![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
If an aura is present in the preictal period of a seizure, its nature may provide clues to the ictal onset and the diagnosis. What are the auras associated with the frontal lobe? (3) |
1. Eye deviation (forced) 2. Speech impairment (dominant hemisphere) 3. Increased motor activity; simnple motor activity: primary motor strip; complex motor activity: supplementary motor area |
|
|
If an aura is present in the preictal period of a seizure, its nature may provide clues to the ictal onset and the diagnosis. What are the auras associated with the parietal lobe? |
Sensory symptoms |
|
|
If an aura is present in the preictal period of a seizure, its nature may provide clues to the ictal onset and the diagnosis. What are the auras associated with the temporal lobe? (5) |
1. Psychic symptoms: deja vu 2. Rising epiugatric aura 3. Formed visual images (dominant hemisphere) 4. Powerful emotions (fear or fright) 5. Noxious smell |
|
|
If an aura is present in the preictal period of a seizure, its nature may provide clues to the ictal onset and the diagnosis. What are the auras associated with the occipital lobe? |
Basic visual images (flashes or colours) |
|
|
Eight common causes of seizurelike events |
1. Syncope (hypotension or arrhythmia) 2. Transient ischemic attack 3. Paroxysmal vertigo (otolithic crisis of Tumarkin) 4. Epilepsy or seizure 5. Psychiatric disorders ( especially panic) 6. Psychogenic nonepileptic seizure (PNES) 7. Migraine with complex features 8. Paroxysmal sleep disorders (cataplexy) |
|
|
1-year mortality rate of syncope? |
30% |
|
|
What is a convulsive syncope? |
A syncope with brief myoclonic activity that is particularly perplexing confounder |
|
|
Features in the history that may favour seizures and epilepsy as the diagnosis include (4) |
1. Family history of epilepsy 2. History of febrile seizures 3. History of significant perinatal injury 4. History of significant head injury |
|
|
Basic, initial evaluation of suspected seizure in the emergency department? (6) |
1. CBC 2. Complete metabolic panel (electrolytes, creatinine, liver function tests) 3. Other electrolytes: magnesium, calcium 4. Drug screen 5. Antiepileptic drug levels as appropriate 6. Blood glucose |
|
|
The gold standard in making the diagnosis of nonepileptic seizures is |
recording EEG confirmation of an event with routine EEG or ambulatory EEG or with a long-term epilepsy monitoring unit (EMU) |
|
|
Estimated number of patients with epilepsy who also have migraine? |
5% to 10% |
|
|
Features that distinguishes migraine from epilepsy (3) |
1. Last minutes and hours, in contrast to seizures, which typically last only a few minutes 2. Migraine is typically positive, and lasts minutes, in contrasts to seconds in seizures 3. Migraine typically does not have altered awareness associated with attacks |
|
|
Features of seizurelike events tha tfavour a diagnosis of PNES (5) |
1. Psychiatric history (abuse history, psychiatric comorbidity, elevated somatization scales on personality profile testing) 2. Lack of stereotypy 3. Never witnessed or only seen by 1 person 4. Eyes closed at onset 5. Pelvic thrusting |
|
|
Why can a routine EEG be misleading? |
Because a negative EEG does not rule out seizures and a nonspecific finding does not rule in seizures: a wrongly interpreted EEG, with normal variants interpreted as epileptiform activity, is misleading and leads to a diagnostic error |
|
|
How can the diagnostic yield of routine EEG be improved? |
By performing several EEGs up to a total of 4, beyond which the likelihood that any useful information will be discovered is small. Sleep deprivation and obtaining sleep improve the yield in activating epileptiform activity. |
|
|
If an answer is not obtained with routine or ambulatory EEG, what may be the appropriate next step? |
Prolonged video EEG in an EMU may be necessary for proper diagnosis |
|
|
EMU is an acronym for |
Epilepsy Monitoring Unit |
|
|
How many patients get a different diagnosis after admission to an EMU? |
Up to 25% of patients - the diagnosis of nonepileptic seizures has been reclassified as epileptic seizures and vice versa
|
|
|
Indications for structural imaging in patients with seizurelike episodes |
First-time seizures, unless there is a clear idiopathic epilepsy syndrome; sensitivity of MRI is much higher than that of CT, and MRI is the preferred imaging method for evaluating a new seizure disorder; urgency should reflect other clinical characteristics and examination findings, e.g., suspected meningitis, encephalitis, or cerebral ischemia, and whether the semiology or examination suggests a focal seizure rather than a generalized one |
|
|
Which radioactive ligand is used in PET scanning to determine seizure localization? |
18F fluoro-2-deoxy-D-glucose: its uptake reflects metabolic activity; interictally, the PET scan may show a hypometabolic region |
|
|
What is Wada testing? |
Amobarbital is injected into a single carotid distribution through an angiographic cather; it depresses cortical function of the ipsilateral hemisphere, and neuopsychologic testing is then performed to identify the hemisphere with language function; poor at identifying specific locations |
|
|
Role of SPECT in epilepsy (3) |
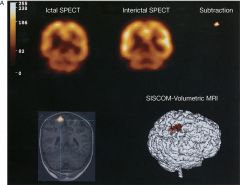
1. Ictal SPECT can measure increase in blood flow at the site of epilepsy focus 2. Subtraction ictal SPECT coregistered MR (SISCOM) takes the ictal image and subtracts it from the interictal image, and the difference is coregistered to MRI to localize the potneital anatomical location of the focus 3. SISCOM is an independent predictor of epilepsy surgery outcome |
|
|
Next step in workup of seizurelike disorders when EEG, MRI, video EEG, semiology, and examination are inconclusive? |
Functional imaging, and is often used in epilepsy surgical evaluation |

