![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
42 Cards in this Set
- Front
- Back
|
Describe the stages of the human life cycle, with regard to diploid and haploid cells
|
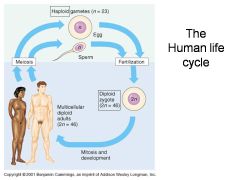
Both eggs and sperm are generated through meiosis, resulting in haploid (1n, 23 chromosomes) cells for each gamete (egg or sperm)
Once the egg is fertilized, it becomes a diploid zygote (2n, 46 chromosomes), undergoes mitosis and development, becoming a multicellular diploid adult (2n, 46 chromosomes) |
|
|
Contrast and compare the processes of mitosis vs. meiosis
|
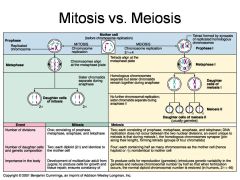
Mitosis:
1 division, with 4 phases (prophase, metaphase, anaphase, and telophase) 2 daughter cells, diploid and identical to mother cell Utilized throughout all stages of organism development and repair Meiosis: 2 divisions with 4 phases (prophase, metaphase, anaphase, and telophase), tetrads are developed from joining chromatids 4 daughter cells, all haploid (1n), not identical to mother cell Utilized in reproduction to ensure genetic variability |
|
|
Describe the stages of spermatogenesis
|
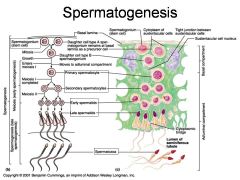
1. Spermatogonium (stem cell) undergoes mitosis at the basal lamina
2. One daughter cell (type A) remains at basal lamina, while second daughter cell (type B) becomes migrates towards lumen and enters the adluminal compartment of the seminiferous tubule. 3. Type B daughter cell (2n, known at primary spermatocyte) undergoes meisosis I, resulting in 2 1n secondary spermatocytes 4. 2 Secondary spermatocytes undergo meiosis II, resulting in a total of 4 spermatids (1n, haploid) 5. Spermatids mature into spermatozoa. |
|
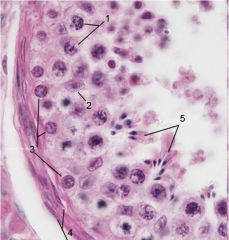
What is this? What are the numbered bits?
|
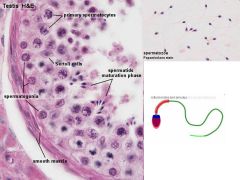
Testis. 1.Primary spermatocytes 2. Sertoli cells 3. Spermatogonia 4. Smooth muscle 5. Spermatids in maturation phase
|
|

What are these?
|
Spermatozoa
|
|
|
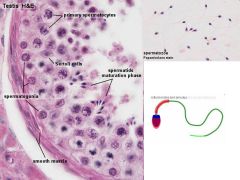
How is sperm production regulated by hormones?
|
1. The hypothalamus releases GnRH, which stimulates the anterior pituitary gland
2. The anterior pituitary gland releases FSH (which stimulates Sertoli cells) and LH (which stimulates interstitial cells) 3. Sertoli cells initiate spermatogenesis and produce Inhibin (which travels back to the hypothalamus, negative feedback) 4. Interstitial cells produce Testosterone (which travels back to the hypothalamus, negative feedback, and other body tissues, stimulating other production) 5. Testosterone and Inhibin inhibit the hypothalamus, lowering GnRH production (Negative feedback loop). |
|
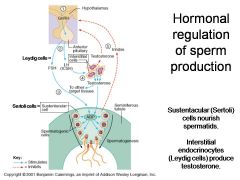
What is this?
|
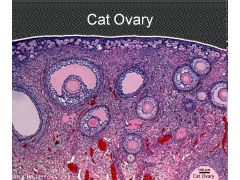
A cat ovary
|
|
|
Describe the hormonal control of the female reproductive system, relative to development
|
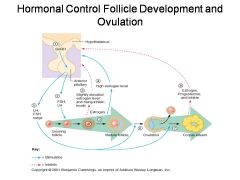
1. The hypothalamus produces GnRH, which stimulates the Anterior Pituitary gland
2. The Anterior Pituitary gland produces LH and FSH, which stimulates the growing folicle 3. Follicle stimulates rising inhibin level and slightly elevated estrogen 4. High estrogen level and elevated inhibin inhibit GnRh production, which stops development of all but one follicle 5. LH and FSH production surges as inhibiting effect from other follicles disappears, and estrogen level elevates 6. Ovulation occurs as egg leaves mature follicle 7. Mature follicle becomes the corpus luteum 8. Corpus luteum stimulates production of estrogen, progesterone, and inhibin, which act as negative feedback and inhibit GnRH production in the hypothalamus |
|
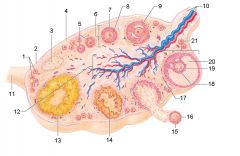
Identify 1
|
Primordial follicles
|
|
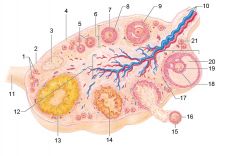
Identify 2
|
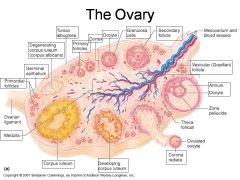
Germinal epithelium
|
|
Identify 3
|
Degenerating corpus luteum (corpus albicans)
|
|
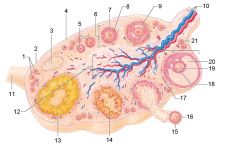
Identify 4
|
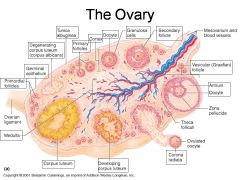
Tunica albuginea
|
|
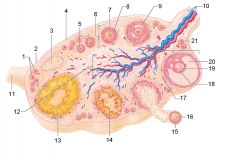
Identify 5
|
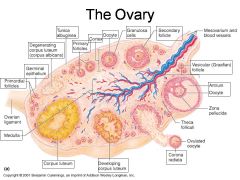
Primary follicles
|
|
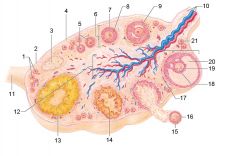
Identify 6
|
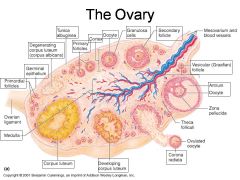
Cortex
|
|
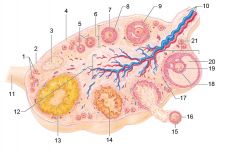
Identify 7
|
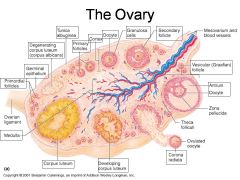
Oocyte
|
|
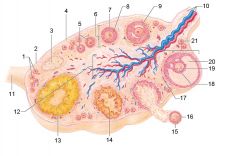
Identify 8
|
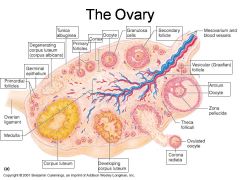
Granulosa cells
|
|
Identify 9
|
Secondary follicle
|
|
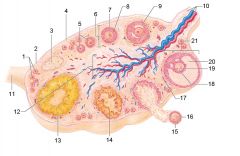
Identify 10
|
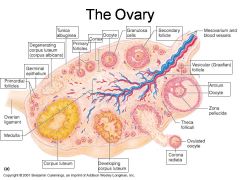
Mesovarium and blood vessels
|
|
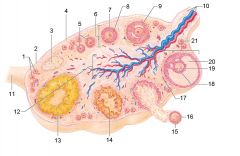
Identify 11
|
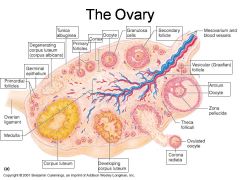
Ovarian ligament
|
|
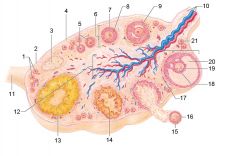
Identify 12
|
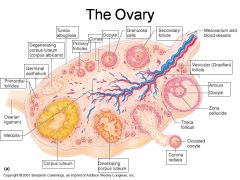
Medulla
|
|
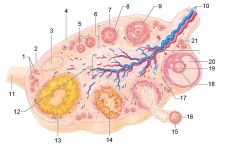
Identify 13
|
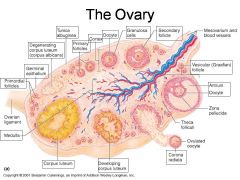
Corpus luteum
|
|
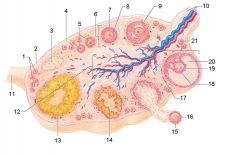
Identify 14
|
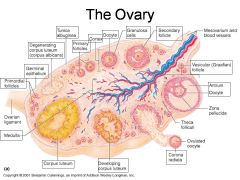
Developing corpus luteum
|
|
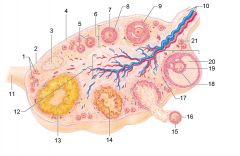
Identify 15
|
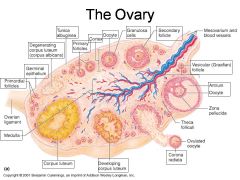
Corona radiata
|
|
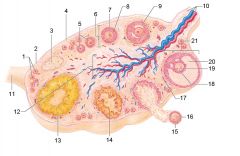
Identify 16
|
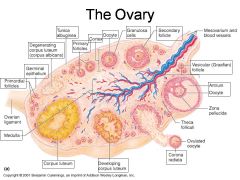
Ovulated oocyte
|
|
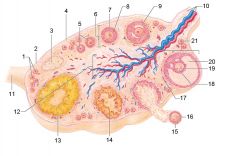
Identify 17
|
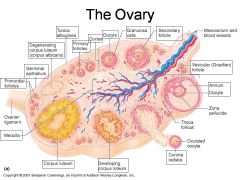
Theca folliculi
|
|
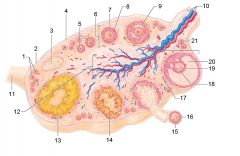
Identify 18
|
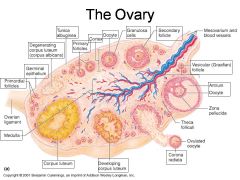
Zona pellucida
|
|
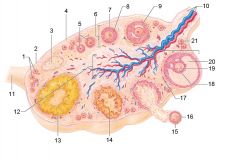
Identify 19
|
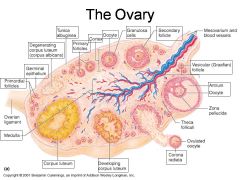
Oocyte
|
|
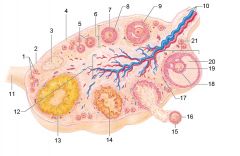
Identify 20
|
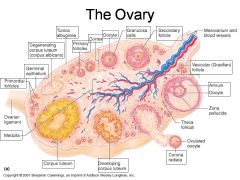
Antrum
|
|
Identify 21
|
Vesicular (Graafian) follicle
|
|

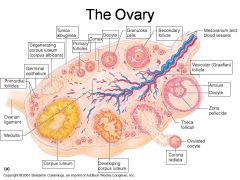
Identify A
|
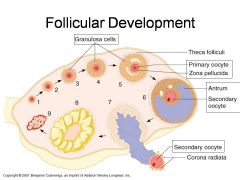
Granulosa Cells
|
|

Identify B
|
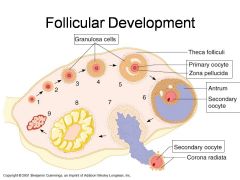
Theca folliculi
|
|

Identify C
|
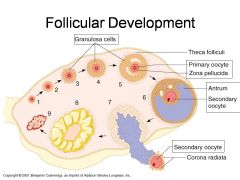
Primary oocyte
|
|

Identify D
|
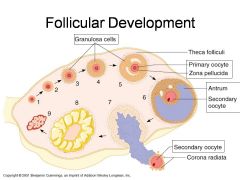
Zona pellucida
|
|

Identify E
|
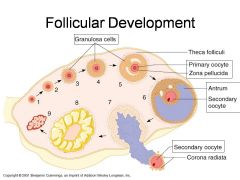
Antrum
|
|

Identify F
|
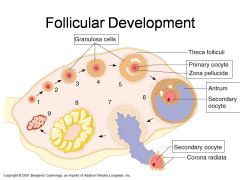
Secondary oocyte
|
|

Identify G
|
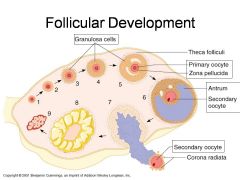
Secondary oocyte
|
|

Identify H
|
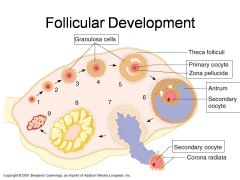
Corona radiata
|
|
|
Describe the relative levels of the hormone LH as related to the periods of the female cycle
|
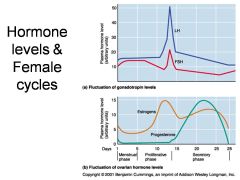
LH rises very slightly from the beginning of the menstrual phase through the middle of the proliferative phase, then begins rising sharply, peaking just before ovulation, then falling sharply over the next day or so, the falls slowly to it's lowest point immediately before menstruation.
|
|
|
Describe the relative levels of the hormone FSH as related to the periods of the female cycle
|
FSH rises slowly to a low peak between the menstrual phase and a few days after the beginning of the proliferative phase. It then falls slowly over the next few days before rising sharply to it's highest peak one day before ovulation (at the same time as LH peaks). It then falls sharply over the next day, then falls slowly to its lowest point a few days before the end of the secretory phase.
|
|
|
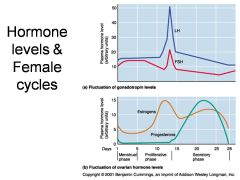
Describe the relative levels of the hormone Estrogen as related to the periods of the female cycle
|

Estrogen falls to its lowest point a few days into the menstrual phase, then rises in an increasing curve to it's highest point a few days before ovulation (before the peak of LH and FSH), then falls to a midpoint valley just after the secretory phase starts. It then rises gradually until a few days before the end of the secretory phase, then falls as menstruation begins.
|
|
|
Describe the relative levels of the hormone Progesterone as related to the periods of the female cycle
|
Progesterone production is minimal as menstruation begins, and falls to almost nothing one day later. It begins rising in an accelerating curve as ovulation begins, peaking midway through the secretory phase and falling in a decreasing arc until menstruation.
|
|
|
Describe the uterine cycle as related to the menstrual cyle
|
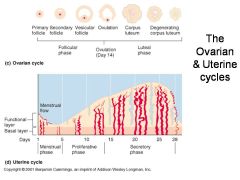
As menstruation begins, the functional layer sloughs off and vascularization of the remaining tissue is minimal, falling to it's lowest point just before the proliferative phase. Build up of the functional layer and increasing vascularization occur throughout the proliferative and secretory phases.
|

