![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
67 Cards in this Set
- Front
- Back
|
mullerian duct in male?
|
regress via Muellerian inhibiting factor (MIF) released from testes
Wolffian duct develops instead |
|
|
mullerian duct in female?
|
develop fully (into fallopian tube, uterus, and upper part of vagina)
|
|
|
induces the development of undifferentiated gonads into testes
|
Y chromosome induces production of Testicular Determining Factor (TDF),
which induces dev. of undifferentiated gonads into testes |
|
|
Muellerian inhibiting factor (MIF); MIF induces:
|
MIF released from testes induces:
1. regression of Muellerian ducts 2. stimulation of Leydig cells + testosterone -> Wolffian ducts develop |
|
|
Testicular function is ___ sensitive in most mammals
|
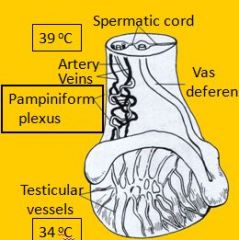
Testicular function is temperature sensitive in most mammals
Optimum: 2 – 6 degree celcius below core temperature |
|
|
Descent of testes into scrotum through inguinal rings occurs when?
|
Usually completed during last days / weeks of gestation
* except dogs/cats: first days post partum |
|
|
failure of one or both testes to descend
|
Cryptorchidism
|
|
|
ined testes show higher incidence of ____?
|
neoplasms (Sertoli cell tumors)
|
|
|
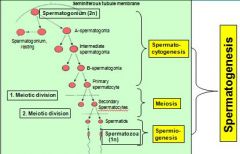
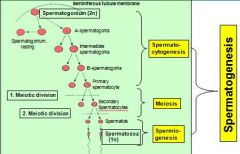
Identify stages of spermatogenesis (early to late)?
|

spermatogonia (stem)
Primary spermatocytes, Secondary spermatocytes (short-lived) Spermatid, Spermatozoa |
|
|
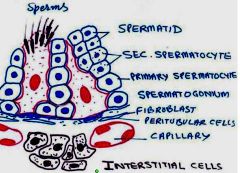
Testes contain 2 functional compartments:
|
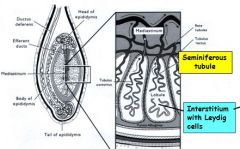
1. Tubular compartment = seminiferous tubules
2. Interstitial compartment = Leydig cells |
|
|
site of SPERMATOGENESIS
|
Tubular compartment = seminiferous tubules =
|
|
|
site of TESTOSTERONE production
|
Interstitial compartment = Leydig cells = site of TESTOSTERONE production
|
|
|
Stages of spermatogenesis (early to late)
|

spermatogonia,
Primary spermatocytes, Secondary spermatocytes, Spermatid, Spermatozoa |
|
|
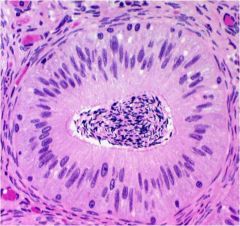
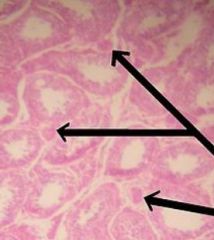
What are the three (two are cellular) components of the seminiferous tubules?
|
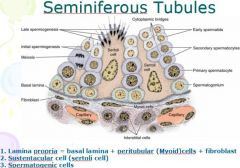
1. lamina propria = basal lamina + peritubular + FB
2. sustebtacular or sertoli cells (supportive) 3. spermatogenic cells |
|
|
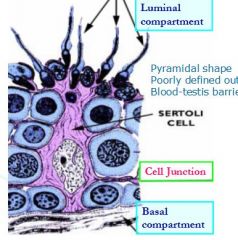
Tubular compartment (seminiferous tubules) contains
|
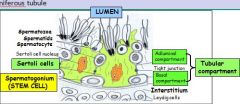
Tubular compartment contains host cells (=Sertoli cells) and germinal stem cells
note: tight junctions divide the tubule into basal and adluminal compartment = blood - testis barrier (protects sperm cells against auto-immune reactions |
|
|
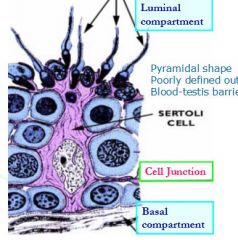
true "resident cells" of the seminiferous tubule?
|
Sertoli cells
Sertoli cells are really the only true "resident cells" of the seminiferous tubules. The various stages of spermatozoal development all are destined to mature and be used up, but Sertoli cell is present before puberty and remains in place until death. |
|
|
Which cells make up the blood-testis barrier?
Main purpose of this? |
Sustentacular (sertoli) cells
- purpose is to protect haploid gametes (haploid spermatocytes and spermatogonia?) from immune system. |
|
|
What are some of the funcitons of sertoli cells?
|
- Phagocytosis of degenerating spermatogenic cells (consume residual cytoplasm)
- Production of Mullerian inhibitory hormone - Secretion of introtubular fluid nursing cells inside - their tight junctions make-up blood-testis barrier (seperates interstitial blood in testis from lumen in seminif.tubules) |
|
|
Which spermatogenic cells is small and situated next to the basal lamina?
(describe location of cells in relation to others) |
Spermatogonium (stem cells)
Stem cell and earliest stage. Spermatogonia are densely stained, round nuclei. These are diploid cells, and they're in the basal compartment created by the Sertoli cells. > As stem cells divide and transform, they migrate towards the luminal side, always in close contact with Sertoli cells |
|
|
Which spermatogenic cells are the largest and have obvious condensed chromosomes?
|
Primary spermatocytes
Initial product of spermatogonial maturation (after spermatogonium); large cells with a round nucleus filled with clumped chromatin material. May see in various stages of meiotic cycle. |
|
|
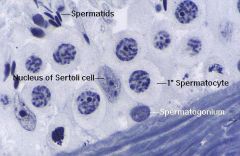
Which spermatogenic cells are short-lived and difficult to observe?
|

Secondary spermatocytes
Very short-lived and difficult to distinguish from primary spermatocyte. By time cells have progressed to spermatocyte stage, meiosis is complete; hence secondary spermatocytes are haploid. |
|
|
Which cells are small, towards the lumen of seminiferous tubules, and undergo spermiogenesis to form spermatozoa?
|
Spermatids
Spermatids will be seen in different stages of maturation. Some will be chunky and squarish-looking cells with nuclei beginning to get quite dense. Others more advanced will be narrow and have tails beginning to develop. |
|
|
Which cells appear in the interstitial space of the testis during puberty?
|
Interstitial or Leydig cells
|
|
|
What is the function of the epididymis?
|
Maturation (head and body)
Storage (Tail) |
|
|
Which accessory male sex gland is absent in dogs and cats (carnivores)?
|
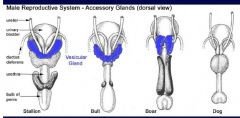
vesicular gland (aka seminal vesicle)
|
|
|
What are the accessory male sex glands?
Which responsible for secreting pre-ejaculate fluid? Which not in carnivores? |
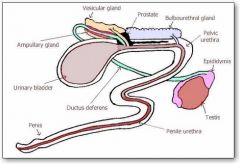
Ampulla (Terminal part of ductus deferens)
Vesicular gland (seminal vesicle; not in carnivores) Prostate gland Bulbourethral gland (pre-ejaculate) note: image included may be of human anatomy, be aware of discrepancies |
|
|
Which part of the prostate gland is absent in SMALL ruminants?
|
Body or compact portion absent in goats and sheep
|
|
|
Which part of the prostate gland is absent in horses?
|
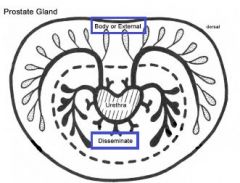
Pars disseminata (internal part) - thin layer of the prostate that surrounds the urethra; as distinct from the body of the gland.
|
|
|
Prostate Gland most developed in?
least developed in? |
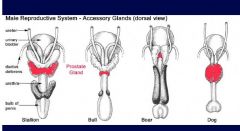
Most developed in dogs and horses.
Smaller in cats, pigs and ruminants. |
|
|
Produce testosterone for secondary male sex characteristics?
|
Leydig (interstitial) cells - located near ST in testis
|
|
|
__________ is region responsible for transport and maturation of spermatozoa.
|
Epididymis
|
|
|
= secretions of epididymis, ampullae, vesicular, prostate and bulbourethral
glands |
Seminal fluid = secretions of epididymis, ampullae, vesicular, prostate and bulbourethral
glands |
|
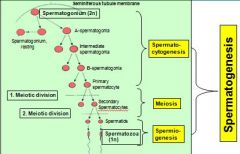
Does spermatocytogenesis (making primary spermatocyte) occur before or after meiosis?
is secondary spermatocyte haploid or diploid? |
before
haploid (only 1 meiotic division) |
|
In most domestic species, spermatogenesis requires __ days
|
spermatogenesis requires 40 – 60 days
|
|
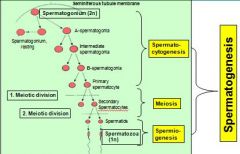
differentiation from spermatid to spermatozoa know as ?
|

Spermiogenesis
spermatid is after 2nd meiotic division but still need to transform into sperm (spermatozoa) |
|
|
What is it called when spermatozoa are released into epididymis after sper-
matogenesis? Are they mobile and capable of fertilization at this point? |
SPERMIATION: spermatozoa are released into epididymis ; are still immobile and not capable of fertilization
|
|
|
Time frame for mitotic cycles?
|
Mitotic stem cell division occurs in cycles of 10-14 days (= once every 10-14 days)
=> cells in 1 layer belong to 1 generation 4 – 5 layers of separate generations occur in every section ( 40-60 days / 10-14 days) |
|
|
Cycles in adjacent sections of a seminiferous tubule are co-ordinated = begin at
successive time intervals => spermatozoa mature and are released in adjacent sections of a tubule in a sequential manner |
spermatogenic wave
|
|
|
Purpose:
of spermatogenic cycles and waves? |
spermatogenic cycles and waves guarantee continual sperm production
Daily sperm production: several billion / day |
|
|
Transit time: for sperm through epididymis?
|
Transit time: ca. 9-14 days
thr. epididymis |
|
|
External indicator of sperm maturity
|
loss
of cytoplasmic droplet |
|
|
sperm is inhibited, achieved by several factors
|
citric acid, low pH, high CO2, low Temp.)
|
|
|
what happens to sperm concentration with high freq. mating?
|
with high frequency mating, sperm number per ejaculation drops -> lowered fertility
|
|
|
Ampullae Absent in ?
|
Ampullae Absent in PIG
secrete mucloid fluid |
|
|
encircles urethra, partially embedded in urethral muscle
secretions contain electrolytes, prostaglandins, clotting enzyme |
Prostate gland
|
|
|
absent in dogs; major gland in boars
> secretions contain mucus and fibrinogen cause ‘dribbling’ in bulls before copulation (flushing effect) |
Bulbourethral glands : secretions contain mucus and fibrinogen
- cause ‘dribbling’ in bulls before copulation (flushing effect) |
|
|
Functions of seminal fluids:
|
Functions of seminal fluids:
- to flush sperm through the urethra - to provide sperm with nutrients + buffers after ejaculation |
|
|
sperm undergoes activation and final maturation where/when?
(this is supported by?) |
After ejaculation, sperm undergoes activation and final maturation while traversing the female system!
Seminal fluid provides means for sperm survival. |
|
|
energy source for sperm?
|
Fructose / sorbitol main energy source for sperm
|
|
|
_____ affect female mucus to facilitate sperm motility
(unanswered question) |
Prostaglandins
But what is source of prostaglandin? |
|
|
What is it called when cholesterol layer around acrosome thins while sperm is migrating -> weakens acrosomal membrane -> becomes permeable for Ca -> facilitates whiplash movements
|
Capacitation
Capacitation requires 1-10 hours |
|
|
Capacitation requires ?
|
(Capacitation seems to require glucosaminoglycans (GAG) produced in the female
tract, e.g. heparin; higher concentrations of GAG during estrus) |
|
|
Sperm releases what expose receptors on egg???
-> dissolve intercellular cement between granulosa cells of ovum -> liberate receptor sites (glycoproteins) on zona pellucida |
Sperm releases hyaluronidase and proteolytic enzymes (acrosin)
|
|
|
Binding initiates ACROSOME REACTION what is this?
|
Bind of sperm-ovum initiates :
massive influx of Ca -> acrosome dissolves at anterior head of sperm -> enzyme release -> localized digestion of zona pellucida |
|
|
How does ovum block additional sperm / avoid polyspermy?
|
Ovum reacts with:
-> Ca release, leading to immediate depolarization of ovum membrane -> activation of cortical granules with exocytosis of enzymes -> structural changes of receptor sites (=zona reaction) |
|
|
Are any (female) oocytes present at birth?
If so, are they fully mature? What stage in? |
Yes
meiosis inhibiting factor -> arrests oocyte development during prophase of the first meiotic division = PRIMARY OOCYTE (2n) |
|
|
T/F Primordial follicles are present at time of birth
|
True
|
|
|
T/F In cats, number of primary oocytes is fixed at time of birth
|
False, number of primary oocytes is fixed at time of birth in all, EXCEPT cats
|
|
|
Follicular growth occurs when?
(check on this) |
Follicular growth occurs during cyclic ovarian activity; usually only after puberty
(but sometimes even before puberty) |
|
|
folliculogenesis begins when?
|
don't know
|
|
|
Towards the end of folliculogenesis, meiotic
inhibitors are removed (when __ becomes dominant) this leads to: ? |
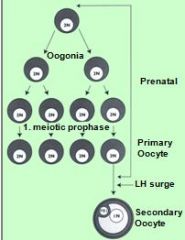
lutenizing hormone
meiosis continues with formation of polar body = SECONDARY OOCYTE (1N) |
|
|
OVULATION releases _____ oocytes, except in ___.
|
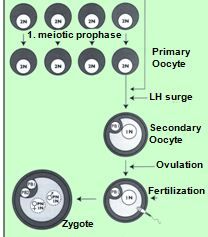
OVULATION releases secondary oocytes
Exception: dog releases primary oocytes |
|
|
2nd meiotic division with second polar body occurs during ___
and is completed ______. |
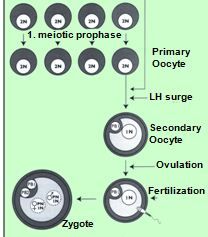
2nd meiotic division with second polar body occurs <during oviduct passage> and is completed -> only after fertilization
|
|
|
T/F estrogen influence fluid flow during ovulation?
|
True
|
|
|
? = site of fertilization
how long does egg remain here? |
- Remains at ampulla-isthmus junction for 2-3 days
= site of fertilization |
|
|
Where does capacitation occur?
|
* capacitation occurs after ejaculation -> inside uterus
|
|
|
Are seconary oocytes (female) present at or just after birth?
If called secondary oocytes, have they completed 2nd mitotic division (1n)? |
don't know, but i think so
don't think so |

