S2)
(Fibularis Longus, Fibularis Brevis) Everts Foot |

Fibularis longus Upper lateral surface of fibula, head of fibula, and occasionally the lateral tibial condyle Undersurface of lateral sides of distal end of medial cuneiform and base of metatarsal I Superficial fibular nerve [L5, S1, S2] Eversion and plantarflexion of foot; supports arches of foot
Fibularis brevis Lower two-thirds of lateral surface of shaft of fibula Lateral tubercle at base of metatarsal V Superficial fibular nerve [L5, S1, S2] Eversion of foot |
|
|
How do the Superior & infererior gluteal nerve and lumbar plexus relate to one another?
|

|
|
|
Where do these compartments branch from each other off the sciatic nerve?
|
|
|
|

|
|
|
|
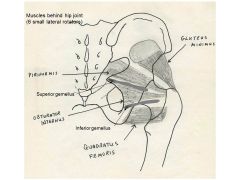
These six muscles
PIRIFORMIS GLUT MINIMUS SUPERIOR GEMELLUS INFERIOR GEMELLUS QUAD FEMORIS OBTURATOR INTERNUS Collectively supply this type of support for hip joint ? |
posterior support (duh)
|
|
|
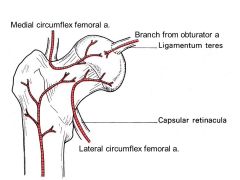
Look at the blood supply of the hip joint... Why do some people need a hip replacement after they fracture their hip?
|
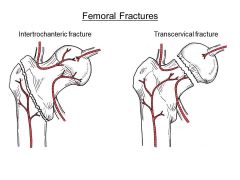
transcervical fx near head means the head will become necrotic...
|
|
|

Whats this? Predict what you might find on MRI
|

|
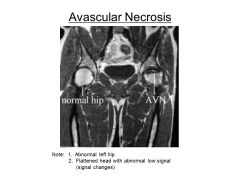
AVN= death of bone & cartilage
MOST COMMONLY INVOLVED: Femoral head Lunate Talus Proximal Scaphoid Humeral Head Vertebral Body |
|
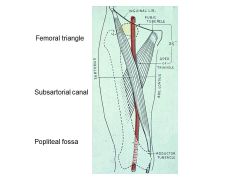
The femoral triangle contains the femoral artery, vein, nerve and sheath... what only structure is not found in the sheath?
|
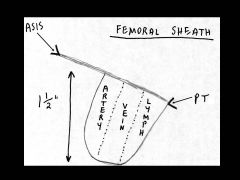
THE FEMORAL NERVE IS NOT FOUND IN THE SHEATH
(it lies lateral next to femoral artery outside sheath) |
|
|
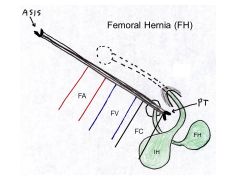
What distiguishes an inguinal hernia from a femoral hernia?
|
The neck of a femoral hernia lies LATERAL to the pubic tubericle
|
|
|
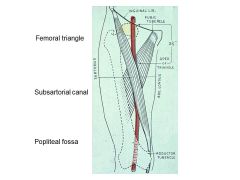
The Femoral artery, Femoral Vein, and saphenous nerve all pass through which canal?
|
HUNTER'S/ SUBARTORIAL CANAL
|
|
|
|
Which muscles surround the popliteal artery in the back of the knee?
|
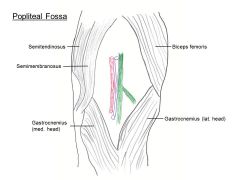
Right knee
|
|
|

A fracture in between what area would not interfere with blood supply to head of femur?
|
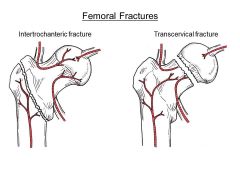
Between greater and lesser trochanters
|
|
|
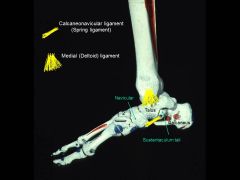
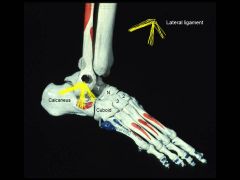
Tearing/ streatching pf which ligament would cause you to be flat footed?
|
Spring ligament!
|
I already tore this one
|
|
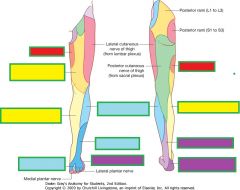
Which area would you check for a lesion in:
Femoral Nerve Obturator Nerve Tibial Nerve Common Fibular Nerve |
the femoral nerve innervates skin on the anterior thigh, medial side of the leg, and medial side of the ankle;
the obturator nerve innervates the medial side of the thigh; the tibial part of the sciatic nerve innervates the lateral side of the ankle and foot; the common fibular nerve innervates the lateral side of the leg and the dorsum of the foot. |

|
|
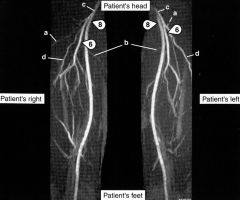
Which area supplies blood to POSTERIOR part of thigh
|
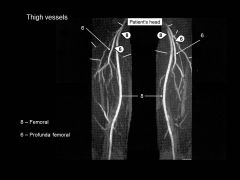
#8- Profunda (Deep) Femoral
|
|
|
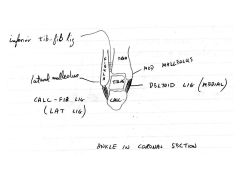
Which ligament of the ankle is SO STRONG it can actually cause a fracture when torn
|
Deltoid (medial) ligament can rip off a chunk of bone along with it.
|
|
|
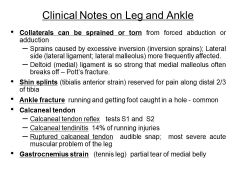
![The ankle can only PLANTAR FLEX AND DORSI FLEX... SO where does inversion and eversion of the foot occur by:
Tibialis (A+ P) / Inversion
Fibularus (Longus + Brevis/ [Eversion]](https://images.cram.com/images/upload-flashcards/08/61/82/3086182_m.jpg)
The ankle can only PLANTAR FLEX AND DORSI FLEX... SO where does inversion and eversion of the foot occur by:
Tibialis (A+ P) / Inversion Fibularus (Longus + Brevis/ [Eversion] |
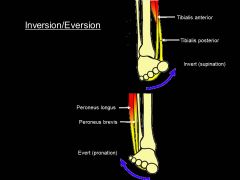
At subtalar joint!
|

|
|
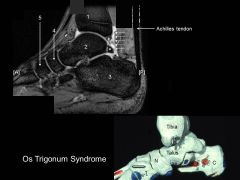
What can cause this painful pinch behind ankle joint in ballet dancers?
|
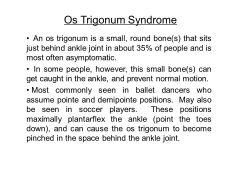
|
|
|
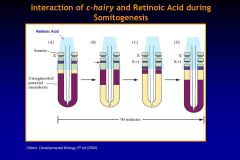
What is the first step in somite formation and uses the mechanism of oscillators?
|
PERIODOCITY
creates a morphogenetic field! |
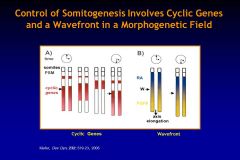
Periodicity - mechanism is governed by oscillators that involve the hairy gene (a
pair-rule gene of drosophila) or related genes. Hairy expression is very dynamic - moves back and forth along the unsegmented paraxial mesoderm every 90 minutes in the mouse. As it recedes caudally a small amount is left where a new somite will bud off. While the targets of the hairy transcription factor are unknown, they may include ephrins and their receptors. |
|
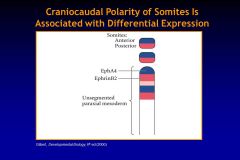
Describe the SEPARATION of somites during their formation process...
|
Separation - ephrin and its receptor are able to cause cell-cell repulsion - EPHRIN B2 and
EPH-A4 are expressed at the boundary between a new somite and unsegmented mesoderm. Injection of mRNA for Ephs alters somite boundary formation. |

|
|

Which transcription factor is associated with regulating EPITHELIALIZATION of somites via expression of cell adhesion proteins FIBRONECTIN and N-CADHERIN?
|
PARAXIS
|

|
|
|
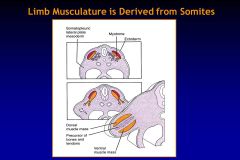
What do the following give rise to:
Sclerotome (SHH) Dermatome (Neurotrophin-3) Epimere (Wnt) Hypomere (BMP4 + Fgf5) |
Sclerotome= chondroctyes of vertebral body
Dermatome= dermal connective tissue of back Epimere= muscles of back Hypomere= muscles of front & sides of throax/abdomen |
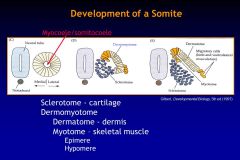
Initially the cells of the somites are pluripotential; however, as development proceeds
different regions of the somites become committed to a particular fate due to factors secreted by the surrounding tissues. At the end of week 4 as the somites become polymorphous, the gap junctions break apart, and the cells migrate throughout the embryo. These regions of the dissolving somite include: 1. Sclerotome - ventral-medial portion of the somite which is induced by the factor sonic hedgehog (Shh) that is secreted by the notochord and the ventral portion of the neural tube. It will give rise to the chondrocytes of the vertebral column. 2. Dermatome - dorsal portion of the somite, which is induced by neurotrophin 3 (NT-3) secreted by the dorsal region of the neural tube, gives rise to the dermal connective tissue of the dorsal skin (other cells are responsible for the dermis in other portions of the body). Antibodies to NT-3 inhibit the formation of the dermis. 3. Epimere - small dorsal-medial part of the myotomes, which is induced by members of the Wnt family secreted by the apical region of the neural tube. It will give rise to the muscles of the back. 4. Hypomere - dorsal-lateral part of the myotomes, which is induced by Bone morphogenic protein-4 (BMP4) and perhaps FGF5 secreted by the lateral mesoderm. There is another factor secreted by the neural tube that inhibits the effects of BMP4 so that it acts only on the most lateral cells of the somite. These cells give rise to the muscles on the lateral and ventral body wall in the thorax and abdomen. B. Sclerotome - represents the ventro-medial section of the somites. It is the first to dissociate from the somite and migrate. The cells migrate medially and ventrally (to surround the notochord) and dorsally (to surround the neural tube). They differentiate into fibroblasts (connective tissue), and chondroblasts (cartilage). Ultimately, they form the vertebral column. C. Dermomyotome - what remains of the somite after the sclerotome migration. This is further divided into the two regions (Fig. 12): 1. Dermatome – the dorsal section – mesenchymal cells that migrate under the surface ectoderm to form the subcutaneous tissue. 2. Myotome – located between the sclerotome and the dermatome. The cells transform into spindle-shaped cells that migrate away. These cells form all of the voluntary skeletal muscle in the trunk of the body from the neck down, as well as the muscles of the limbs. The myotome consists of two divisions: a. Epimere – small section of myotome cells which differentiate into the skeletal muscles along the back (posture, etc.). b. HYPOMERE- larger section of myotome which migrates around rest of the body (front, sides, etc.) gives rise to intercostal muscles, abdominal obliques, and rectus abdominus) |
|
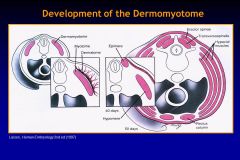
The dermomyotome is what remains of the somite after the sclerotome (future vertebral column) migrates... then the dermomyotome further divides to dermatome & myotome--> epimere and hypomere... what do all those become?
|
Dermatome= dermal connective tissue of back
Epimere= muscles of back Hypomere= muscles of front & sides of throax/abdomen |
Dermomyotome - what remains of the somite after the sclerotome migration. This is further divided into the two regions:
1. Dermatome – the dorsal section – mesenchymal cells that migrate under the surface ectoderm to form the subcutaneous tissue. 2. Myotome – located between the sclerotome and the dermatome. The cells transform into spindle-shaped cells that migrate away. These cells form all of the voluntary skeletal muscle in the trunk of the body from the neck down, as well as the muscles of the limbs. The myotome consists of two divisions: a. EPIMERE – small section of myotome cells which differentiate into the skeletal muscles along the back (posture, etc.). b. HYPOMERE- larger section of myotome which migrates around rest of the body (front, sides, etc.) gives rise to intercostal muscles, abdominal obliques, and rectus abdominus) |
|
|
Which genes (and the transcription factor) can account for different segmentation, like different number of vertebrae in differfent species?
|
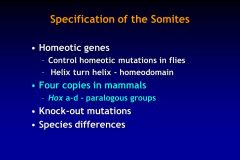
Hox genes! (of HELIX-TURN-HELIX family)
HOMEOTIC TRANFORMATIONs |

|
|
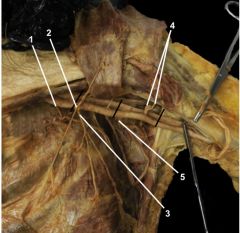
Identify:
Superior thoracic artery Thoracoacromial artery Lateral thoracic artery Posterior & anterior circumflex humeral arteries Subscapular artery |

|
|

