![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
31 Cards in this Set
- Front
- Back
|
Define: Sprain
|
An injury to the ligamentous structures surrounding a joint, usually caused by a wrenching or twisting motion
|
|
|
Define: Strain
|
An excessive stretching of a muscle, its fascial sheath, or a tendon.
|
|
|
Identify: Dislocation, Normal, Subluxation
|
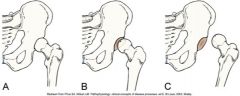
Identify: A, B, and C
|
|
|
What structures are involved with carpal tunnel syndrome and how can one receive relief?
|
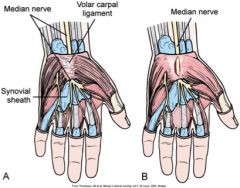
The median nerve and the volar carpal ligament. Relief of carpal tunnel syndrome involves the decompression of the medial nerve by incision through the transverse carpal ligament.
|
|
|
What areas of the hand does one experience pain due to carpal tunnel syndrome?
|
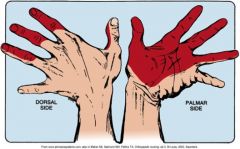
Pain is experienced through the distribution of the median nerve. The shaded areas depict the locations.
|
|
|
What is a meniscus injury?
|
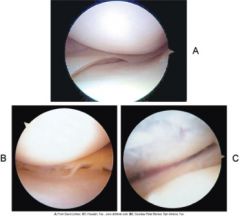
Primarily, injury of fibrocartilage in the knee, but can be found in other joints. Injuries mainly consists of ligament sprains (common with athletes) and torn meniscus.
A. Normal meniscus B. Torn meniscus C. Surgically repaired meniscus |
|
|
What is a anterior cruciate ligament (ACL) injury?
|
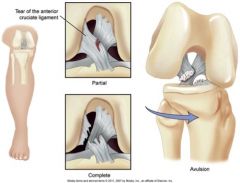
Most common knee injury. Injury can result in partial, complete, and avulsion (tearing away). Often reported as coming down on knee, twisting, and hearing a pop; followed by acute pain and swelling.
|
|
|
Identify the location of the amputations sites and provide a brief description.
|
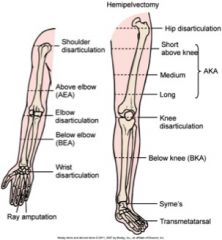
Locations include: upper and lower extremities. Descriptions of amputations are illustrated above.
|
|
|
What is a fracture?
|
Is a disruption or break in the continuity of the structure of the bone.
Majority of fractures from traumatic injuries. Some fractures secondary to disease process (i.e. cancer or osteoporosis) |
|
|
What is the difference between open and closed fractures?
|
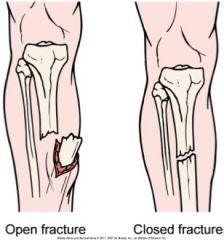
They are both classifications according to communication with the external environment.
Open (or compound) fracture is a brake in skin, exposing the bone and causing soft tissue injury. Close (or simple) fracture is characterized by an intact and non-rupture of the skin. |
|
|
What are the 7 types of fractures?
|
A. Transverse
B. Spiral C. Greenstick D. Comminuted E. Oblique F. Pathological G. Stress |
|
|
What are the 5 types of fractures?
|
A. Bleeding, subsequent hematoma
B. Fibrous network C. Invasion of osteoblasts, lengthening collagen, deposition of calcium D. Callus formation E. Remodeling |
|
|
Identify collaborative care for fractures.
|

Diagnostics: History and physical, X-ray, MRI, CT
Collaborative Therapy: Fracture reduction, Fracture immobilization, Open fractures |
|
|
What are the clinical manifestations of a fracture?
|
Mechanism of injury associated with numerous signs and symptoms:
Immediate localize pain Decrease function inability to bear weight on or use affected part Patient guards and protects extremity |
|
|
What observations and steps for fractures are important?
|
Fractures may not be accompanied by obvious bone deformity.
Immobilize extremity if fracture is suspected. Unnecessary movement can increase soft tissue damage and may convert closed fracture to open. |
|
|
What factors influence healing?
|
Age
Initial displacement Site of fracture Implants Infection Blood supply to area Hormones |
|
|
What are the overall goals of fracture treatment?
|
Anatomic realignment of bone fragments
Immobilization to maintain realignment Restoration of normal or near-normal function of injured parts. |
|
|
What is closed reduction?
|
Nonsurgical, manual realignment of bone fragments to previous anatomic position.
Traction and countertraction manually applied to bone fragments to restore position, length, and alignment |
|
|
What is open reduction?
|
Correction of bone alignment through surgical incision
Includes internal fixation with use of wires, screws, pins, plates, intramedullary rods, or nails NOTE: closed reduction is preferred over open reduction |
|
|
What drug therapy medications are common for fractures?
|
Central and peripheral muscle relaxants.
May include carisoprodol (Soma), cyclobenzaprine (Flexeril), and methocarbamol (Robaxin). |
|
|
What are some side effects of muscle relaxants?
|
Drowsiness
Lassitude (physical and mental weakness) Headache Weakness and fatigue Blurred vision Ataxia Gastrointestinal upset |
|
|
What are the dietary requirements for fractures?
|
Ample protein (1g/ kg of body weight)
Vitamins (B, C, D) Calcium Phosphorus Magnesium 2L-3L daily fluid intake High-fiber with fruits and vegetables |
|
|
N.A. What findings should cause concern for fractures?
|
Deformity or unnatural position of affected limb
Edema and ecchymoses Muscle spasm Tenderness and pain Loss of function Numbness, tingling, loss of distal pulses Grating (crepitus) Open wound over injured site, exposure of bone |
|
|
N.A. What are the vital initial treatments for fractures?
|
Life-threatening injuries first
Ensure airway, breathing, and circulation Control external bleeding with direct pressure or sterile pressure dressing and elevation of extremity |
|
|
N.A. What are other important initial treatments for fractures?
|
Check neurovascular status distal to injury before and after splinting
Splint joints above and below fracture sites Splint fracture sites Do not straighten fractured or dislocated joint Do not manipulate protruding bone ends IF possible, elevate injured limb Apply ice packs to affected area Obtain x-rays of affected area Administer tetanus diphtheria prophylaxis |
|
|
N.A. What are the ongoing monitoring criteria for fractures?
|
Vital signs, level of consciousness, oxygen saturation, neurovascular status, and pain
Compartment syndrome (characterized by excessive pain, pallor, parasthesia, paralysis, and pulselessness) Monitor for fat embolism Mark location of pulses to facilitate; repeat assessment |
|
|
N.A. What past health history (subjective) are relevant to fractures?
|
Traumatic injury
Long-term repetitive forces (stress fracture) Bone or systemic disease Prolonged immobility Osteopenia Osteoporosis |
|
|
N.A. What medications or health management therapies (subjective) are relevant to fractures?
|
Use of corticosteroid (osteoporotic fracture)
Analgesics Estrogen replacement therapies Calcium supplements |
|
|
N.A. What surgeries and other treatments are relevant to fractures?
|
First aid treatment of fracture
Previous musculoskeletal surgeries |
|
|
N.A. What activities-exercises or cognitive perceptions (subjective) are relevant to fractures?
|
Loss of motion or weakness
Muscle spasms Sudden and severe pain in affected areas Numbness, tingling, loss of sensation Chronic pain that increases with activity |
|
|
N.A. What observations (objective) are relevant to fractures?
|
Apprehension, guarding injury
Skin lacerations Pallor and cool skin or bluish and warm distal to injury Ecchymosis Hematoma Edema at site of fracture Decrease or absent pulse distal to injury Decrease or absent sensation Delayed capillary refill Paresthesias Hypersensation Restricted or lost function of affected part Local bony deformities Abnormal angulation Shortening, rotation, or crepitation of affected part Muscle weakness |

