![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
92 Cards in this Set
- Front
- Back
|
Prenatal development
a. Embryonic period - embryo b. Fetal period - fetus c. Fetal viability border - time and weight |
a. From conception to the 8th week.
b. From 9th week to parturition. c. 24th week, 600g (Dpt of gynecology & obstetrics, 3LF) |
|
|
Delivery term
a. Length of physiological pregnancy - days, weeks, months b. Conceptional age - what, length of pregnancy c. Menstrual age - what, length of pregnancy |
a. 280 days = 40 weeks = 10 months
b. From conception, 266 days\38 weeks c. From 1st day of last menstrual period, 280 days\40 weeks (Dpt of gynecology & obstetrics, 3LF) |
|
|
Naegele's formula
|
EDT = LMP - 3M + 7D
(Dpt of gynecology & obstetrics, 3LF) |
|
|
Which ultrasound measurements are used to determine the age of the fetus (6)
|
1. Gestational sac diameter
(Amniotic sac, fluid, and placenta) 2. CRL - Crown-rump length (A measurement from the skull vertex to the midpoint between the apices of the buttocks of an embryo or fetus) 3. BPD - Biparietal diameter (The diameter of the fetal head between the two parietal eminences) 4.HC - Head circumference 5. AC - Abdominal circumference 6. FL - Femur length (Dpt of gynecology & obstetrics, 3LF) |
|
|
Fetal development - 3rd month\week 9-12
a. Weight b. Length (CRL) c. Characteristics (3) |
a. 15g
b. 55 mm (CRL) c. 1. Disproportion between head and trunk and upper and lower extremities 2. Indifferent external genitalia 3. Presence of kidneys (Dpt of gynecology & obstetrics, 3LF) |
|
|
Fetal development - 4th month\week 13-16
a. Weight b. Length (CRL) c. Characteristics (4) |
a. 105 g
b. 112 mm c. 1. Fast growth 2. Normalizing of disproportion 3. Ossification 4. External genitalia (Dpt of gynecology & obstetrics, 3LF) |
|
|
Fetal development - 5th month\17-20 week
a. Weight b. Length (CRL) c. Characteristics (5) |
a. 310g
b. 25 cm (CRL) c. 1. Proportional length of extremities 2. Lanugo\Downy hair (Fine, soft, lightly pigmented fetal hair with minute shafts and large papillae) 3. Vernix caseosa (The fatty substance, consisting of desquamated epithelial cells, lanugo, and sebaceous matter, covers the skin of the embryo) 4. Hairs and eyelashes 5. Movements (Dpt of gynecology & obstetrics, 3LF) |
|
|
Fetal development - 6th month\21-24 week
a. Weight b. Length (CRL) c. Characteristics (3) |
a. 640 g
b. 30 cm (CRL) c. 1. Weight doubled from fifth month 2. Open eyes 3. Viability |
|
|
Fetal development - 7th month\25-28 weeks
a. Weight b. Length (CRL) c. Characteristics (1) |
a. 1000 g
b. 35 cm c. 1. Fatty tissue (+ hairs and eyelashes, vernix caseosa, open eyes, lanugo) (Dpt of gynecology & obstetrics, 3LF) |
|
|
Fetal development - 8th month\week 29-32
a. Weight b. Length (CRL) c. Characteristics (3) |
a. 1600 g
b. 40 cm c. 1. Increased fatty tissue 2. Pink skin 3. Respiration? (Dpt of gynecology & obstetrics, 3LF) |
|
|
Fetal development - 9-10th month\week 33-40
a. Weight b. Length (CRL) c. Characteristics (3) |
a. 2500-3000 g
b. 45-50 cm c. 1. Fatty tissue +++ 2. Hairless skin 3. Respiration (Dpt of gynecology & obstetrics, 3LF) |
|
|
Signs of fetal maturity
|
1. Weight > 2500 g
2. Length > 50 cm 3. Pink smooth skin 4. Fatty tissue + 5. Rounded shapes 6. Presence of eyelash (hair on eyelid) and eyebrows (hair on superior edge of orbit) 7. Hair several cm long 8. Nails reaching the tips of the fingers 9. Skull bones hard - fonticulus major (ant.) and minor (post.) are divided 10. Genitalia I. Boys - testicles inside of scrotum II. Girls - labia minora hidden between labia mjaora (Dpt of gynecology & obstetrics, 3LF) |
|
|
Fetal position in utero
a. Situs - synonym, what b. The 3 types |
a. Lie.
Relationship between long axis of fetus and long axis of uterus b. 1. Longitudinal - head (99.5%), breech (3%) 2. Transverse 3. Oblique (Dpt of gynecology & obstetrics, 3LF) |
|
|
Fetal position in utero
a. Position b. Habitus - synonym, what c. Praesentatio\Presentation |
a.
I. Longitudinal situs\site -> Relationship between back of fetus and the side of the uterus (Right, Left) II. Transverse site\situs -> Relationship between head and uterus side (Left, right) b. Habitus\Attitude Relationship among parts of the fetal body (Habitus: the physical characteristics of a person) c. Relationship of leading parts of the fetal body (most often the head) to the pelvic brim (Lie of fonticulus ant., post., and sagittal suture in the pelvic planes) (Dpt of gynecology & obstetrics, 3LF) |
|
|
Delivery
a. Definition b. Preterm delivery c. In term delivery d. After term delivery |
a. Delivery of live newborn weighing > 500g, delivery of fetus of weight < 500g that live more than 24h, or delivery of dead fetus weighing > 1000g
(>500g, <500g, >1000g) b. < 38 weeks c. 38-42th week d. > 42 week (Dpt of gynecology & obstetrics, 3LF) |
|
|
Delivery - the 4 stages, characteristics and duration
|
1. Dilation stage
12-18h (4-10h) Regular contraction of uterus -> dilation of cervix 2. Expulsion stage 1h (10-20min) Cervix is fully dilated, fetus is expulsed through the pelvis 3. Placental stage 30-60min Expulsion of placenta and fetal membranes 4. 4th period 2h after delivery Uterus contract and retract (shrink and pull back) (When bleeding can occur) (Dpt of gynecology & obstetrics, 3LF) |
|
|
Delivery - head presentation
a. Leading point b. Mechanism (5) |
a. Fonticulus minor\Posterior fontanelle
b. 1. Flexion 2. Progression 3. Internal rotation (from side to down) 4. Extension 5. External rotation (From down to side) (Dpt. of obstetrics and gynecology, LF3) |
|
|
Umbilical cord - what, composition at birth
|
The definite connecting stalk between the embryo\fetus and the placenta.
At birth it is primarily composed of Wharton's jelly in which the umbilical vessels- 2 arteries, 1 vein, is embedded. (Wharton's jelly - the mucous connective tissue of the umbilical cord) (Stedman) |
|
|
Placenta accreta and percreta
a. Placenta accreta b. Placenta percreta |

a. The abnormal adherence of the chorionic villi to the myometrium.
(Placenta increta is a form of placenta accreta in which the chorionic villi invade the myometriumm) (Associated with partial or complete absence of the decidua basalis and, in particular, the stratum spongiosum.) (Accretio - to grow together) b. The term applied when the villi have invaded the full thickness of myometrium or through the serosa of the uterus, causing incomplete or complete rupture, respectively. (Stedman) |
|
|
Placenta adherens
|
Retained placenta following delivery due to failure of contraction of the myometrium behind the placenta.
|
|
|
What are the three main types of retained placenta following vagina delivery
|
1. Placenta adherens
(Failed contraction of the myometrium behind the placenta) 2. Trapped placenta (A detached placenta trapped behind a closed cervix) 3. Partial placenta accreta (A small area of accreta preventing detachment) (Obstetrics School of Reproductive and Developmental Medicine, Liverpool Women's Hospital) |
|
|
Multiple pregnancies
a. Occurrence in normal population of twins b. Occurrence in normal population of triplets |
a. 1%
b. 0.01% (Dpt. of obstetrics and gynecology, LF3) |
|
|
Dizygotic twins
a. Proportion of total twins b. Mechanism c. Composition of fetal membranes |
a. 2\3
b. Fertilization of two female and two male gametes c. Two zygotes, two amnions, and the chorions and placenta can be fused or split. (Dpt. of obstetrics and gynecology, LF3) |
|
|
Monozygotic twins
a. Mechanism b. Composition of the fetal membranes |

a. Fertilization of one ovum.
(-> always the same sex and the same phenotype) b. Depend on the time of twinning 1. Twinning during 2-8 cell stage Each has its own amnion, chorion, and placenta. (Biamnati, bichoriati) (The chorion and placenta can fuse) (Split after degradation of zona pellucida -> implant separately) 2. During the blastocyst stage Own amnion, share chorion and placenta (Biamniati, monochoriati) (Danger of growth restriction of one twin because of blood perfusion preference to the second one) (The embryonic bud divides itself in the interior of the same blastocyst cavity into two embryoblasts -> both has the same chorion and placenta, but have their own amnion) 3. During notogenesis\prior to primitive streak (bilaminar embryoblast stage) Share all - amnion, chorion, placenta (Monoamniati, monochoriati) (Danger of conjoined twins) |
|
|
Twins
a. When is there increased risk of conjoined twins b. What are the two main groups of conjoined twins, and what are the subdivisions |
a. With monoamniati
(Twinning during notogenesis) b. 1. Conjoined\Symmetric\Siamese twins Thoracopagus (pagos - something fastened) - conjoined twins with union in the thoracic region) Craniopagus - conjoined twins with fused skulls Dicephalus - conjoined twins with two separate heads Dipygus (pygus - buttocks) - conjoined twins with a single head and thorax and the pelvis and lower extremities duplicated. Xiphopagus - conjoined at the xiphoid process of the sternum Pygopagus - conjoined at buttocks 2. Parasitic\Asymmetric twins - thoracopagus parasiticus (Dpt. of obstetrics and gynecology, LF3, Stedman) |
|
|
Intrauterine position of twins at the end of pregnancy
|
45% - both head position
35% - one head, one breech position 10% - both breech position 9% - one longitudinal, one transverse (Dpt. of obstetrics and gynecology, LF3) |
|
|
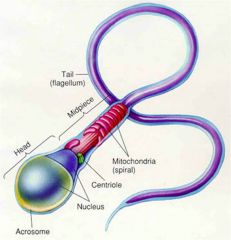
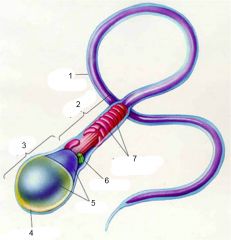
(Flagellum - A whiplike locomotory organelle, consist of nine double peripheral microtubules and two single central microtubules; it arises from a deeply staining basal granule, often connected to the nucleus by a fiber, the rhizoplast. Though characteristic of the protozoan class Mastigophora, comparable structures are commonly found in many other groups, e.g., in spermatozoa.)
(Centriole - tubular structure with a wall having 9 triple microtubules, usually seen as paired organelles lying in the cytocentrum) (Acrosome (acro- tip): A caplike organelle or saccule derived from the golgi that surrounds the anterior two-thirds of the nucleus of a sperm cell. Within this cap are enzymes that are thought to facilitate entry of the sperm through the zona pellucida.) (Stedman) |
|

|
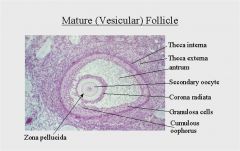
(Theca ('sheath', 'capsule') interna\Tunica ('coat') interna thecae folliculi -
The inner cellular and vascular layer of the vesicular ovarian follicle, there is evidence that the epithelioid cells produce estrogen and contribute to the formation of the corpus luteum after ovulation) (Theca externa\Tunica externa thecae folliculi - the external fibrous layer of the theca of a well-developed vesicular ovarian follicle) (Granulosa cells - a cell of the membrana granulosa lining the vesicular ovarian follicle that becomes a luteal cell of the corpus luteum after ovulation) (Cumulus oophorus - a mass of epithelial granulosa cells surrounding the ovum in the ovarian follicle (cumulus - a colleaction\heap of cells)) (Corona radiata - a single layer of columnar granulosa cells derived from the cumulus oophorus, anchor on the pellucid zone of the oocyte in a secondary follicle) (Vesicular ovarian\antral\graafian\secondary follicle - a follicle in which the oocyte attains its full size and is surrounded by an extracellular glycoprotein layer (zona pellucida) that separates it from a peripheral layer of follicular cells permeated by one or more fluid-filled antra) |
|
|
Fertilization
a. Usual location b. What layers must the sperm pass through, and how c. When is it called a zygote |
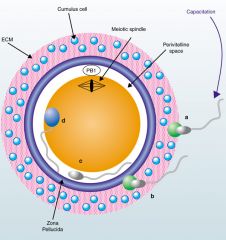
a. Ampulla of the uterine tubes.
(92%) (Cornual 2.5%, Isthmic 0.4%, ovarian 0.4%, cervical 0.1%) b. I. Corona radiata - hyaluronidase (Cell layer) II. Zona pellucida - acrosin, neuraminidase (Glycoprotein) (Zonal reaction - the zona pellucida undergoes a structural change known as the zonal reaction after sperm penetration. On sperm contact with the egg plasma membrane, cortical granules break down and substances are liberated into the perivitelline space that rapidly modify the zona pellucida resulting in a block to further sperm penetration.) (Vitelline membrane - the membrane enveloping the yolk, specifically the thickened cell membrane of large-yoked ova (Vitellus - yolk)) c. When the membranes of the male and female primonuclei disappear after fusion. |
|
|
Embryo
a. Blastomere b. Why do the cells get smaller with subsequent divisions, what is the resulting primary intercellular interactions called c. Morula |
a. One of the cells into which the egg divides after its fertilization. (syn: cleavage cell\embryonic cell)
b. Due to the presence of zona pellucida, compactization. c. 12-15 blastomeres. (Mulberry shape) (Stedman, LF3 ppt) |
|
|
Blastocyst\Blastula
a. What b. What gives rise to the embryonic part of the placenta |
a. The blastula stage of mammalian embryos, consist of the inner cell mass - embryoblast, and a thin trophoblast layer enclosing the blastocele.
(Blastocele (cele - cavity) - the cavity in the blastula of a developing embryo) b. The trophoblast. |
|
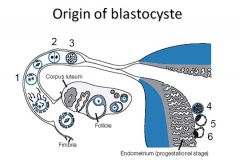
Time
|
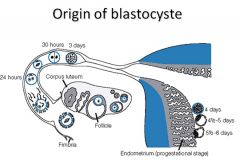
3. Morula
5. Blastocyst |
|
|
Nidation
a. Nidation b. When does the zona pellucida degenerate c. What happens on day 6 d. Where is the most common site of nidation |
a. Embedding of the early embryo in the uterine endometrium.
(Nidus - nest) b. 4-6D c. The blastocyst attach by the embryonal pole to the endometrium. d. The upper posterior part of uterus (Stedman, LF3 ppt) |
|
|
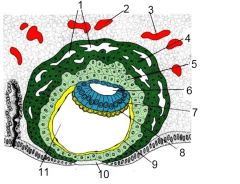
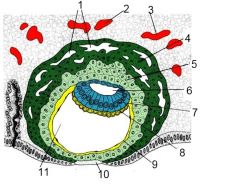
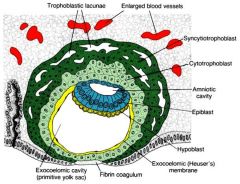
Nidation period
a. What happens with the trophoblast on day 6\the time of nidation b. What happens with the embryoblast on day 8 |
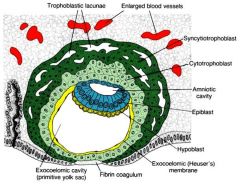
a. The trophoblast split into two layers
I. Cytotrophoblast - inner cell layer, distinguishable cells II. Syncytiotrophoblast - external layer, syncytium, <- cytotrophoblast (Produce enzymes which erode the endometrium -> embryo dwells deeper and gain nutrition from degraded tissue) b. 1. It splits into two layers - bilaminar blastoderm I. Epiblast Tall cells, embryonal pole, -> endo-, ecto- and mesoderm II. Hypoblast short cells, blastocele pole, adjacent to the yolk sac cavity 2. Amniotic cavity appears between epiblast cells (some cells of the epiblast change into amnioblasts that surround the cavity) (Stedman, LF3 ppt) |
|
|
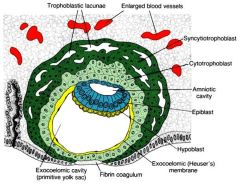
(Exocoelomic\Heuser's membrane - a layer of cells delaminated from the inner surface of the blastocystic cytotrophoblast, envelope the primary yolk sac during second week of embryonic life)
(Exocelom (exo- exterior, celom - cavity)\Extraembryonic celom - that portion of the celom that extends beyond the confines of the embryonic body) (Primary yolk sac/primitive yolk sac\exocelomic cavity: it is the vesicle constituted in the second week, its floor is represented by the Heuser membrane and its ceiling by the hypoblast. It is also known as the exocoelomic cavity) |
|
|
Yolk sac
a. Exocelom\primary yolk sac, when does it arise, from what b. What is extraembryonic mesoderm, how does it arise |
a. 9D
Cells of hypoblast separate and give rise to the exocelomic Heuser membrane. The floor is made from the exocelomic Heuser membrane and the roof is made by the hypoblast cells. b. Soft tissue that invaginate between the amnion, yolk sac, and the cytotrophoblast. <- Cells of the yolk sac. (Stedman, LF3 ppt) |
|
|
Implantation
a. What happens during the 9-10th day b. When is the defect in uterine mucosa overgrown by new epithelium (simple columnar) c. How can these processes cause miscalculation of the delivery term |
a. The embryo is fully implanted in the endometrium and the defect of the uterine mucosa is covered by a fibrin clot.
b. 12D c. Syncytiotrophoblast can cause gentle bleeding as they invade the endometrium -> mistaken for menstruation since it is around the same time. |
|
|
Human chorionic gonadotropin
a. Which structure produce it b. How long does it maintain the activity of the corpus luteum c. How early is the levels high enough to be detected in the urine by a pregnancy test |
a. Synctiotrophoblast
b. Up to the 6th month c. Cca 14 day (Production starts early after nidation) (Pregnancy test work on immunological basis of its beta subunit detection) (Marker of tumor originating from trophoblast in case of extragravidity) |
|
|
Yolk sac
a. Exocelom\primary yolk sac, when does it arise, from what b. What is extraembryonic mesoderm, how does it arise |
a. 9D
Cells of hypoblast separate and give rise to the exocelomic Heuser membrane. The floor is made from the exocelomic Heuser membrane and the roof is made by the hypoblast cells. b. Soft tissue that invaginate between the amnion, yolk sac, and the cytotrophoblast. <- Cells of the yolk sac. (Stedman, LF3 ppt) |
|
|
Implantation
a. What happens during the 9-10th day b. When is the defect in uterine mucosa overgrown by new epithelium (simple columnar) c. How can these processes cause miscalculation of the delivery term |
a. The embryo is fully implanted in the endometrium and the defect of the uterine mucosa is covered by a fibrin clot.
b. 12D c. Syncytiotrophoblast can cause gentle bleeding as they invade the endometrium -> mistaken for menstruation since it is around the same time. |
|
|
Human chorionic gonadotropin
a. Which structure produce it b. How long does it maintain the activity of the corpus luteum c. How early is the levels high enough to be detected in the urine by a pregnancy test |
a. Synctiotrophoblast
b. Up to the 6th month c. Cca 14 day (Production starts early after nidation) (Pregnancy test work on immunological basis of its beta subunit detection) (Marker of tumor originating from trophoblast in case of extragravidity) |
|
|
(Exocoelomic\Heuser's membrane - a layer of cells delaminated from the inner surface of the blastocystic cytotrophoblast, envelope the primary yolk sac during second week of embryonic life)
(Exocelom (exo- exterior, celom - cavity)\Extraembryonic celom - that portion of the celom that extends beyond the confines of the embryonic body) (Primary yolk sac/primitive yolk sac\exocelomic cavity: it is the vesicle constituted in the second week, its floor is represented by the Heuser membrane and its ceiling by the hypoblast. It is also known as the exocoelomic cavity) |
|
|
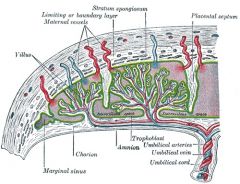
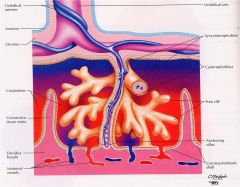
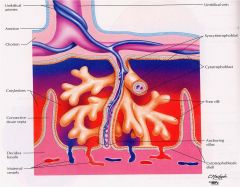
Decidua
a. Decidua b. Decidua basalis c. Decidua capsularis d. Decidua parietalis |
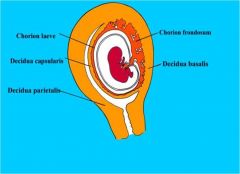
a. Decidua\Deciduous ('falling off') membrane
The mucous membrane of the pregnant uterus that has already undergone certain changes under the influence of the ovulation cycle to fit it for the implantation and nutrition of the zygote. (So called because the membrane is cast off after labor) b. Decidua basalis Between the conceptus and myometrium. c. Decidua capsularis Covers the conceptus (In the fourth month it is squeezed against the decidua parietalis and thereafter undergoes rapid regression) (Operculum deciduale) d. Decidua parietalis The rest of the decidua. (The altered mucous membrane lining the main cavity of the pregnant uterus other than at the site of attachment of the chorionic vesicle) |
|
|
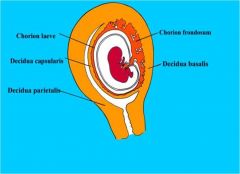
(Chorion\Chorionic vesicle - an extraembryonic fetal membrane, composed of trophoblast lined with mesoderm; it develops villi, becomes vascularized, and forms the fetal part of the placenta)
(Decidua basalis - the area of endometrium between the implanted chorionic vesicle and the myometrium, which develops into the maternal part of the placenta.) (Decidua capsularis - the layer of endometrium overlying the implanted chorionic vesicle; it becomes progressively attenuated as the chorionic vesicle enlarges and, by the fourth month, is squeezed against the decidua parietalis and thereafter undergoes rapid regression.) (Decidua parietalis - the altered mucous membrane lining the main cavity of the pregnant uterus other than at the site of attachment of the chorionic vesicle.) (Chorion laeve\smooth - the portion of the chorion from which the villi disappear in the later stages of pregnancy) (Chorion frondosum\shaggy - the part of the chorion where the villi persists, forming the fetal part of the placenta) |
|
|
Chorion
a. Chorion\Chorionic vesicle b. Chorion laeve\smooth c. Chorion frondosum\shaggy |
a. Chorion\Chorionic vesicle
The outermost of the fetal membranes, composed of trophoblast lined with mesoderm; it develops villi, becomes vascularized by allantoic (yolk sac) vessels, and forms the fetal part of the placenta. b. Chorion laeve\smooth The portion of the chorion from which the villi disappear in the later stages of pregnancy, next to decidua capsularis c. Chorion frondosum\shaggy The part of the chorion where the villi persists. Form the fetal part of the placenta. Next to decidua basalis. |
|
|
Decidual reaction\Reactio decidualis - where, what, under influence of
|
In margo syncytiodecidualis.
-> 1. Change of stromal cells (fibroblasts) -> decidual cells with higher energy content (glycogen, lipid) (Shape: fusiform -> polyhedric) 2. Change of blood supply -> edema 3. Dental arrangement of glands in stratum spongiosum Under influence of progesterone. (Change of stratum functionale) (LF3 ppt) |
|
|
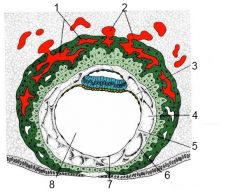
Uteroplacental circulation
a. Origin of the maternal sinusoids b. Origin of the trophoblastic lacunes, when c. Which maternal arteries and veins are involved in the trophoblastic lacunes d. Further development of the lacunae |
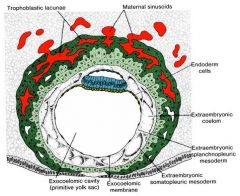
a. Enlargement of endometrial capillaries adjacent to the embryo.
b. The trophoblastic lacunes are formed in the syncytiotrophoblast and the blood comes from sinusoids which have become digested by the syncytiotrophoblast. Around the 9th day. c. Spiral arteries and endometrial veins. d. Lacunae -> lacunar network -> intervillous space |
|
|
|
|
|
Extraembryonic mesoderm
a. How does the extraembryonic celom originate b. Connecting stalk c. What happens to the yolk sac d. What happens to the extraembryonic mesoderm as the extraembryonic celom forms |

a. Cavities in the extraembryonic mesoderm enlarge and fuse.
b. Connecting\body stalk The extraembryonic precursor of the umbilical cord by which the embryo is attached to its trophoblastic chorion. (The embryo 'hangs' from this structrue in the extraembryonic celom) c. Part of it is turned into an exocelomic cyst and then disappear in the celomic wall. The rest of it remains as the secondary yolk sac. d. It remains as the I. somatic mesoderm - on the surface of the extraembryonal celom and amniotic cavity II. Splanchnic mesoderm - on the surface of the secondary yolk sac (Extraembryonal celom = chorionic cavity) (Both part of the trophoblast and the extraembryonal somatic mesoderm create the wall of the chorionic cavity) |
|

|

Extraembryonal celom = chorionic cavity
|
|
|
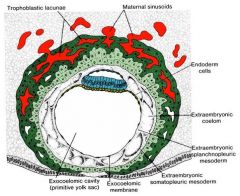
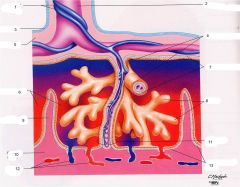
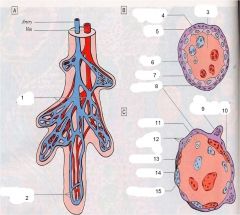
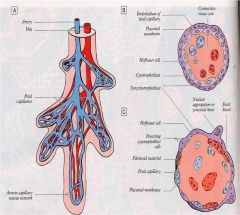
Villus
a. Primary villus, when, <-, components b. Secondary villus, components c. Tertiary villus, components |
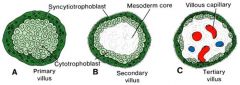
a. Primary villus
13-14th day <- Induction by extraembryonal somatic mesoderm. Invasion of cytotrophoblast into the syncytiotrophoblast -> components 1. Syncytiotrophoblast 2. Cytotrophoblast b. Trophoblast and extraembryonic mesoderm. c. Trophoblast (only cytotrophoblastic islets), extraembryonic mesoderm, and vessels. |
|
|
Allantois ('sausage')
a. What b. The 3 stages and its parts c. Later the opening moves into d. When does hematopoiesis occur here e. What is the fate of the intraembryonal part |
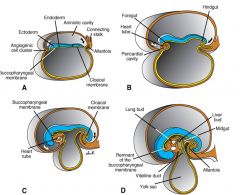
a. Diverticulum from the posterior wall of the yolk sac.
b. 1. Gemma ('bud') alloenterica 2. Canalisatio I. Pars proximalis -> murus ventralis mesenteri (wall of ventral mesenery) I. Pars distalis -> diverticulum allantoicum 3. Pedunculus allantoicus I. Diverticulum allantoicum II. Mesenchyma allantoica (hematopoiesis) III. Vasa allantoica -> vasa umbilica (For fetal nutrition from placenta) c. Cloaca (In early embryos, the endodermally lined part into which the hindgut and allantois empty into) d. 3-5T (d?) e. Intraembryonal part -> urachus (-> ligamentum umbilicale medianum\median umbilical ligament), pars vesicalis sinus urogenitalis\vesical part of urogenital sinus -> urinary bladder |
|
|
Yolk sac
a. Meckel diverticulum b. Two important functions |
Transitory yolk sac structure. Extinction during body wall closure.
Part is used for gut development. (Stedman: the remains of the yolk stalk of the embryo, which, when, persisting abnormally as a blind sac in he adult is located on the ileum a short distance above the cecum, it may be attached to the umbilicus and, if the lining includes gastric mucosa, peptic ulceration and bleeding may result) b. Gametes, first hematopoietic site |
|
|
Umbilical cord\Funiculus umbilicalis\Chorda umbilicalis
a. Yolk stalk\Umbilical duct\Vitelline duct\Omphaloenteric duct b. When is the period of physiological herniation\ansa umbilicalis intestini (ansa - any anatomical structure that form an arc or loop) c. Which structures obliterates and thus differentiates the primitive from the definite umbilical cord d. Length and diameter of the umbilical cord at birth |

a. Connection between extra- and intraembryonic cavity.
(The connection disappears at the end of the 3rd month.) b. 6-10th week c. Allantois, vitelline vessels, and yolk sac with the omphaloenteric duct -> Definite umbilical cord: umbilical vessels, warthon's jelly d. 50 cm x 2 x cm |
|
|
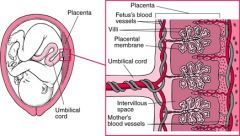
Placenta - components
|
Embryonic origin - chorion frondosum
Maternal origin - decidua basalis (Stedman) |
|
|
Chorionic plate
|
The part of the fetal placenta that gives rise to chorionic villi, which attach to the uterus during the early stage of formation of the placenta.
(Chorionic villi - vascular processes of the chorion of the embryo that enter into the formation of the placenta) (Mosby's medical dictionary) |
|
|
Chorionic villi
|
Vascular processes of the chorion of the embryo that enter into the formation of the placenta.
|
|
|
Developemnt of the fetal membranes - what, when (3)
|

1. Fetal growth within amniotic sac -> obliteration of the chorionic cavity in the 8th week -> Amniochorion
(Lined by amniotic epithelium internally and chorionic villi externally) 2. New growth phase -> obliteration of the uterine cavity -> fusion of decidua capsularis and parietalis at the end of the 2nd trimester 3. Amniochorion fuse with the decidua parietalis |
|
|
Cytotrophoblastic shell
|
The external layer of fetally derived trophoblastic cells on the maternal surface of the placenta.
(Stedman) |
|
|
Villus
a. Parts of centrum villi b. Parts of cortex villi c. Parts of superficies villi |
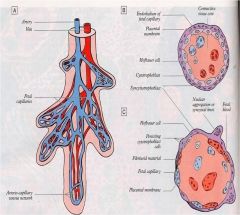
Villus
a. Centrum villi I. Fibroblasts II. Myofibroblasts III. Hofbauer macrophages IV. Rete arteriocapillarovenularum (Rete - network) (Endothelium continuum) b. Cortex villi I. Vestigium cytotrophoblasti Langhansi (Vestigium - trace\rudimentary structure\ the degenerated remains of any structure which occurs as an entity in the embryo\fetus) II. Nodi syncytiales c. Superficies villi I. Syncytiotrophoblast II. Gemma ('bud') syncytiales (Formation site?) III. Substantia fibrinoidea perivillosa\intravillosa Rohri\Rohr stria (In areas without syncytiotrophoblast cover) (Layer of fibrinoid in the intervillous spaces of the placenta) |
|
|
Intervillous space
|
The space of the placenta into which the chorionic villi project and through which the maternal blood circulates.
Lined with syncytiotrophoblasts. |
|
|
Intervillous space
What Lined by Derived from |
The space of the placenta into which the chorionic villi project and through which the maternal blood circulates (from aa spirales).
Lined with syncytiotrophoblasts. From lacunae. |
|
|
Placental membrane\Barrier (claustrum)
a. What b. Components (5) |
a. The semipermeable layer of fetal tissue separating the maternal from the fetal blood in the placenta.
b. 1. Endothelium of fetal capillaries 2. Subepithelial basal lamina 3. Stroma of the villi 4. Cytotrophoblast 5. Syncytiotrophoblast (Stroma and cytotrophoblast gradually fades) |
|
|
(Anchoring\stem villi - act to stabilize the mechanical integrity of the placental-maternal interface)
(Floating\free villi - found 'floating' in the intervillous space) |
|
|
Fetoplacental circulation
a. Flow b. Pathway |
a. 400 mL\min
b. 1. Aa iliaca internae --> 2. 2 aa umbilicales --> (50-60% o2sat) 3. Capillaries in villi --> 4. 1 v umbilicalis --> (70-80% o2-sat) 5. Ductus venosus --> 6. v. cava inferior |
|
|
Pars basalis placentae propriae - components (6)
|
1. Paries externus syncytialis spatii intervillosi (External wall of syncytial layer of intervillous space)
2. Rohr stria\Stria fibrinoidea externa Rohri (Layer of fibrinoid in the intervillous spaces of the placenta) (Stria - band\stripe) 3. Cytotrophoblast 4. Vestigium testae ('shell') trophoblasticae\Remnant of cytotrophoblastic shell 5. Loose connective tissue\Textus connectivus laxus I. Zona limitans decidualis II. Stria fibrinoidea interna Nitabuchi\Nitabuch membrane (a layer of fibrin between the boundary zone of compact endometrium and the cytotrophoblastic shell in the placenta.) III. A. spiralis uteri 6. Decidua basalis (A cotyledon ('cup-shaped') is the area between the placental septa, a unit of the fetal placenta supplied by the vessels of one stem villus) |
|
|
Placenta praevia
|
Placenta located in the lower uterine segment, so that it partially or completely covers or adjoins the internal os.
(The main risk with a vaginal delivery with a praevia is that as you are trying to bring down the head or a leg, you might separate more of the placenta and increase the bleeding. Placenta praevia increases the risk of puerperal sepsis and postpartum haemorrhage because the lower segment to which the placenta was attached contracts less well post-delivery.) |
|
|
Variations of situs placentae (10)
|
1. Situs dorsalis placentae
2. Situs lateralis placentae 3. Situs ventralis placentae 4. Situs fundalis placentae (Fundus ('bottom'): the bottom or the part farthest removed from the opening or exit of a hollow organ) 5. Sitius cornualis placentae (In cornu of uterus\uterine horn. The portion of the uterus to which the intramural section of the uterine tube enters on either the right or left side) 6. Placenta praevia 7. Placenta preavia centralis 8. Placenta praevia lateralis 9. Placenta praevia marginalis 10. Situs cervicalis placentae |
|
|
Variations of formae placentae\shapes of placenta (8)
|
1. Placenta discoidea
2. Placenta accessoria\succenturiata (accessory) (A mass of placental tissue distinct from the main placenta) 3. Placenta anularis 4. Placenta lobata 5. Placenta bilobata\bipartita 6. Placenta trilobata 7. Placenta membranacea\diffusa (An abnormally thin placenta covering an unusually large area of the uterine lining) 8. Placenta vallata\circumvallata |
|
|
Variations in insertions of the umbilical cord\funiculus umbilicalis
|
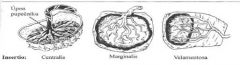
1. Insertio centralis
2. Insertio marginalis 3. Insertio velamentosa (Velamentous - expanded in the form of a sheet\veil) (A form of insertion of the fetal blood vessels into the placenta, in which the vessels separate before reaching the placenta and develop toward it in a fold of amnion, somewhat like ribs of an open parasol -> parasol insertion) |
|
|
Anomalies of the fetal membranes\Anomaliae membranarum fetalium - groups
|
1. Anomaliae amnii et liquoris amniotici
(Adhaesio amnii Hydramnion; Polyhydramnion Oligohydramnion Taenia amniotica) 2. Anomaliae chorii (Deformitas placentae Defectus placentae Defectus paraplacentalis chorii) 3. Anomaliae funiculi umbilicalis (A. umbilicalis singularis Funiculus umbilicalis glomeratus, Strangulatio, Amputatio, Nodus spurius funiculi umbilicalis, Nodus verus funiculi umbilicalis, Vesicula allantoica) 4. Anomaliae placentae (Placenta adhaerens Placenta accreta Placenta increta Placenta percreta Placenta extrachorialis Placenta fenestrata Placenta incarcerata Placenta panduriformis) |
|
|
Clinical outcomes of wrong placentation (3)
|
Clinical outcomes of wrong placentation (3)
1. Misshapes of embryonic growth 2. Preeclampsia (Triad of hypertension, proteinuria and edema. Usually occurs after the 20th week of gestation) 3. Abruptio placentae (Premature detachment of a normally situated placenta) |
|
|
Anomaliae amnii et liquoris amniotici (4) - part of Anomaliae membranarum fetalium\fetal membrane defects
|
1. Adhaesio amnii
2. Polyhydramnion\Hydramnion (<- esophageal atresia, gross developmental defects of the nervous system) 3. Oligohydramnios (<- premature rupture of amniochorion, renal agenesis: hypouresis or anuresis) 4. Taenia amniotica (Amniotic band sequence - activity comprising early rupture of the amnion with formation of bands that adhere to or compress parts of the fetus, resulting in a wide variety of anomalies; craniofacial defects, amputation of a limb, and abdominal evisceration.) |
|
|
Anomaliae chorii (3) - part of anomaliae membranarum fetalium\fetal membrane defects
|
1. Deformitas placentae
2. Defectus placentae 3. Defectus paraplacentalis chorii |
|
|
Anomaliae placentae (8) - part of anomaliae membranarum fetalium\fetal membrane defects
|
1. Placenta adherens
2. Placenta accreta 3. Placenta percreta 4. Placenta increta 5. Placenta extrachorialis 6. Placenta fenestrata 7. Placenta incarcerata ('trapped')\Retained placenta (Incomplete separation of the placenta and its failure to be expelled at the usual time after delivery of the child) 8. Placenta panduriformis |
|
|
Anomaliae funiculi umbilicalis (7) - part of Anomaliae membranarum fetalium
|
1. Arteria umbilicalis singularis
2. Funiculus umbilicalis glomeratus 3. Strangulatio 4. Amputatio 5. Nodus spurius (fake) funiculi umbilicalis\False umbilical cord knot (A knotlike bulge in the umbilical vein causing apparent twisting of the cord) 6. Nodus verus funiculi umbilicalis (knot in the umbilical cord) 7. Vesicula allantoica |
|
|
Functions of the placenta (5)
|
1. Metabolic - synthesize glycogen, cholesterol, and MK (source of nutrition for the embryo)
2. Placental transport 3. Keep blood of mother and fetus from mixing 4. Passive immunity via diffusion of IgG 5. Endocrine function I. hCG II. hPL (human placental lactogen)\human chorionic somatomammotrophic hormone III. hCT IV. hCACTH (human chorionic adrenocorticotropin) V. Progesteron (hormone of pregnancy, <- maternal cholesterol or pregnenolone) and estrogen (estriol) (Harmful substances that can pass through: drugs (alcohol), poisons, CO, viruses (rubella, CMV), toxoplasmosis gondii) |
|
|
Placental villi
a. Villus ancorans (anchoring)\Inserting villus b. Villus ramosus\Branching villus c. Villus liber\Free villus |
a. Villus ancorans (anchoring)\Inserting villus
Attached to decidua basalis b. Villus ramosus\Branching villus Branches in the intervillous space c. Villus liber\Free villus Branches of the branching villus, in the intervillous space |
|
|
Amniotic fluid\Liquor amnioticus
a. Composition b. Produced by c. First urine excretion d. First swallowing |
a. 99% water
b. 1st - amnioblasts 2nd - diffusion through amniochorion from decidua parietalis 3rd - diffusion from maternal blood from spatia intervillosa c. 11w d. end of 3rd trimester (400 mL\day) |
|
|
Amniotic fluid - significance\function (6)
|
Amniotic fluid - significance\function
1. Enable symmetrical growth of the embryo 2. Provide a barrier against infection 3. Involved in lung development 4. Mechanical protection - 'pillow' effect 5. Thermoregulation 6. Enable movement (amniocentesis) |
|
|
Amniocentesis
a. When b. Which conditions can be diagnosed, how |
a. 16-20th week
b. 1. Fetal sex 2. Chromosomal aberrations - Trisomy 21, 13\Patau syndrome, 18\Edwards syndrome. DNA diagnosis of other hereditary diseases 3. AFP I. High -> heavy defects of the neural tube II. Low -> hereditary defects - ie Downs syndrome (In non-embryo\fetus high values indicate hepatocellular carcinoma, germ cell tumors and metastatic cancer in the liver) 3. Spina bifida (Polyhydramnion can be treated) |
|
|
|
|
|
Placental transfer
a. Which substances are transferred by active transport b. Which substances are transferred by pinocytosis c. Hormones that cross the placenta |
a. Sugars, Amino acids, Fatty acids
(No transfer of cholesterol, TG, or phospholipids) b. Gamma-globulins - IgG (Provide passive immunity for diphtheria, smallpox, and measles. Not for chickenpox or pertussis) c. 1. Thyroxine and T3 2. Testosterone 3. Synthetic progestins |
|
|
Placental transfer - which pathogens can be transferred (8)
|
Only viral
1. CMV 2. Rubella 3. Coxsackie 4. Varicella 5. Polio 6. Syphilis 7. Spirochete (genus of motile bacteria) 8. Toxoplasmosis gondii (protozoa) |
|
|
Adult vestigial structures
a. Umbilical vein b. Ductus venosus c. Ductus arteriosus |
a. Umbilical vein -> ligamentum teres (free edge of the falciform ligament)
b. Ductus venosus -> ligamentum venosum (stretch from the left branch of the portal vein to the inf. vena cava) c. Ductus arteriosus -> ligamentum arteriosus (left pulmonary artery to the under surface of the aortic arch) |
|
|
Yolk sac
a. Synonym (2) b. The two developmental types c. What remains |
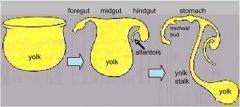
a.
1. Vesicula umbilicalis 2. Saccus vitellinus b. 1. Vesicula umbilicalis primaria\Primary yolk sac\Cavity of blastocyst\Exocelom (Blastocystis trilaminaris?) 2. Vesicula umbilicalis secundaria\Saccus chorionicus immaturus c. Part is used for gut development, part may reside as diverticulum ilei Meckeli (2%) |
|
|
Yolk sac\Saccus vitellinus\Vesicula umbilicalis
a. Parts of secondary yolk sac\Vesicula umbilicalis secundaria\saccus chorionicus immaturus b. Function of the yolk sac (4) |
a.
1. Cavitas vesicula umbilicalis secundaria 2. Pedunculus vesicula umbilicalis I. Vasa omphaloenterica\vitellina II. Ductus omphaloentericus\Yolk stalk (Omphalo- umbilicus\navel) b. 1. 13th day - Gonocytes\Cellulae germinales precursoriae, in endoderma extraembryonicum vesicae umbilicalis 2. 2-3 weeks - selective transport of fluid and nutrition to the fetus 3. 3-6th week - Hematopoiesis (first hematopoiesis) in mesenchyma extraembryonicum vesicae umbilicalis 4. Venae omphaloenterica\vitelline -> part of liver bed and portal vein |
|
|
Endometrium
a. Type of epithelium b. Name and type of glands c. Which cells become the decidual cells d. Name the two layers |
a. Simple columnar
b. Glandulalae uterales, tubular c. Stroma cells d. I. Stratum basale - rich on cells, more reticular fibers, blood vessels II. Stratum functionale - segregates during menstruation, -> stratum spongiosum, stratum compactum |
|
|
Stratum functionale
a. Stratum functionale b. Stratum spongiosum c. Stratum compactum |
a. The endometrium except for the stratum basale
(formerly believed to be lost during menstruation but now considered to be only partially disrupted.) (-> decidua) b. the middle layer of the endometrium formed chiefly of dilated glandular structures. c.The superficial layer of decidual tissue in the pregnant uterus, in which the interglandular tissue preponderates. |
|
|
Decidua basalis - parts (5)
|
1. Cryptae endometrii
2. Glandulae endometrii 3. Septa placenta, Insulae cellularum placentae (mixed origin mother and fetus) 4. Zona limitans decidualis (Stratum compactum-cytotrophoblastic shell) 5. Substantia fibrinoidea (At the end of gravidity, mark of degradation) |
|
|
Lamina chorionica of mature placenta - components (5)
|
1. Mesothelium amnioticum
(Simple cuboidal epithelium) 2. Remnant after vesicula umbilicalis in placental insertion of umbilicus 3. Vasa umbilicalia 4. Cytotrophoblastus langhansi 5. Substantia fibrinoidea Langhansi |
|
|
Cotyledon
a. Number of cotyledo maternalis and cotyledo fetalis b. Characteristics of the fetal cotyledon (4) |
a. Cotyledo maternalis\Physician's cotyledon - 30
cotyledo fetalis\embryologists cotyledon - 40-60 b. Fetal cotyledon ('cup-shaped hollow') 1. One root villus (villus peduncularis major\truncus chorii) and one spiral artery 2. Has several villi (villus peduncularis) with artery or arteriole and vein or venule 3. Has more middle villli\villi intermedii 4. Has lots of villi terminales (With loops of capillaries) (Fetal cotyledon - a unit of the fetal placenta supplied by the vessels of a stem villus. Several such cotyledons may occur between two placental septa (a maternal cotyledon)) |

