![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
262 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
albumin
|
oncotic pressure, bind = hydrophobic = 1 hormones 2 AAs 3 steroids 4 vitamins 5 FAs 6 hemin (heme+chloride)
|
|
|
|
alpha1-antiprotease/antitrypsin
|
trypsin and general protease inhibitor (protect tissue from enzymes of inflammatory cells, esp elastase), acute-phase protein
|
|
|
|
alpha2-macroglobulin
|
inhib serum endoproteases -> protease-α2M is recognized by macrophage receptors
|
|
|
|
angiotensinogen
|
alpha2, precursor to the pressor peptide angiotensin I
|
|
|
|
antithrombin-III
|
alpha2, protease inhibitor of intrinsic pathway
|
|
|
|
apolipoprotein B
|
assembly of lipoprotein particles
|
|
|
|
blood serum
|
plasma minus I, II, V, VIII plus serotonin (thrombocyte lysis)
|
|
|
|
C-reactive protein
|
beta-globulin, acute-phase protein (inflammation) - bind phosphocholine on surface of dead\dying cells to activate complement
|
|
|
|
ceruloplasmin\Ferroxidase
|
alpha-globulin, transport copper, oxidize Fe2+ (to facilitate transport)
|
|
|
|
chylomicron
|
dietary (exogenous) fat (mainly TAG) from intestine to striated muscle & adipose tissue
|
|
|
|
clotting via intravascular and extravascular pathways, time
|
IV pathway about 3 min, EV pathway about 10 s
|
|
|
|
contact activation pathway
|
intrinsic pathway
|
|
|
|
events in hemostasis
|
1 - vascular constriction 2 - formation of a platelet plug 3 - formation of a blood clot through blood coagulation 4 growth of fibrous tissue into it
|
|
|
|
factor IV
|
Ca2+
|
|
|
|
factor IX
|
1 plasma thromboplastin component (PTC) 2 Christmas factor 3 Antihemophilic factor B
|
|
|
|
factor v
|
1 proaccelerin 2 labile factor 3 accelerator factor 4 Ac-globulin (Ac-G)
|
|
|
|
factor VII
|
1 serum prothrombin conversion acceleration (SPCA) 2 proconvertin 3 stable factor
|
|
|
|
factor VIII
|
1 antihemophilic factor (AHF) 2 antihemophilic globulin (AHG) 3 antihemophilic factor A
|
|
|
|
factor X
|
1 Stuart factor 2 stuart-prower factor
|
|
|
|
factor XI
|
1 plasma thromboplastin antecedent (PTA) 2 antihemophilic factor C
|
|
|
|
Factor XII
|
Hageman factor
|
|
|
|
Factor XIII
|
Fibrin-stabilizing factor, transglutaminase
|
|
|
|
FI
|
Fibrinogen
|
|
|
|
FII
|
Prothrombin
|
|
|
|
FIII
|
tissue factor\tissue thromboplastin
|
|
|
|
haptoglobin
|
alpha2-globulin, bind free Hb (= spare iron, protect tubules), acute phase protein
|
|
|
|
HDL
|
transport cholesterol from tissue to liver for excretion (good cholesterol)
|
|
|
|
hemopexin
|
beta-globulin, bind to porphyrins (esp heme)
|
|
|
|
High-molecular-weight kininogen (HMWK)
|
Fitzgerald factor
|
|
|
|
IGF-I (insulinlike growth factor)
|
mediate anabolic effect of GH
|
|
|
|
LDL
|
cholesterol from liver to tissue (bad cholesterol)
|
|
|
|
lipoproteins
|
1 chylomicrons 2 IDL 3 VLDL 4 LDL 5 HDL
|
|
|
|
orosomucoid
|
alpha1-globulin, uncertain, rise in inflammation
|
|
|
|
platelet-activating factor\platelet-aggregating factor (PAF), source
|
1 neutrophils 2 basophils 3 platelets 4 endothelial
|
|
|
|
platelet-aggregating factor\platelet-activating factor, function
|
phospholipid mediator of platelet aggregation, inflammation and anaphylaxis
|
|
|
|
Prekallikrein
|
Fletcher factor
|
|
|
|
Protein C
|
alpha2, anticoagulant
|
|
|
|
sex-hormone binding globulin (SHBG)
|
betagloublin, androgens and estrogens
|
|
|
|
stromatin
|
intermediate filament of RBCs
|
|
|
|
thyroxine-binding globulin
|
alpha, bind thyroid hormone in blood stream
|
|
|
|
time for production of a new RBC
|
7d
|
|
|
|
tissue factor pathway
|
extirinsic pathway, extravascular pathway
|
|
|
|
tissue factor pathway inhibitor (TFPI)\lipoprotein-associated coagulation inhibitor (LACI)/anticonvertin
|
protein that inhibit extravascular pathway by binding to IIIa-VIIa-Ca2+-Xa complex
|
|
|
|
transthyretin\thyroxine-binding prealbumin
|
carrier protein for thyroid hormones in blood stream
|
|
|
|
VLDL
|
carry newly synthesized (endogenous) lipids (mainly TAG) from liver to extrahepatic tissue
|
|
|
|
what determines the density of lipoproteins
|
increased density = decreased lipid, increased protein
|
|
|
|
basophil function
|
1 allergic\anaphylactic 2 high binding to IgE(reagin) 3 secrete 1 histamine 2 heparin 3 serotonin 4 bradykinin
|
|
|
|
bradykinin
|
potent vasodilator, one of the physiological mediators of anaphylaxis
|
|
|
|
cause of megaloblastic\macrocytic\pernicious anemia
|
vit b12, folic acid
|
|
|
|
eosinophils, function
|
1 mucous immunity 2 parasitic infection (1 release hydrolytic enzymes from lysosomes 2 release reactive oxides esp lethal to parasites 3 release a larvacidal polypeptide (major basic protein)) 3 allergy (detoxify some of the inflammatory products)
|
|
|
|
hemosiderin
|
aggregated ferritin, less mobilizable
|
|
|
|
histamine
|
vasodilator, bronchoconstrictor
|
|
|
|
IgA
|
1 dimer 2 mucosal, secretory 3 antiviral
|
|
|
|
IgD
|
1 monomer 2 uncertain function 3 receptor on B cell
|
|
|
|
IgE\reagin
|
1 monomer 2 bind to mast\basophils 3 allergy 4 histamine&serotonin 5 parasitic worms
|
|
|
|
IgG
|
1 most abundant 2 secondary humoral response of immunity 3 monomer 4 activate complement system 5 opsonization 6 cross the placental barrier
|
|
|
|
IgM
|
1 pentamer 2 B-cell surface 3 first antibody in primary immune response 4 activate complement system (as IgG)
|
|
|
|
lifespan of granulocytes
|
4-8h in blood, 4-5d in tissue, faster if serious infection
|
|
|
|
lifespan of lymphocytes
|
weeks to months
|
|
|
|
lifespan of monocytes
|
10-20h in blood, months in tissue
|
|
|
|
lifespan of platelets
|
8-12d
|
|
|
|
monocyte function
|
1 phagocytosis 2 1st line of defence 3 APC 4 can phagocytose up to 100 bacteria and large particles (parasites, cells)
|
|
|
|
monocytes, number
|
300-600\μL
|
|
|
|
neutrophils, function
|
1 phagocytosis 2 2nd line of defence 3 can phagocytose 3-20 bacteria
|
|
|
|
number of leukocytes, mnemonics
|
NLM EB
|
|
|
|
serotonin
|
vasoconstrictor, bronchoconstrictor
|
|
|
|
sideropenic anemia
|
iron deficiency
|
|
|
|
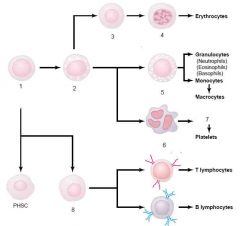
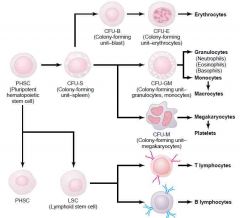
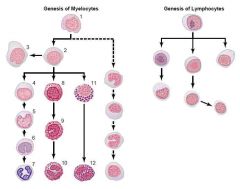
Erythrogenesis, cell line
|
multipotential hematopoietic stem cell (hemocytobloast) -> common myeloid progenitor -> proerythroblast (pronormoblast) -> basophilic erythroblast -> polychromatic erythroblast -> orthochromatic erythroblast (normoblast) -> polychromatic erythrocyte (reticulocyte) -> erythrocyte
|
|
|
|
orthochromatic
|
tissue\cell that stain with the same colour as the dye
|
|
|
|
hemolysin
|
an agent or substance (antibody, bacteria), that causes hemolysis
|
|
|
|
Tenase
|
complex activating FX, intrinsic and extrinsic way
|
|
|
|
extrinsic tenase
|
III, VII, Ca2+
|
|
|
|
intrinsic tenase
|
IXa (cofactor VIIIa), negatively charged surface (platelet membrane)
|
|
|
|
prothrombinase, function
|
activate thrombin from prothrombin
|
|
|
|
prothrombinase complex, components
|
Xa (serine protease), Va (protein cofactor), on negatively charged phospholipid membrane in the presence of Ca2+
|
|
|
|
statistical significance (p)
|
mean that the difference is not random, but that the stimulus induced this change with the p probability
|
|
|
|
altricial
|
altrix = nourisher. helpless at birth and require parental care for a period of time
|
|
|
|
precocial
|
active and able to move freely from birth, require little parental care
|
|
|
|
lissencephalic
|
smooth cerebrum without convolutions
|
|
|
|
poikilotherm
|
poikilos = varied. an organism having a BT that varies with the environment
|
|
|
|
cannula
|
a tube that can be inserted into a cavity, usually by means of a trocar filling its lumen
|
|
|
|
trocar
|
= 3-side. used to insert a cannula, removed after placement of cannula
|
|
|
|
DuBois-Reymond rule
|
there must be sufficient velocity in intensity change to elicit an impulse
|
|
|
|
stealing of a stimulus
|
accommodation of the membrane to the stimulus
|
|
|
|
incomplete tetanus
|
tetanus in which each stimulus cause a contraction to be initiated when the muscle has only partially relaxed from the previous one, superposition
|
|
|
|
complete tetanus
|
tetanus in which stimuli to a particular muscle is repeated so rapidly that decrease of tension between stimuli cannot be detected, summation
|
|
|
|
oligocythemia\erythrocytopenia
|
low RBCs
|
|
|
|
polycythemia, polyglobulia
|
increased RBCs
|
|
|
|
leukocytosis
|
increased WBCs
|
|
|
|
leukocytopenia
|
decreased WBCs
|
|
|
|
hematocrit
|
centrifugation of non-coagulated blood
|
|
|
|
determine hemoglobin content
|
spectrophotometry of Drabkin's solution, create hemoglobin cyanide
|
|
|
|
increased blood sedimentation rate can indicate
|
inflammation, tumor, change of blood pH
|
|
|
|
blood sedimentation men
|
men 3-9 mm\h
|
|
|
|
blood sedimentation women
|
7-12 mm\h
|
|
|
|
APCs
|
non-professional (almost all via MHC1), professional (MHC2) = dendritic cell, macrophage, B-cells
|
|
|
|
bradykinin, effect, from which cell
|
vasodilation, mast cell+basophil after allergen contact
|
|
|
|
C1
|
initiate classical pathway
|
|
|
|
C3b
|
opsonization of bacteria
|
|
|
|
C4a, C3a
|
activate mast+basophil
|
|
|
|
C5a
|
chemotaxis of WBCs, activate mast+basophil
|
|
|
|
C5b6789 complex\membrane attack complex (MAC)
|
lysis (perforin)
|
|
|
|
complement system is triggered by
|
antibody-antigen, mannose-binding lectin pathway, alternative way (directly to pathogen)
|
|
|
|
complement system, function
|
lysis (perforin), opsonization, modulate immune and inflammatory response, immune clearance (deposit immune complex in spleen\liver)
|
|
|
|
cytokines
|
hormone-like molecules that generally act in paracrine fashion to regulate immune response
|
|
|
|
cytotoxic T cells
|
CD8 surface protein, bind antigen from MHCI, mechanism = perforin, secretions
|
|
|
|
dendritic cell, function
|
APC, secrete cytokines
|
|
|
|
dendritic cell, location
|
skin, mucosa, lymphoid tissue
|
|
|
|
Dendritic cell, origin
|
hemopoietic stem cell
|
|
|
|
GM-CSF, source
|
T cell, macrophages, NK, B cell
|
|
|
|
helper T cell
|
most numerous, major immune regulator via lymphokines, express CD4 surface protein, TH1 stimulate B lymphocyte, TH2 stimulate T lymphocyte
|
|
|
|
IL-1
|
by macrophages, activate T cell+macrophage, promote inflammation
|
|
|
|
IL-11, cellular source
|
bone marrow stromal cells
|
|
|
|
IL-11, effect
|
stimulate acute-phase protein production
|
|
|
|
IL-12, cellular source
|
Macrophages, B cells
|
|
|
|
IL-12, effect
|
stimulate interferon-gamma production, induce TH1 differentiation
|
|
|
|
IL-2
|
by TH1, activate lymphocytes+NK+macrophage
|
|
|
|
IL-4, cell origin
|
TH2, basophil, mast cell, eosinophil
|
|
|
|
IL-4, effect
|
activate lymphocytes, monocytes, IgE class switching
|
|
|
|
IL-5
|
by TH2+mast cell+eosinophil, stimulate eosinophil differentiation, late-phase allergy response
|
|
|
|
IL-6, ceullar source
|
TH2, macrophages
|
|
|
|
IL-6, effect
|
activate lymphocytes, differentiate B cell, stimulate production of acute-phase proteins
|
|
|
|
IL-8, cellular sources
|
T cell, macrophages
|
|
|
|
IL-8, effect
|
chemotaxis of neutrophils, basophils, T cell
|
|
|
|
interferon-alpha + beta
|
from virally infected cells, induce resistance in other cells
|
|
|
|
interferon-gamma, effect
|
activate macrophage, inhibit TH2
|
|
|
|
interferon-gamma, source
|
TH1, NK
|
|
|
|
K+ ICF
|
140 mM
|
|
|
|
Langerhans cell
|
specialized dendritic cell in the skin
|
|
|
|
lymphokines
|
interleukins, GM-CSF, interferon-gamma
|
|
|
|
Lymphotoxin\TNF beta, effect
|
promote inflammation, lyse\damage many cell types
|
|
|
|
Lymphotoxin\TNF beta, source
|
TH1, B cells
|
|
|
|
MHCI present antigen to
|
cytoxic T cell
|
|
|
|
MHCII present antigen to
|
helper T cell
|
|
|
|
Na+, ICF
|
14 mM
|
|
|
|
serotonin
|
(sero = serum, tonin = tonus), neurotransmitter, vasconstrictor, released by thrombocytes
|
|
|
|
suppressor T cell
|
immune tolerance, inhibit immune response
|
|
|
|
TGF (transforming growth factor) beta, effect
|
immunosuppression (inhibit other cytokines)
|
|
|
|
TGF beta, source
|
T cells, macrophages, B cells, mast cell
|
|
|
|
TNF alpha, effect
|
promote inflammation
|
|
|
|
TNF alpha, source
|
macrophages, NK, T cells, B cells, mast cell
|
|
|
|
von Willebrand factor
|
secreted mainly by healthy endothelium, mediate platelet adhesion to collagen, complex with VIII to keep it from degrading
|
|
|
|
4 components of surgical anesthesia
|
analgesia, hypnosis, myorelaxation, neurolepsis
|
|
|
|
altricial animals
|
rat, mouse, cat, dog
|
|
|
|
amount of calcium in body
|
1100g
|
|
|
|
amount of phosphorus in body
|
500-800 g
|
|
|
|
anesthesia
|
= loss of sensation
|
|
|
|
barbiturates (pentarbital, phenobarbital)
|
CNS depressant, tranquilizer, hypnotic, anti-seizure
|
|
|
|
descriptive statistics
|
gaussian distribution (SD, average), mean, median, mode (most frequent parameter)
|
|
|
|
dihydropyridine receptor\L(long-lasting)-type calcium channel
|
voltage-dependent calcium channel in skeletal muscle cell
|
|
|
|
gyrencephalic animals
|
monkey, dog, cat
|
|
|
|
halothane\fluothane and methoxyflurane\isoflurane, properties
|
good myorelaxant, mild cardiovascular and respiratory depression, rapid onset and reversal
|
|
|
|
hypercalcemia
|
cardiac arrest, CNS depression
|
|
|
|
hypocalcemia
|
increased excitation, tetany
|
|
|
|
ketamines (Ketalar, Imalgane, Nalorphin)
|
catatonia (rigidity), strong analgesia, increased sympathetic activity, bad myorelaxant
|
|
|
|
maximal contraction force of muscle
|
300 kg\m2
|
|
|
|
maximal power of muscle, at which speed
|
750 kW\m2, at 2.5 m\s
|
|
|
|
Power
|
= W\t = F x V
|
|
|
|
precocial animal
|
guinea pig
|
|
|
|
procaine derivatives
|
local anesthetic
|
|
|
|
Ryanodine receptor (RyRs)
|
class if intracellular calcium channels (release Ca2+ from sarcoplasmic reticulum)
|
|
|
|
xylazine
|
neuroleptic agent
|
|
|
|
Ig's - classes
|
GAMED. IgG, IgA, IgM, IgE, IgD
|
|
|
|
IgG and IgM - which is the first response?
|
IgM: IMmediately produced. IgG: Greater response
|
|
|
|
Increased risks of certain cancers when on immunosuppressant therapy (ie after heart or kidney transplant)
|
Up to 5 five times higher
(Thus the immune system eliminates many of the potential cancer cells. Mutation -> Abnormal gene -> abnormal protein -> humor\cell-mediated immunity) (Guyton) |
|
|
|
The carcinogens that currently cause the greatest number of deaths are those found in?
|
Cigarette smoke
(They cause about 1\4 of all cancer deaths) (Guyton) |
|
|
|
How can physical irritants lead to cancer?
|
Ie continued abrasion of the lining of the intestinal tract by some types of food -> damage to tissue -> rapid mitotic replacement of the cells
The more rapid the mitosis, the greater the chance for mutation. (Guyton) |
|
|
|
Size of normal red blood cell
a. Diameter b. Thickness - thickest point, center c. Volume |
a. 7.8 um
b. 2.5 um c. 1 um d. 90-95 um^3 (Guyton) |
|
|
|
What happens to the volume of RBCs when hemoglobin formation is deficient?
|
The volume of the red cell can decrease due to diminished hemoglobin to fill the cell.
(Guyton) |
|
|
|
Carrying capacity of oxygen in hemoglobin per 100 mL of blood
a. In men b. In women |
a. 20 mL O2\100 mL blood
b. 19 mL O2\100 mL blood (each gram of pure Hb can combine with 1.34 mL of oxygen, men have 15g Hb\100mL of cells while women have 14g Hb\100mL of cells) (Guyton) |
|
|
|
Area of production of red blood cells in adults
|
Mostly membranous bones such as vertebrae, sternum, ribs, ilia
Proximal parts of humeri and tibiae (the rest of the bone marrow of the long bones become quite fatty and stop producing RBCs after about 20 years) (Guyton) |
|
|
|
Growth inducers
a. What? b.Which growth inducer promotes growth and reproduction of virtually all the different types of committed stem cells? |
a. Proteins which control growth and reproduction of the different stem cells
b. Interleukin 3 (Guyton) |
|
|
|
Differentiation inducers
a. What |
a. Cause one type of committed stem cell to differentiate one or more steps toward a final adult blood cell
(Guyton) |
|
|
|
(Guyton)
|
|
|

a. 1-6
b. Where does 1 arise from? |

b. Colony-forming-unit erythrocyte (CFU-E)
(Basophil erythroblast because it stains with basic dyes. Have little Hb at this stage In the next generations, the cells become filled with Hb (to 34%), the nucleus condenses to a small size which is finally absorbed or extruded from the cell. At the same the the ER is reabsorbed. Now its a retiuclocyte. It still contains basophilic material: remnants of GA, mitochondria, and a few other cytoplasmic organelles Reticulocyte: diapedesis from bone marrow to capillary The remaining basophilic substance disappear within 1-2 days and the cell is then a mature RBC) (Guyton) |
|
|
|
B12 and folate deficiency
a. Hinders what part of the RBC formation b. Characteristics of the cells |
a. Formation of thymidine triphosphate -> abnormal\diminished DNA
(Maturation failure in the process of erythropoiesis) b. 1. Macrocytes 2. Irregular, oval 3. Increased fragility -> only live 1\2-1\3 as long (Guyton) |
|
|
|
Atrophy
|
A wasting of tissue, organs, or the entire body. Various causes (death and reabsorption of cells, diminished cellular proliferation, decreased cellular volume, pressure, ischemia, malnutrition, lessened function, hormonal changes)
(Guyton) |
|
|
|
Intrinsic factor
a. What b. Function |
a. Glycoprotein secreted from parietal cells in the stomach
b. 1. Bind to B12 and keep it from getting digested 2. Complex bind to receptor sites on the brush border of the ileum and gets absorbed by pinocytosis (Guyton) |
|
|
|
Vitamin B12
a. Minimum amount needed daily to maintain normal red cell maturation b. How much is stored in the liver |
a. 1-3 ug
b. 1000 times that -> 1-3 mg (-> takes 3-4 years for defective absorption to cause maturation failure anemia) (Guyton) |
|
|
|
|
|
|
|

|

(Hb synthesis begins in the proerythroblast stage and continues into the reticulocyte stage)
(Succinyl CoA from Krebs cycle) (Hemoglobin has a molecular weight of 64.5 kD) (Guyton) |
|
|
|
Sickle cell anemia
b. Cause b. Effect |
a. Valine is substituted for glutamate at one point in the beta chain
b. Hypoxia -> sickling: crystallization of Hb molecules (can form 15 um elongated crystals) -> crystals "puncture" the cell membrane when the cell tries to pass through small capillaries -> Sickle-cell anemia (Guyton) |
|
|
|
Iron is used in the body in (6)
|
1. Hb
2. Mb 3. Cytochromes 4. Cytochrome oxidase 5. Peroxidase 6. catalase (Guyton) |
|
|
|
Storage of liver
a. 65% in b. 4% in c. 1% in d. 0.1% in e. 15-30% in f. Total iron |
a. Hemoglobin
b. Myoglobin c. Various heme compounds that promote intracellular oxidation d. Transferrin e. Stored for later use, principally as ferritin, in - reticuloendothelial system (spleen, bone marrow) and heptocytes e. 4-5g (Ferritin is a large storage protein, 460 kD) (Hemosiderin is an extremely insoluble storage form of iron, its main role is when the apoferritin storage pool is saturated. Can be seen microscopically as opposed to ferritin) (Guyton) |
|
|
|
Absorption of iron
a. Mechanism b. How much can be absorbed per day |
a.
1. Liver secrete apotransferrin to bile 2. Apotransferrin binds to free iron, myoglobin, or hemoglobin to form transferrin 3. Transferrin binds to receptor of mucosal cells on most of the GI tract and is pinocytosed 4. Transferrin is released beneath these cells as plasma transferrin b. A few mg a day (Almost independent of ingested amount) (Guyton) |
|
|
|
Sickle cell anemia
b. Cause b. Effect |
a. Valine is substituted for glutamate at one point in the beta chain
b. Hypoxia -> sickling: crystallization of Hb molecules (can form 15 um elongated crystals) -> crystals "puncture" the cell membrane when the cell tries to pass through small capillaries -> Sickle-cell anemia (Guyton) |
|
|
|
Iron is used in the body in (6)
|
1. Hb
2. Mb 3. Cytochromes 4. Cytochrome oxidase 5. Peroxidase 6. catalase (Guyton) |
|
|
|
Storage of liver
a. 65% in b. 4% in c. 1% in d. 0.1% in e. 15-30% in f. Total iron |
a. Hemoglobin
b. Myoglobin c. Various heme compounds that promote intracellular oxidation d. Transferrin e. Stored for later use, principally as ferritin, in - reticuloendothelial system (spleen, bone marrow) and heptocytes e. 4-5g (Ferritin is a large storage protein, 460 kD) (Hemosiderin is an extremely insoluble storage form of iron, its main role is when the apoferritin storage pool is saturated. Can be seen microscopically as opposed to ferritin) (Guyton) |
|
|
|
Iron
a. Average iron loss per day in males b. Average iron loss per day in females c. Total amount stored in the body |
a. 0.6mg\day
b. 1.3mg\day c. 4-5g (Guyton) |
|
|
|
Absorption of iron
a. Mechanism b. How much can be absorbed per day |
a.
1. Liver secrete apotransferrin to bile 2. Apotransferrin binds to free iron, myoglobin, or hemoglobin to form transferrin 3. Transferrin binds to receptor of mucosal cells on most of the GI tract and is pinocytosed 4. Transferrin is released beneath these cells as plasma transferrin b. A few mg a day (Almost independent of ingested amount) (Guyton) |
|
|
|
Where is most of the red blood cells destroyed?
|
In the red pulp of the spleen
(The spaces between the trabecula of the red pulp is only 3 um wide) (Guyton) |
|
|
|
Red blood cells
a. Functions of their limited enzymes b. Cause of their destruction |
a.
1. Maintain pliability of cell membrane 2. Ionic transport 3. Keep iron of Hb in the ferrous form 4. Prevent oxidation of its proteins b. Metabolic systems of old cells becomes progressively less active which make the cell more fragile (The average life span of an RBC is 120 days) (Guyton) |
|
|
|
Megaloblastic anemia
a. Cause of megaloblastic cells |
a. the erythroblasts cannot proliferate rapidly enough to form normal numbers of RBCs
(Guyton) |
|
|
|
Hemolytic anemia - disorders causing increased fragility of RBCs - 3 examples?
|
1. Hereditary spherocytosis
(small and spherical cells, too little cell membrane thus has less compressibility) 2. Sickle cell anemia (hemoglobin S, sickle cells) 3. Erythroblastosis fetalis (Rh+ fetus are attached by Ab from Rh- negative mom) |
|
|
|
Cause of increased cardiac output in anemia (3)
|
1. Hypoxia
2. Less viscosity of blood (1.5 that of water, compared to 3 which is normal) 3. Peripheral hypoxia -> peripheral vasodilation -> increased venous return (Guyton) |
|
|
|

(Guyton)
|
|
|
|
Life span of platelets
|
10 days
|
|
|
|
Life span of white blood cells
a. Which cells have a life span of 4-8 hours in in the circulation and 4-5 days in tissues where they are needed b. Which have life span of 10-20 hours in the blood and months in the tissue c. Which have from weeks to months (Guyton) |
a. Granulocytes
b. Monocytes c. Lymphocytes (Guyton) |
|
|
|
White blood cells
a. Enter the tissue spaces by? b. Move through tissue spaces by? c. White blood cells are attracted to inflamed tissue areas by? |
a. Diapedesis
b. Ameboid movement (up to 40 um\min) c. Chemotaxis (Functional up to 100 um, most cells are within 50 um from a capillary) (Guyton) |
|
|
|
Whether phagocytosis will occur or not depend on 3 selective procedures
|
1. Most natural structures in the tissue have smooth surfaces which resist phagocytosis. Rough surface increase likelihood of phagocytosis
2. Most natural substances of the body have protective protein coats that repel phagocytosis, in contrast to dead cells and foreign particles 3. Antibody\Complement mediation (Guyton) |
|
|
|
Neutrophil & macrophages - compounds aiding the destruction of ingested foreign particles (3)
|
1. Special lysosomal proteolytic enzymes - both
2. Lysosomal lipase (only macrophage)(digest the thick lipid membranes possessed by some bacteria such as the tuberculosis bacillus) 3. Bactericidal powerful oxidizing agents: superoxide, hydrogen peroxide, hydroxyl ions, hypochlorite (hypochlorite is made from chloride and hydrogen peroxide by myeloperoxidase)(these substances are made in the membrane of the phagosome or in peroxisomes) (Guyton) |
|
|
|
Reticuloendothelial system
a. Components |
a. Components
1. Monocytes 2. Fixed tissue macrophages 3. Mobile macrophages 4. A few specialized endothelial cells in the bone marrow (Since most originate in the bone-marrow, the term monocyte-macrophage system is almost synonymous) (Guyton) |
|
|
|
Fixed tissue macrophages in
a. connective tissue b. Lymph nodes c. Lungs d. Liver sinusoids |
a. Histiocytes
b. Tissue macrophages c. Alveolar macrophages d. Kupffer cells (Guyton) |
|
|

|
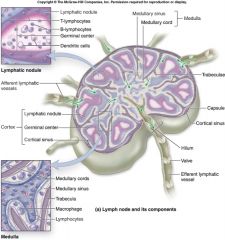
(Lymphoid\lymphatic nodule
one of the spherical masses of lymphoid cells, frequently having a more lightly staining center.) (Germinal center of Flemming: the area in the center of a lymph nodule containing aggregations of actively proliferating lymphocytes) (Dendritic cell: the immune cells involved in the activation of T cells and B cells. They are primarily found in exposed tissue such as skin, the lungs, the stomach and intestines, and the membranes of the nose, but they are also found in blood \ A cell that captures antigens and migrates to lymph nodes and spleen, where it presents the processed antigens to T cells. In the skin there is specialized dendritic cells called Langerhans cells) (Cortical sinus: vascular sinuses in the cortex of a lymph node) (Medullary cords: cords of lymphoid tissue between the sinuses in the medulla of a lymph node) (Medullary sinus: part of the flow system for lymph through lymph nodes; drain into efferent lymphatic vessels at the node hilus) (Trabeculae: supporting bundles of connective tissue traversing the substance of lymph nodes, derived from the capsule) |
|
|

Spleen
|

(Red\Splenic pulp: seen grossly as a reddish-brown substance, because of its abundance of RBCs, consisting of splenic sinuses and the tissue intervening them (splenic cords))
(Sinusoids are capillaries that have enlarged diameter (30-40 um), endothelial cells form an discontinuous layer and have fenestrations without diaphragms, the basal lamina is discontinuous) (Splenic\Billroth cords\Red pulp cords: the tissue occurring between the venous sinuses in the red pulp of the spleen. Consisting of CT cells with a large population of monocytes and macrophages. They contain half the body's monocytes as a reserve. RBCs pass through the cords of Billroth before entering the sinusoids. The passage into the sinusoids may be seen as a bottleneck, where they need to be flexible to pass through) (White pulp of spleen: the part of the spleen that consists of lymphatic nodules and other concentrations of lymphatic tissue, surrounding the arteries of the spleen) (Splenic lymph follicles\Malphigian bodies: small nodular masses of lymphoid tissue attached to the sides of the smaller arterial branches) (Marginal zone: a zone between the red and white pulp of the spleen containing numerous macrophages and a rich plexus of sinusoids supplied white pulp arterioles carrying blood-antigens) (Stedman, The American Heritage® Medical Dictionary) |
|
|
|
How does white blood cells invade a inflamed area? (3)
|
Products from the inflamed tissue (degraded cellular products, viral\bacterial toxins, inflammatory products, complement products..) ->
1. Alter the inside surface of the capillary endothelium, causing the white blood cells to stick to the capillary wall in the inflamed area - this is called margination 2. They cause the intercellular attachments between vascular endothelial of capillaries and small venules to loosen, allowing openings large enough for diapedesis 3. Chemotaxis (Guyton) |
|
|
|
IF AN ITEM COSTING_______ OR MORE IS REPORTED AS LOST, MISSING, STOLEN, OR DAMAGED BEYOND NORMAL WEAR-AND-TEAR, A REPORT OF SURVEY IS REQUIRED.
|
$500
|
1
|
|

Instructions for completion of an SF-368 can be found in what manual?
|

SPPM, COMDTINST M4400.19B
|
1
|
|
|
What is pus?
|
Necrotic tissue excavated in the inflamed tissue by varying portions of dead neutrophils, macrophages, and tissue fluid)
(The dead cells and necrotic tissue gradually autolyze over a period of days) (Guyton) |
|
|
|
Eosinophil - antiparasitic mechanisms
|
Attach themselves to parasites and
1. Release hydrolytic enzymes from their granules which are modified lysosomes 2. Release highly reactive forms of oxygen 3. Release a highly larvacidal polypeptide called major basic protein (Ie against schistosomiasis (1\3 of third world infected), trichinosis <- Trichinella (pork worm), (Believed to detoxify some of the inflammation-inducing substances released by mast cells and basophils during allergic reactions, and probably to phagocytize and destroy allergen-antibody complexes. Attracted by eosinophil-chemotactic factor) (Guyton) |
|
|
|
Leukopenia
a. Causes b. Effects of total leukopenia - after 2 days, after 7 days |
a.
1. Irradiation (gamma, X-ray) 2. Chemicals (anthracene nuclei, benzene) 3. Drugs (chloramphenicol (antibiotic), thiouracil (vs thyrotoxicosis), some barbiturates) b. Due to infection of already present - benign bacteria 1. 2 days -> severe respiratory infection, ulcer of mouth and colon 2. 7 days -> death (Guyton) |
|
|
|
Innate immune system - components
|
1. Phagocytosis by white blood cells and cells of the tissue macrophage system
2. Intestinal conditions - HCl, digestive enzymes 3. Resistance of the skin to invasion by organisms 4. Lysozyme (a mucolytic polysaccharide that attacks bacteria and cause them to dissolute) 5. Basic polypeptides (reach with and inactivate certain types of G+ bacteria) 6. The complement system 7. Natural killer cells (recognize and destroy foreign cells, tumor cells, some infected cells) (Guyton) |
|
|
|
Epitope
|
The simplest form of an antigenic determinant, on a complex antigenic molecule, which can combine with antibody or T cell receptor.
(Stedman) |
|
|
|
Requirements for an antigen (3)
|
1. > 8 kD
2. Regularly recurring molecular groups (epitopes) 3. Generally proteins or large polysaccharides (Guyton) |
|
|
|
Thymus gland preprocessing of the T-lymphocytes
a. What happens b. When does most of the preprocessing take place? |
a. Proliferate and develop extreme diversity for acting against different specific antigens (by combining different gene segments to form the T-cell receptor), the self-reacting T-lymphocytes (up to 90%) gets destroyed an phagocytized.
b. Shortly before birth and a few months after (Guyton) |
|
|
|
Preprocessing of B-lymphocytes
a. During midfetal life b. During late feta life and after birth c. Origin of name |
a. Liver
b. Bone marrow c. Bursa of Fabricius in birds (first discovered site of preprocessing of B-lymphocytes) (Guyton) |
|
|
|
B-lymphocyte
a. Cell differentiation b. Number of divisions of an initial B-lymphocyte, time for each division |
a. B-lymhpocyte -(activated)-> Lymphoblast -> plasmablast -> plasma cells
(Plasma cells are the proliferating cells) b. 9 times, 10 hours each (500 cells in 4 days) (First produce gamma-globulin at a rate of about 200 molecules\s\plasma cell) (Guyton) |
|
|
|
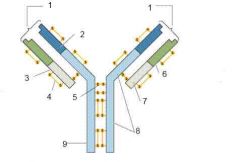
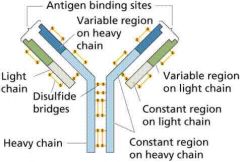
Immunoglobulins - IgG
a. Molecular weight of simple (ie IgG) b. Constituents c. Functional parts |
a. 160 kD
b. Made up of 2 heavy and 2 light chains c. Constant and variable portion (The constant region determines properties such as diffusivity of the antibody in the tissues, adherence of the antibody to specific structures within the tissues, attachment to the complement complex, the ease with which the antibodies pass through membranes...) (Guyton) |
|
|
|
Antibody
a. Antibody-antigen forces b. Formula for affinity constant |
a.
1. Hydrogen bonding 2. Hydrophobic bonding 3. Ionic attractions 4. Van der Waals forces (temporary fluctuating dipoles) b. Ka = [bound antibody-antigen]\([Ab] x [Ag] (Guyton) |
|
|
|
|
|
|

Cascade of reactions during activation of the classic pathway of complement
|

(C3b strongly activate phagocytosis by both neutrophils and macrophages. This process is called opsonization. Often enhance the number of bacteria that can be destroyed by hundredfolds)
(Lytic complex (C5b6789), has a direct effect of rupturing the cell membranes) (In general they cause agglutination and inactivation of viruses) (C5a initiates chemotaxis of neutrophils and macrophages) (Activation of mast cells and basophils by C3a, C34a, and C5a) (In addition to the inflammatory effect by activating basophils and mast cells, several other complement products contribute to local inflammation by vasodilating, increasing permeability and cause fluid proteins to clot the interstitial space) (Guyton) |
|
|
|
Complement system
a. Which cause opsonization for macrophages and neutrophils b. Which cause lysis as the lytic complex c. Which cause chemotaxis of neutrophils and macrophages? d. Which activate mast cells and basophils thus potentiating the inflammation? |
a. C3b
b. C5b6789 c. C5a d. C3a, C4a, C5a (C5a is the only dual-functioning in both causing chemotaxis of phagocytes and activating basophils and mast cells) (Guyton) |
|
|
|
The three major types of antigen-presenting cells
|
1. Dendritic cell (most potent, this is its only known function)
2. Macrophage 3. B-lymphocyte (Guyton) |
|
|
|
Major histocompatibility complex
a. Which type present antigens to Thelper cells b. Which type present antigens to Tc cells |
a. MHC II
b. MHC I (Guyton) |
|
|
|
T-lymphocytes
a. Different types? (3) |
1. Helper T cell
2. Cytotoxic T cell 3. Suppressor T cell (Guyton) |
|
|
|
Helper T cell
a. Function b. IL-2 ->? c. IL4,5,6 ->? |
a. Major regulator of virtually all of the immune system, by secreting lymphokines (interleukins, interferon-gamma, GM-CSF)
b. Most important growth & differentiation inducer of cytotoxic T cells and suppressor T cells. Also stimulates themselves (in association of antigens..) c. The most important growth & differentiation inducer of B-lymphocytes (in association with antigens)(These 3 (IL4-6) have been called B-cell stimulating factors or B-cell growth factors) (usually 3\4 of population, the cell type affected by HIV) (Guyton) |
|
|
|
Immunization by injection of antigens
a. Which type of antigens is used for typhoid fever, whooping cough, diphtheria and many other types of bacterial diseases? b. Which type of antigens is used for toxins of tetanus, botulism and other similar toxic diseases? c. Which type of antigens is used for poliomyelitis, yellow fever, measles, smallpox and other viral diseases? |
a. Dead organisms
b. The toxins have been treated with chemicals so that their toxic nature has been destroyed c. Live, attenuated, organisms (grown in a special culture media, mutated through a series of animals until they have lost their pathogenicity) (Guyton) |
|
|
|
Atopy\Atopic allergy
|
A genetically determined state of hypersensitivity to environmental allergens
(Atopia: strangeness. A-: topos: a place) (Stedman) |
|
|
|
Allergy
a. Reagin b. Allergen |
a. Reagin or sensitizing antibodies. Antibodies that mediate hypersensitivity reactions (IgE in humans)
b. An antigen that reacts specifically with a specific type of IgE reagin antibody (Guyton) |
|
|
|
Basophils and mast cells
a. Released substances |
a.
1. Histamine 2. Proteases 3. Slow-reacting substances of anaphylaxis (LTC4, LTD4, LTE4) (These can cause spasm of the smooth muscles of the bronchioles, eliciting an asthma-like attack, sometimes causing death by suffocation) 4. Eosinophil chemotactic substance 5. Neutrophil chemotactic substance 6. Heparin 7. Platelet activating factors (Guyton) |
|
|
|
Allergic reactions
a. Urticaria b. Hay fever c. Asthma |
a. Results from allergens entering specific skin areas and causing localized anaphylactoid reactions. Vasodilation -> red flare, increased permeability -> swelling (hives)
(Antihistamines are effective) b. The allergen-reagin reaction occurs in the nose (histamine -> vasodilation & increased permability -> swollen, hypersecretion) (Antihistamines are effective) c. Allergen-reagin in bronchioles of the lungs (the slow-reacting substances of anaphylaxis (LT C4 D4 E4) is believed to vause spasm of the bronchiolar smooth muscle) (Administration of antihistamines is not very effective) (Guyton) |
|
|
|
Blood transfusion
a. Agglutinogens b. Agglutinins c. Effect by mixing |
a. Antigens found on surface of blood cells that can cause blood agglutination
b. Antibodies against agglutinogens, most are IgG and IgM c. 1. Agglutination 2. Delayed hemolysis by phagocytosis or physical distortion by agglutination 3. Acute hemolysis due to lytic complement complex (Rare, require high agglutinin concentration and IgM (these are called hemolysins) (Guyton) |
|
|
|
What does the ABO blood group system classify according to?
|
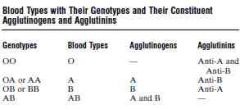
Presence of agglutinogens (antigens)
(These are determined by 1 gene, one on each chromosome) (O (47%) and A (41%) are most common. B (9%), AB (3%)) (Guyton) |
|
|
|
Rh antigens
a. Main difference compared to ABO system b. Components c. Most prevalent and most antigenic |
a. Antibodies to Rh does not develop spontaneously, the person must first be massively exposed to an Rh antigen
b. C,D,E,c,d,e (can have big or small letter) c. D. Someone with the D antigen is said to be Rh+ (There can still be transfusion reactions in an Rh- person, but it will usually be milder) (Prevalence: 85% Rh+ of white people, 95% in american blacks, and almost 100% in african blacks) (It takes 2-4 months after exposure to Rh antigen before the anti-Rh agglutinins reach their maximum concentration, its high variability between individuals) (Guyton) |
|
|
|
Erythroblastosis fetalis
a. Cause b. Risk in 1st, 2nd, and 3rd child c. Treatment\Prevention |
a. Rh+ agglutinogen from fetus (from father) is exposed to the maternal circulation which develops anti-Rh agglutinins. These diffuse through the placenta into the fetus and cause agglutination, hemolysis, hyperbilirubinemia, jaundice, kernicterus..
b. Next to none in first child, 3% in second child, 10% in third child c. 1. Treat by replacing infant's Rh+ positive blood with Rh- 2. Prevent by giving anti-D antibody to susceptible mothers (Start at 28-30 weeks, also given to prevent sensitization to Rh- negative women with their first Rh+ baby) (It works by binding any fetal red cells with the D antigen before the mother is able to produce an immune response and form anti-D IgG) (Guyton) |
|
|
|
Cause of acute kidney shutdown after transfusion reactions (3)
|
1. Renal vasoconstriction
(the antigen-antibody reaction of the transfusion reaction releases toxic substances from the hemolyzing blood cells that cause vasoconstriction) 2. Circulatory shock (from loss of rbcs, toxic substances released from hemolyzed cells, and products of immune reaction) 3. Renal tubular blockage (If the Hb released is higher than can bind with haptoglobin. Hb can only slightly reabsorbed from the renal tubules, thus when the renal filtrate is concentrated by reabsorption of water, Hb can precipitate) (Guyton) |
|
|
|
Transplantation
a. Autograft b. Isograft c. Allograft d. Xenograft |
a. Autograft
Transplant of a tissue or whole organ from one part of the same animal to another part b. Isograft From one identical twin to another c. Allograft From one human being to another (or between individuals of same species) d. Xenograft Cross-species (Guyton) |
|
|
|
Immune reactions in transplant tissue
a. The most important antigens for causing graft rejection? b. How many do we have? |
a. HLA antigens
b. 6 (About 150 to choose from) (Some of the HLA antigens are not severely antigenic, for which reason a precise match of some antigens between donor and recipient is not always essential to allow allograft acceptance) (Guyton) |
|
|
|
Hemostasis
a. What? b. The four steps |
a. Prevention of blood loss
b. 1. Vascular constriction 2. Formation of a platelet plug 3. Formation of a blood clot as a result of blood coagulation 4. Eventual growth of fibrous tissue into the blood clot to close the hole in the vessel permanently (Guyton) |
|
|
|
Vascular constriction in hemostasis -mechanism (3)
|
1. Local myogenic spasm (initiated by direct damage to the vascular wall)
2. Local autacoid factors from the traumatized tissue and from platelets (ie TXA2) 3. Nervous reflexes (via pain afferents?) (Guyton) |
|
|
|
Platelets - functional characteristics (8)
|
1. Contractile proteins - actin & myosin, trombosthenin (protein that can cause the platelets to contract)
2. Residuals of GA and ER -> enzymes, store Ca2+ 3. Mitochondria & other enzyme systems -> ATP formation 4. Enzymes for prostaglandin synthesis 5. Fibrin-stabilizing factor 6. A growth factor - for vascular endothelial cells, vascular smooth muscle cells, and fibroblasts (all the components of the vessels) 7. Cell membrane have coat of glycoprotein that repulse normal endothelium and adhere to injured areas, especially exposed collagen 8. The membrane contains large amounts of phospholipid, which can activate many stages in the blood coagulation process (Guyton) |
|
|
|
Mechanism of platelet plug
|
<- Damaged vascular surface, especially collagen ->
1. Platelets swell & assume irregular forms with pseudopodia 2. Contract -> extrude granules -> ADP, TXA2, 3. Become more "sticky" (adhere more to each other, collagen, and von Willebrand factor: protein that leaks into the traumatized tissue from plasma) (Followed by invasion of fibrin threads.) (Extremely important for closing minute ruptures in very small vessels) (Guyton) |
|
|
|
The three essential steps of blood coagulation
|
1. Rupture of the vessel\damage to the blood -> chemical cascade -> prothrombin activator is formed (rate limiting step)
2. Prothrombin activator actives prothrombin to thrombin (need sufficient amounts of Ca) 3. Thrombin convert fibrinogen to fibrin fibers (that enmesh platelets, blood cells, and plasma to form the clot) (Guyton) |
|
|
|
Fibrinogen
a. Size |
a. 340 kD
(Because of this, little of it normally leaks to the interstitial fluid. Since it is an essential part of the coagulation process, interstitial fluid normally don't clot) (Guyton) |
|
|
|
Fibrin-stabilizing factor
a. <-? (2) b. Activated by c. Function |
a. <- plasma, released from platelets (entrapped in the clot)
b. Thrombin c. Has enzymatic ability to catalyze formation of covalent bonds between fibrin monomers (before this they are only linked by hydrogen bonding) (Guyton) |
|
|
|
Initiation of coagulation: formation of prothrombin activator
a. The 3 causes b. Which belong to intrinsic and which to extrinsic |
a.
1. Trauma to the vascular wall and adjacent tissues 2. Trauma to the blood 3. Contact of the blood with damaged endothelial cells, collagen, and other tissue elements outside the blood vessel b. Extrinsic pathway = 1 (by release of tissue factor) Intrinsic pathway = 2,3 (Guyton) |
|
|
|
Extrinsic pathway for initiating clotting
a. Caused by b. Steps |

a.Traumatized vascular wall or traumatized extravascular tissue that come in contact with blood.
b. 1. Release of tissue factor( tissue thromboplastin\factor III) (Complex of phospholipids from the membranes of the tissues plus a lipoprotein complex, catalytic) 2. Activates VII and in the presence of Ca also X, VII helps to activate X 3.X combines with phospholipids (from tissue factor or released from platelets and V to form prothrombin activator (Works in presence of Ca) (V is inactive at first, then activated by thrombin (positive feedback!). V is also caused proaccelerin because when it is activated it is an additional strong accelerator of prothrombin activation) (Guyton) |
|
|
|
Intrinsic pathway for initiating clotting
a. Cause b. Steps |
a. Trauma to the blood itself, exposure of the blood to collagen from a traumatized blood vessel wall
b. 1. Blood trauma or collagen exposure -> activate XII, release platelet phospholipids (XII can also be activated by ie glass) (blood trauma damage platelets -> release platelet phospholipids (contain the lipoprotein platelet factor 3) 2. XII activate XI (Require HMW-kininogen, accelerated by prekallikrein) 3. XI activate IX 4. X is activated by a. IX b. VIII (hemophilia) c. platelet phospholipids (thereunder platelet factor 3) (Thus this step require both clotting factors and platelets) 5. X combine with V and platelet or tissue phospholipids to form prothrombin activator (Guyton) |
|
|
|
Intrinsic pathway for initiating clotting
a. Cause b. Steps |

a. Trauma to the blood itself, exposure of the blood to collagen from a traumatized blood vessel wall
b. 1. Blood trauma or collagen exposure -> activate XII, release platelet phospholipids (XII can also be activated by ie glass) (blood trauma damage platelets -> release platelet phospholipids (contain the lipoprotein platelet factor 3) 2. XII activate XI (Require HMW-kininogen, accelerated by prekallikrein) 3. XI activate IX 4. X is activated by a. IX b. VIII (hemophilia) c. platelet phospholipids (thereunder platelet factor 3) (Thus this step require both clotting factors and platelets) 5. X combine with V and platelet or tissue phospholipids to form prothrombin activator (Guyton) |
|
|
|
Petechiae (pinpoint red dots on the skin) are more common in dysfunction of platelets or coagulation factors, whereas deep bleeding is more common when there is a disorder of?
|
Platelets
Coagulation factors (Berkowitz) |
|
|
|
Which coagulation factors need vitamin K as a cofactor for their synthesis?
|
II, VII, IX, X
(Berkowitz) |
|
|
|
Prothrombin time (PT) and partial thromboplastin time (PTT)
a. Which measure in extrinsic pathway (VII more selectively)? b. Which measure intrinsic pathway (factor XII, XI, IX, VIII more selectively)? |
a. PT -> extrinsic (VII)
b. PTT -> intrinsic (XII, XI, IX, VIII) (PTT is a longer name than PT and the intrinsic pathway has more factors) (PTT has an extra T INside it and it measures the INtrinsic pathway) (Ofcourse both of them also measure the final common pathway) (Berkowitz) |
|
|
|
Coumadin
a. Effect b. Mechanism b. Extrinsic or intrinsic pathway? use PT or PTT? |
a. Anticoagulant by affecting the vitamin K-dependent factors II, VII, IX, X, and regulatory proteins S, C, Z
b. antagonist to vitamin K epoxide reductase (VKOR)) which is needed to replenish vitamin K for its co-factor function for gamma-glutamyl carboxylase which form a new carboxy group on glutamyl residues. This carboxy group binds to Ca, which form a bridge between clotting factors and phospholipids (Takes 8-12 hours to function, and may not peak until 3-4 days) c. Extrinsic is most affected, therefore PT is used (Berkowitz) |
|
|
|
Heparin
a. Effect b. Extrinsic or intrinsic pathway? use PT or PTT? |
a. Increase antithrombin III activity
b. Intrinsic pathway -> PTT (Intrinsic = PTT = XII, XI, IX, VIII = heparin. HINT = Heparin = INTrinsic pathway) (Berkowitz) |
|
|
|
Time for clotting
a. In extrinsic pathway b. In intrinsic pathway |
a. 10-15 seconds
b. 1-6 minutes (Guyton) |
|
|
|
Preventon of blood clotting in the normal vascular system - intravascular anticoagulants (7)
|
1. The smoothness of the endothelial surface
(Prevent contact activation of the intrinsic pathway) 2. A layer of glycocalyx on the endothelium (mucopolysaccharide, repel clotting factors and platelets) 3. Thrombomodulin - protein on endothelial membrane (a. Bind and thus inhibit thrombin. b. activate protein C) 4. Protein C (Activated by thrombomodulin, inactivates V and VIII) 5. Fibrin fibers - adsorb thrombin (Adsorb up to 90% of thrombin -> control the clotting process and keep it localized) 6. Antithrombin III - inactivate thrombin, potentiated by heparin up to a thousandfold (Also inactivate XII, XI, X, IX) 7. Plasminogen\Profibrinolysin -> Plasmin\Fibrinolysin (proteolytic enzyme (like trypsin) that inactivate fibrin, II, V, VIII, XII) (activated by tissue plasminogen activator (tPA) formed slowly by injured tissue and vascular endothelium) (Guyton) |
|
|
|
Hemophilia
a. 85% of cases is due to? b. 15% of cases is due to? c. Genetics |
a. Abnormality\deficiency of factor VIII - hemophilia A
b. Mainly abnormality\deficiency of factor IX - hemobilia B c. X-recessive (Factor VIII has two components - one large (von Willebrand factor) and one small (the one affected in hemophilia A) (Guyton) |
|
|
|
von Willebrand factor
a. Function b. Name of disease? |
a. Circulates in the blood bound to factor VIII. Binds to vessels that have lost their endothelial cell linings, creating a surface to which platelets can adhere.
(Binds to collagen, platelet gpIb, gpIX and gpV receptors) (Made of endothelial cells and megakaryocytes) b. von Willebrand disesae |
|
|
|
Cause of thromboembolic conditions - two main factors
|
1. Any roughened endothelial surface <- arteriosclerosis, infection, trauma
2. Slowly flowing blood (Guyton) |
|
|
|
Disseminated intravascular coagulation
a. Cause b. Effect (2) |
a. Often as a result of presence of large amounts of traumatized or dying tissue in the body that release great quantities of tissue factor into the blood.
(Ie in septicemia, endotoxin is an effective activator of the clotting system. This exacerbates septicemic shock, which is deadly in > 85% of patients) b. Numerous small blood clots are formed in the small peripheral blood vessels -> exacerbate shock by increasing tissue ischemia Can deplete clotting factors and cause increased bleeding (Guyton) |
|
|
|
Bleeding time
a. Procedure b. Value b. Especially indicative of |
a. Pierce the tip of the finger or lobe of the ear
b. Bleeding normally stops within 1-6 minutes c. Thrombocytopenia (Guyton) |
|
|
|
Prothrombin time (PT)
a. Procedure b. Used for heparin or coumadin? c. Value |
a.
1. Remove blood and oxalate it immediately 2. Add excess of Ca and tissue factor to activate extrinsic pathway 3. Observe time to clotting (The time is determined mainly by prothrombin concentration) b. Coumadin c. About 12 seconds (Guyton) |
|

