![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
186 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What are the ancient origins of therapeutic exercise? ***
|
- India, circa 800 BC (Atharva-Veda recommended exercise and massage for chronic rheumatism
- Greece, circa 480 BC (Herodicus and his student Hippocrates wrote of benefits of exercise to include muscle strengthening, improved mental attitude, and decreased obesity) |
|
|
|
What are the modern origins of therapeutic exercise? ***
|
- Sweden in the 19th century with Pehr Henri Ling (a fencing instructor) who believed precise movements, scientifically applied, could remedy disease and dysfunction of the body
- Switzerland, in 1902 when Frenkel published an exercise program for ataxia; his main contribution was insistence on repetition - Delorme in 1945 developed progressive resistance exercises (PRE) which is considered one of the most important advances in therapeutic exercise - Kabat took therapeutic exercise out of the cardinal plane by introducing diagonal movement; Knott and Voss furthered his work by publishing "Proprioceptive Neuromuscular Facilitation" in 1956 |
|
|
|
Who is the Father of Therapeutic Exercise?
|
Herodicus
|
|
|
|
According to the "Guide to Physical Therapist Practice," what is the most important procedural intervention?
|
therapeutic exercise
|
|
|
|
Macrotrauma
|
a single injurious force in which the pain and tissue destruction occur simultaneously
|
|
|
|
Microtrauma
|
a series of small injurious forces, many/most/all of which precede the patient's perception of pain
|
|
|
|
Is pain always an accurate indicator of tissue health?
|
No, since the chemical mediators which relay pain may dissipate long before the tissue is healthy enough to respond to the forces such as those that led to the initial injury.
|
|
|
|
Describe Phase I of tissue healing. ***
|
- inflammatory response
- lasts 24-48 hours, up to 7-10 days - vasoconstriction (clot), then vasodilation (bring in WBC, etc.) - edema, pain, redness, increased temperature, loss of function |
|
|
|
Describe Phase II of tissue healing. ***
|
- repair/proliferation phase
- 48 hours to 6 weeks after injury - tissue regeneration, vascularization, cell growth - initially lays down Type III collagen, which is weak and thin, but exists as a foundation for further replacement with Type I collagen - revascularization - epithelialization - new skin/mucous/serous membranes |
|
|
|
Describe Phase III of tissue healing. ***
|
- connective tissue formation/remodeling phase
- 3 weeks to 12 months after injury - Type III collagen converted to Type I for better cross-lineage and tensile strength - balance of tissue deposition, modification and degradation - collagen and connective tissue reorient along lines of physical stress - scar remodeling |
|
|
|
Different tissues have _____ rates of healing, but all must receive _____ to heal. Therefore the strongest determinant of tissue healing rate is ______ ______.
|
- different
- nutrients - blood supply |
|
|
|
Definition of therapeutic exercise ***
|
the systematic performance or execution of planned physical movements, postures, or activities intended to enable the patient/client to:
1) remediate or prevent impairments 2) enhance function 3) reduce risk 4) optimize overall health 5) enhance fitness and well being (A secondary definition by Licht states that therapeutic exercise is "motions of the body or its parts to relieve symptoms or to improve function.") |
|
|
|
List the eight types/goals of therapeutic exercise given in lecture. ***
(NOTE: These got a "foot stomp"!!) |
- aerobic capacity/endurance conditioning
- balance, coordination, agility - body mechanics/postural stabilization - flexibility exercises - gait and locomotion training - neuromotor development training - relaxation - strength, power, endurance training (The above were given in lecture as both types of therapeutic exercise and goals of therapeutic exercise. However, the book lists the following as the expected goals and outcomes:) - impact on pathology/pathophysiology - impact on impairment - impact on functional limitations - impact on disabilities - risk reduction/prevention |
- strength, power, endurance training
- aerobic capacity/endurance conditioning - flexibility exercises - agility, balance, coordination - body mechanics/postural stabilization - gait and locomotion training - neuromotor development training - relaxation |
|
|
Describe a joint capsule
|
- exists in all synovial joints
- two layers (stratum fibrosum/fibrous capsule and stratum synovium) |
|
|
|
Describe the stratum fibrosum/fibrous capsule
|
- contributes to joint stability
- large percentage of type I collagen oriented in several directions to combat multidirectional tensile loads - connects to periosteum - poorly vascularized - highly innervated |
|
|
|
Describe the stratum synovium
|
- internal layer of the capsule
- highly vascularized - poorly innervated - specialized cells manufacture synovial fluid for lubrication and nutrition |
|
|
|
Repetitive motion promotes:
|
synovial bathing and easier/less painful motion
|
|
|
|
Ligaments most commonly function as
|
passive connectors and stabilizers between bones
|
|
|
|
What is the healing time for ligaments?
|
between 6-8 weeks, up to 12-14 weeks
|
|
|
|
What can help strengthen the repair of ligamentous tissue?
|
controlled application of stress during the healing process
|
|
|
|
How are tendons attached to bones?
|
via Sharpey's fibers (mineralized fibrocartilage)
|
|
|
|
Describe the blood supply available for healing tendons
|
- blood supply is greatest at the musculotendinous zone
- poorer blood supply in the rest of the tendon |
|
|
|
Most macrotrauma injuries that occur below the musculotendinous junction require ______ ______ for healing
|
surgical intervention
|
|
|
|
What is important to remember about pain with tendon injuries?
|
- tissue injury is present long before the patient identifies the start of pain
- pain will subside prior to the conclusion of healing, leaving patient at risk of repeat injury, pain, inflammation if (s)he returns to full activity too soon |
|
|
|
What are the three types of cartilage?
|
- elastic (ear, epiglottis)
- fibrocartilage (intervertebral discs, menisci) - hyaline (ends of long bones in synovial joints) |
|
|
|
Function of hyaline cartilage
|
- disperse compressive and shearing forces
- provide low coefficient of friction (5-20X more slippery than ice!) |
|
|
|
Nourishment of hyaline cartilage
|
- avascular and aneural
- nourished by synovial fluid and diffusion of nutrients from subchondral bone - via "milking" action through intermittent compression of joint surface |
|
|
|
Grade 1 muscle strain
|
- adverse stretching of fibers
- minimal tear - no palpable defect - minor loss of function |
|
|
|
Grade 2 muscle strain
|
- up to half the muscle fibers are torn
- painful dysfunction - limited ROM and activity |
|
|
|
Grade 3 muscle strain
|
- rupture of all of the muscle fibers
- major disability - often palpable defect |
|
|
|
The inability of a joint to move through a full ROM due to loss of elastic extensibility of the connective tissue components is known as:
|
passive insufficiency
(ex. women who only wear heels shorten their gastrocs and Achilles) |
|
|
|
What could decreased ROM, reduced strength, or increased pain despite the stage of healing indicate? What should the response be?
|
possibly the intervention on one soft tissue exacerbating the symptoms of another, since rarely is only one soft tissue affected
response should be to decrease the load and/or increase amount of rest (work with the PT on POC) |
|
|
|
Use of physical agents or electrotherapeutic modalities in the absence of other interventions is not considered:
|
physical therapy
(unless documentation justifies necessity of exclusive use) |
|
|
|
Definition of range of motion (ROM) ***
|
the extent of osteokinematic motion available for movement activities, functional or otherwise, with or without assistance.
(This is NOT "stretching," we are maintaining, NOT increasing ROM.) |
|
|
|
Osteokinematic motion ***
|
movement of whole bone
|
|
|
|
Arthrokinematic motion
|
motion at articular surfaces within joint capsule
(involuntary—not our focus) |
|
|
|
AROM
AAROM PROM *** |
AROM - solely voluntary
AAROM- partly voluntary with some assistance (by person or equipment) PROM- solely without voluntary contraction |
|
|
|
Describe the therapeutic planes ***
|
- sagittal – medial-lateral axis
- frontal (coronal) – anterior-posterior axis - transverse (axial/horizontal) – vertical/longitudinal axis (Ensure you address each of the planes via therapeutic exercise.) |
|
|
|
What physical and/or physiological factors affect ROM? ***
|
- joint shape, congruency
- soft tissue pliability - pathologies, injuries |
|
|
|
What are the effects of immobilization? ***
|
While immobilization is usually necessary in the initial stages of healing, prolonged immobilization can result in:
- bone density loss - cartilage degeneration - fibrosis and adhesion of connective tissue - atrophy & contracture |
|
|
|
What are the benefits of ROM exercises? ***
|
- maintain current joint movement
- maintain soft tissue extensibility - assist in circulation & nutrition - inhibit pain via stimulation of mechanoreceptors (gating) - prevent clot formation - slow atrophy - psychological outlook may improve |
|
|
|
What is CPM? ***
|
- continuous passive motion
- a form of passive motion delivered via a motorized device - used for extremities, esp. LE. (commonly post knee surgery) |
|
|
|
What is stress deprivation and what tissues are primarily affected? ***
|
- changes that occur at a cellular level in soft-tissue when a limb is immobilized
- synovial joints - other soft-tissue stiffness/adhesions |
|
|
|
What are the beneficial physiological effects of CPM? ***
|
- stresses the tissue (in a good way)
- lubricates, by increasing synovial fluid and vascular circulation - improves nutrition - increases metabolism - facilitates waste removal - increases extensibility/motion |
|
|
|
What are some treatment goals for CPM? ***
|
- healing of avascular articular tissue
- decreasing adhesions of tendons and ligaments - decreasing pain (gating) - decreasing edema (pumping) - increasing ROM |
|
|
|
What are some of the parameters for application of CPM? ***
|
- use is most beneficial during the first 3 weeks after injury or surgery
- device is often applied in recovery room - typical use is 8 hrs. (minimum) and 24 hrs. (maximum) |
|
|
|
What are some contraindications and precautions for use of CPM? ***
|
- increasing motion beyond protected ranges (adhere to instructions of M.D.)
- increase in symptoms of bleeding, pain, or edema |
|
|
|
What is MMT? ***
|
- manual muscle testing
- a method by which muscle strength is defined and measured - an attempt to determine patient's ability to voluntarily contract muscle or muscle group |
|
|
|
What is gross MMT? ***
|
assessment of strength of a limb
|
|
|
|
What is specific MMT? ***
|
differentiates individual muscles where possible
|
|
|
|
What is the purpose of MMT? ***
|
- shows patient’s functional capability
- helps develop POC - shows progress and effectiveness of treatment - demonstrates need for supportive apparatus (e.g., splint, ambulation aid) - assists in diagnosis - justifies payment, documentation |
|
|
|
Two types of resistance testing ***
|
- break test
- active resistance test |
|
|
|
What is a break test? ***
|
resistance given at end of test range
- therapist tries to break the patient’s hold |
|
|
|
What is an active resistance test? ***
|
- resistance applied throughout test range
|
|
|
|
What are the six grades (number, letter, and word) for manual muscle testing? ***
|
5 - normal (N)
4 - good (G) 3 - fair (F) 2 - poor (P) 1 - trace (T) 0 - zero (0) |
|
|
|
Qualify a "normal" (5/N) grade in manual muscle testing ***
|
patient completes full ROM against gravity; holds against maximal resistance
|
|
|
|
Qualify a "good" (4/G) grade in manual muscle testing ***
|
patient completes full ROM against gravity, holds against strong resistance, but yields against maximum resistance
|
|
|
|
Qualify a "fair" (3/F) grade in MMT ***
|
patient completes full ROM against gravity with no manual resistance
(This is the starting point--test a 3, then try 4/5, because you obviously don't want to start with moderate or maximum resistance on someone who cannot even perform the full movement in the first place.) |
|
|
|
Qualify a "poor" (2/P) grade in MMT ***
|
patient either:
- completes full ROM with gravity minimized (e.g., elbow supported on a table—partial would be a 2-/P-), - or completes partial ROM against gravity (gravity minimized is the more correct/better way of testing this level) |
|
|
|
Qualify a "trace" (1/T) grade in MMT ***
|
some visual or palpable contractile activity, but no joint motion
|
|
|
|
Qualify a "zero" (0/Z) grade in MMT ***
|
no palpable contractile activity
|
|
|
|
Qualify an F+ in MMT ***
|
patient can hold the end position against mild resistance
|
|
|
|
Qualify a P+ in MMT ***
|
e.g., plantar flexion – partial heel rise in standing position, or full ROM against max resistance NWB
|
|
|
|
Qualify a P- in MMT ***
|
patient can complete partial ROM in gravity minimized position
|
|
|
|
Are the "+" and "-" typically used in MMT grading? ***
|
Daniels and Worthingham discourage use, but they are readily used in the clinical setting
(thus we will use them too) |
|
|
|
Quantify the Kendall and McCreary test measurements for MMT ***
|
100% - N
80% - G 50% - F 20% - P 5% - T 0% - Z |
|
|
|
What considerations must be made when applying resistance during MMT? ***
|
you need to be able to adjust based on the patient's:
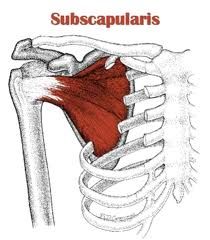
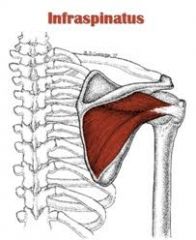
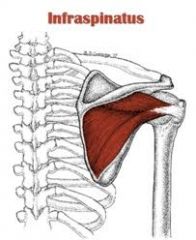
- age - gender - muscle group being tested [e.g., less force (about 2-3 fingers) used for resistance on external shoulder rotation because only the small infraspinatus and teres minor are prime movers; more force/whole hand for internal shoulder rotation because larger latissumus dorsi, pectoralis major, subscapularis, and teres major are prime movers] |
|
|
|
How is it recorded if the patient lacks full ROM? ***
|
e.g., -20/G
(ask for clarification/explanation on this!!) |
|
|
|
The therapist performing MMT must be sure to compare...
*** |
both sides of the body
|
|
|
|
What is important to remember about your hands when performing MMT? ***
|
BOTH hands are doing something at all times!!
provide stabilization to the proximal segment while adding resistance to distal segment (for skills check this also got a foot stomp!!) |
|
|
|
While providing support to the proximal segment, the therapist is also watching for/trying to prevent...
|
substitutions by other muscles
[e.g., on shoulder external rotation for a patient with grade 2 or less (patient lying prone with arm dangling for g.m.) second hand is palpating the infraspinatus/teres minor to ensure there is shoulder movement/rotation and the patient is not simply supinating the forearm) |
|
|
|
The book's definition of ROM
|
the extent of osteokinematic motion available for movement activities, functional or otherwise, with or without assistance
|
|
|
|
How is gravity's affect on ROM controlled?
|
through positioning of the body segment during the movement
|
|
|
|
The amount of ROM available at a synovial joint depends on what two broad categories of factors?
|
- intrinsic
- extrinsic |
|
|
|
What intrinsic factors affect ROM?
|
- anatomic composition of the joint
- shape and congruency of the articulating bony surfaces - pliability of the joint capsule, ligaments, and other collagenous tissues - strength and flexibility of musculature acting on or crossing the joint (one or more of these factors create anatomic limits to joint ROM) |
|
|
|
What extrinsic factors affect ROM?
|
- age (causes decreased pliability in contractile and noncontractile tissues, thus reduced ROM)
- body segment size (related to muscle or adipose tissue bulk) - effects of disease, injury, overuse, and/or immobilization |
|
|
|
Upon what does hyaline cartilage nutrition depend?
|
on the compression and decompression that accompanies joint movement
|
|
|
|
Often, disease and traumatic injuries alter the _______ of the joint and this leads to....
|
biomechanics
malalignment, abnormal motion, and joint tissue degeneration |
|
|
|
What are some adverse effects of immobilization and joint disuse?
|
- regional osteoporosis
- cartilage dehydration and degeneration - collagenous tissue fibrosis and adhesion - muscle tissue contracture and atrophy |
|
|
|
What conditions can arise due to extended periods of immobilization?
|
- paralysis
- muscle spasticity - various forms of arthritis - pain |
|
|
|
How quickly can diminished bone density and reduced bone strength secondary to immobilization appear?
|
within just a few weeks of immobilization
|
|
|
|
Articular cartilage, due to its avascular state, can undergo irreversible degeneration with immobility of how long?
|
even short periods (i.e., days)
|
|
|
|
Why do collagenous tissues (ligaments, joint capsules, fascia, and tendons) experience tightening and stiffening during immobilization?
|
primarily due to the formation of excessive collagen fiber crosslinks that reduce joint motion and mechanical strength of connective tissue
|
|
|
|
What changes in muscle tissue are seen with immobilization? How rapidly can this occur?
|
reduction in muscle tissue size and contractile force (both strength and endurance)
after just a few days of immobilization |
|
|
|
Which muscle tissues atrophy more quickly, fast-twitch or slow-twitch?
|
slow-twitch
|
|
|
|
The amount of muscle tissue contracture (adaptive shortening) is dependent on...
|
the positioning during immobilization (different effects on the sarcomere length and number depending on whether the muscle is immobilized in a shortened or lengthened position)
|
|
|
|
Book definition of ROM exercise
|
AROM, AAROM, or PROM performed repetitively for the general purpose of maintaining current joint movement and preventing decreased pliability of tissue
|
|
|
|
According to the "Guide to Physical Therapist Practice," how are
- AROM and AAROM categorized? - PROM? |
- as therapeutic exercise
- as manual therapy (a passive intervention) |
|
|
|
Indications for ROM exercise
|
- postsurgical musculoskeletal conditions
- pathologic conditions (spasm, strain, inflammation, contusion) - joint sprain, inflammation, degeneration and contracture |
|
|
|
What is the primary precaution for performing ROM exercises?
|
acute injury
|
|
|
|
ROM exercise in the acute phase of rehabilitation is recommended if....
|
it is performed with rigid adherence to specific precautions dictated by the nature of the tissue injury or surgical repair
|
|
|
|
What is the primary therapeutic limitation of AROM exercise?
|
it typically will not increase muscular strength or prevent atrophy
|
|
|
|
What is the primary therapeutic limitation of PROM exercise?
|
- it has little to no potential for even slowing muscle atrophy or maintaining strength
- it is also less effective than AROM at increasing circulation because of the lack of voluntary muscle contraction |
|
|
|
What key factors affect application and performance of ROM exercise techniques?
|
- supportive handling of body segments
- proper positioning of the patient - use of appropriate levels of force to avoid causing intense pain when performing the exercise |
|
|
|
What actions are taken during the Phase I - inflammatory phase of injury? ***
|
- protection phase
- patient education - application of modalities (e.g., cold pack, pulsed US) - selective rest/immobilization - passive movement (CPM or PROM) - muscle setting with caution (contraction of muscle without moving joint—isometric) - can perform active and resisted exercises at other areas - signs of too much movement are increased pain and/or inflammation |
|
|
|
What actions are taken during the Phase II - repair/sub-acute phase of injury? ***
|
- controlled-motion stage
- patient education - progress to non-destructive active, then resistive open and closed chain exercises as tolerated - muscular endurance exercises - carefully progress - emphasize control and proper mechanics - some discomfort will occur as activity is progressed, but should not last longer than couple of hours |
|
|
|
What actions are taken during the Phase III - remodeling phase of injury? ***
|
- return to function phase
- patient education (all phases) - progressive stretching, strengthening, endurance training - functional training - specificity drills |
|
|
|
Composition of ligaments ***
|
- dense connective tissue
- contain collagen, fibroblasts, extracellular matrix (scaffolding), elastin hypovascular (no vascularization if inside the joint capsule—less likely to heal -- e.g., ACL) - rich sensory innervation (= pain) - proprioception (single-leg standing, side-to-side shifting, etc.) |
|
|
|
Strength of ligament depends on: ***
|
- collagen:elastin ratio
(more collagen = stronger more elastin = more flexible) - anatomic location |
|
|
|
Ligament injury grades: ***
|
Grade I- microscopic tearing
- No laxity Grade II- tearing of some ligament fibers - moderate laxity - Grade III- complete rupture of ligament - profound laxity |
|
|
|
Ligament healing: ***
|
- remodeling and maturation are slow
- 1 year or more - can heal faster if more blood supply - usually, extracapsular ligaments heal better- because there is a vascular supply - tensile strength about 50%-70% |
|
|
|
In order for ligament damage to properly heal: ***
|
- torn ligament ends must be in contact
- ligaments heal by scar tissue proliferation, not ligament regeneration - progressive, controlled stress - protection against excessive forces |
|
|
|
Non-surgical vs. surgical repair of ligaments: ***
|
Non-surgical repair
- usually Grade I and II are most common injuries - protective bracing and rehab Surgical Repair - usually Grade III |
|
|
|
Immobilization for ligament repair: ***
|
must be limited, as stress deprivation can cause:
- joint stiffness - adhesion formation - shortening of ST - decreased ligament strength (and other ST, tendon, cartilage) - loss of bone - muscle atrophy - limited ROM |
|
|
|
What are the 3 (2) types of cartilage? ***
|
- Articular/hyaline (bone caps at ends of long bones)
- Fibrocartilage (discs, menisci) - Elastic (ears, larynx - not PT focus) (if 2, hyaline and fibroelastic) |
|
|
|
Composition of hyaline cartilage: ***
|
- water
- chondrocytes – cartilage cells - collagen (Type II) – strong, fibrous protein; gives strength to tissue - proteoglycans – molecules of sugar and amino acids that retain water, therefore providing more absorptive properties to the cartilage |
|
|
|
What are the characteristics of hyaline cartilage? ***
|
- durable, translucent material
- frictionless (better than ice) - dissipates compression, shear and tension forces - permeable - avascular (except deep) - receives nutrition from surrounding synovial fluid |
|
|
|
Types of injuries to hyaline cartilage ***
|
caused by
- joint instability - blunt trauma - repetitive overloading - immobilization - infection manifests as - blistering - fraying/fibrillation - splitting, fissuring, clefting |
|
|
|
Healing and repair of hyaline cartilage ***
|
- deeper lesions heal better than superficial lesions (if they expose subchondral bone blood vessels)
- healed/repaired articular cartilage inferior to normal |
|
|
|
Available noninvasive theraputic treatments for hyaline cartilage damage ***
|
- CPM
- limited weight-bearing activities |
|
|
|
Surgical management available for hyaline cartilage damage ***
|
Debridement
- remove particles of cartilage and other debris - usually only temporary benefit - arthroscopic procedure Microfracture - surgically abrading or fracturing multiple small holes through cartilage layers down to bone to stimulate bleeding - initiates the healing process Osteochondral Autograft Transplantation System (OATS) - full-thickness articular lesions - filled with transplanted plugs - taken from minor load-bearing surface (superior lateral femoral condyle) Autologous Chondrocyte Transplantation - requires two surgical procedures - 1st - harvest cartilage from minor load bearing surface - cultured for 4-6 weeks - 2nd surgery - transplant new cartilage |
|
|
|
Alternative management of hyaline cartilage damage ***
|
Oral Glucosamine and Chondroitin Sulfate
- supplement taken daily - not FDA regulated Intra-articular Hyaluronic Acid Injection |
|
|
|
Examples of fibroelastic cartilage: ***
|
- acromioclavicular joint
- sternoclavicular joint - glenohumeral joint - hip - knee - intervertebral discs |
|
|
|
What is the composition of fibroelastic cartilage? ***
|
- water
- collagen - elastin - proteoglycans |
|
|
|
What is the function of fibroelastic cartilage? ***
|
- dissipate compressive loads
- shock absorption - joint stability |
|
|
|
Most common means of injury of fibroelastic cartilage ***
|
Traumatic
- usu. < 40 y.o. - running, jumping, twisting (macrotrauma) Degenerative - usu. > 40 y.o. - usually a minor event precipitates sx. (microtrauma) |
|
|
|
Healing of fibroelastic cartilage ***
|
- injury to peripheral borders easier to heal because peripheral 10% - 30% is vascularized
- healing through inflammatory response mechanism |
|
|
|
Fibroelastic cartilage zones ***
|
- Zone I: red-on-red
- Zone II: red-on-white - Zone III: white-on-white - red-on-red and red-on-white considered reparable - white-on-white not so much due to lack of blood supply |
|
|
|
Surgical repair (of menisci) ***
|
- partial or total meniscectomy (outpatient and WBAT right away)
- meniscal repair - more extensive rehab because of NWB status |
|
|
|
Rehabilitation for sub-total or total meniscectomy ***
|
- reduce swelling and pain
- increase strength and ROM - improve gait, aerobic fitness, proprioception - usually WBAT right away |
|
|
|
Rehabilitation for surgical repair of meniscus/menisci: ***
|
Same goals as meniscectomy
- decrease pain and swelling - increase ROM and strength - improve gait, aerobic fitness, proprioception - FWB 4-6 weeks post surgery |
|
|
|
Sprain vs. strain ***
|
- injury to ligament
- injury involving muscle and tendon |
|
|
|
Indirect vs. direct muscle injuries ***
|
Indirect muscle injury
- muscle or musculotendinous junction injured by stretch or contraction Direct muscle injury - injury from laceration, incision, contusion, blunt trauma |
|
|
|
Healing of muscle tissue ***
|
- muscle is highly vascular
- has ability to regenerate - angiogenesis |
|
|
|
Effects of immobilization on muscle ***
|
- atrophy
- decreased extensibility - decreased weight - decreased force generating capacity - increased tough connective tissue |
|
|
|
Muscle rehabilitation after immobilization ***
|
- begin with ROM, then isometric exercise
- progress to dynamic muscle contractions - may add electrical stimulation |
|
|
|
Composition of tendons ***
|
- collagen (75%)
- elastin (2%) - other proteins |
|
|
|
Healing of tendons ***
|
- hypovascular, generally
- more vascularity near muscle and bone - slows healing time - healed tendon does not have same quality as non-injured tendon tissue |
|
|
|
Effects of motion and immobilization on tendon healing ***
|
- early motion provides increased mobility, but decreased tendon strength
- need balance of motion & rest |
|
|
|
Sternocleidomastoid origin
(2409) |

|
- sternal (medial) head: top of manubrium (ventral surface)
- clavicular (lateral) head: superior and anterior surface of medial 1/3 of clavicle |
|
|
Sternocleidomastoid insertion
(2409) |

|
- lateral surface of mastoid process of temporal bone
- lateral half of superior nuchal line of occiput |
|
|
Trapezius (middle) origin
(2409) |
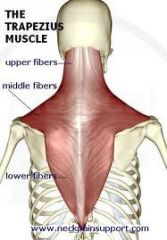
|
spinous processes of T1-T5 vertebrae
|
|
|
Trapezius (middle) insertion
(2409) |
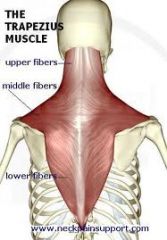
|
scapula (medial margin of acromion, spine of scapula, and crest of its superior lip)
|
|
|
Trapezius (lower) origin
(2409) |
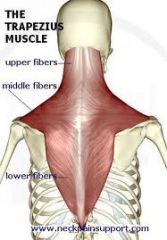
|
spinous processes of T6-T12 vertebrae
|
|
|
Trapezius (lower) insertion
(2409) |
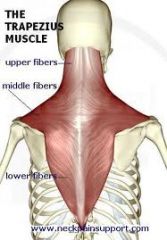
|
scapular spine
|
|
|
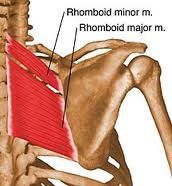
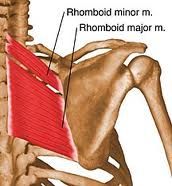
Rhomboid (major) origin
(2409) |

|
spinous processes of T2-T5
|
|
|
Rhomboid (major) insertion
(2409) |
|
medial border of the scapula between the root of the spine and inferior angle
|
|
|
Rhomboid (minor) origin
(2409) |
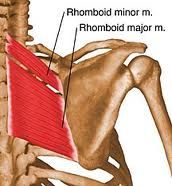
|
spinous processes of C7-T1
|
|
|
Rhomboid (minor) insertion
(2409) |
|
upper portion of medial border of the scapula across from root of spine
|
|
|
Deltoid (anterior) origin
(2409) |

|
clavicle (anterior border and superior surface of lateral 1/3)
|
|
|
Deltoid (anterior) insertion
(2409) |

|
deltoid tuberosity of humerus
|
|
|
Deltoid (middle) origin
(2409) |

|
scapula (acromion, lateral margin, and superior surface)
|
|
|
Deltoid (middle) insertion
(2409) |

|
deltoid tuberosity of humerus
|
|
|
Pectoralis major origin
(2409) |

|
clavicular/upper fibers
- medial half of anterior clavicle sternocostal/lower fibers - sternum and cartilage of ribs 1-6 |
|
|
Pectoralis major insertion
(2409) |

|
Crest of greater tubercle of humerus
(intertubercular sulcus, lateral border via a bilaminar tendon) |
|
|
Subscapularis origin
(2409) |
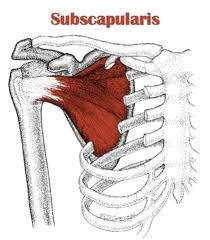
|
subscapular fossa of the scapula
|
|
|
Subscapularis insertion
(2409) |
|
lesser tubercle of humerus
|
|
|
Infraspinatus origin
(2409) |
|
infraspinous fossa of the scapula
|
|
|
Infraspinatus insertion
(2409) |
|
greater tubercle of humerus
|
|
|
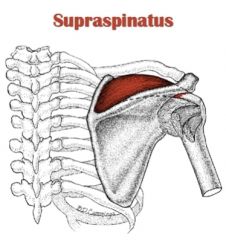
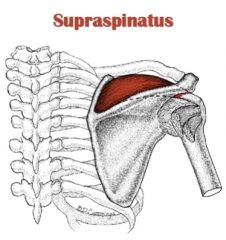
Supraspinatus origin
(2409) |
|
supraspinous fossa of the scapula (medial 2/3)
|
|
|
Supraspinatus insertion
(2409) |
|
greater tubercle of the humerus
|
|
|
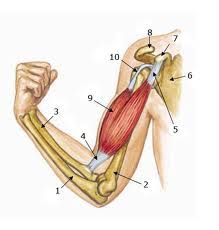
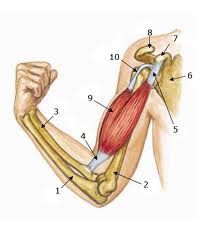
Biceps brachii origin
(2409) |
|
short head:
- coracoid process of scapula long head: - supraglenoid tubercle of scapula |
|
|
Biceps brachii insertion
(2409) |
|
tuberosity of the radius
|
|
|
Extensor carpi radialis longus origin
(2409) |

|
distal one-third of the lateral supracondylar ridge of the humerus
|
|
|
Extensor carpi radialis longus insertion
(2409) |

|
base of second metacarpal
(dorsal surface of base on radial side) |
|
|
Extensor carpi ulnaris origin
(2409) |

|
common extensor tendon from the lateral epicondyle of humerus
|
|
|
Extensor carpi ulnaris insertion
(2409) |

|
base of 5th metacarpal
(tubercle on underside of base) |
|
|
Quadratus lumborum origin
(2409) |

|
posterior iliac crest/inner lip
|
|
|
Quadratus lumborum insertion
(2409) |

|
- 12th (last) rib
- transverse processes of 1st through 4th lumbar vertebrae |
|
|
Sartorius origin
(2409) |

|
anterior superior iliac spine (ASIS)
|
|
|
Sartorius insertion
(2409) |

|
proximal, medial shaft of the tibia at the pes anserinus tendon (along with gracilis and semitendinosus)
|
|
|
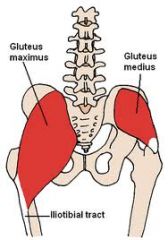
Gluteus maximus origin
(2409) |
|
- coccyx
- dorsal edge of sacrum - posterior iliac crest - sacrotuberous and sacroiliac ligament |
|
|
Gluteus maximus insertion
(2409) |
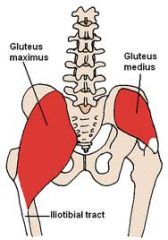
|
- iliotibial tract of TFL (upper fibers)
- gluteal tuberosity of femur (lower fibers) |
|
|
Gluteus medius origin
(2409) |
|
gluteal surface of ilium between the posterior and anterior gluteal lines just below the iliac crest
|
|
|
Gluteus medius insertion
(2409) |
|
lateral aspect of the greater trochanter of the femur
|
|
|
Piriformis origin
(2409) |
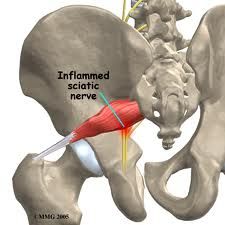
|
anterior surface of sacrum
|
|
|
Piriformis insertion
(2409) |
|
superior aspect of greater trochanter of the femur
|
|
|
Tensor fasciae latae origin
(2409) |

|
iliac crest posterior to the anterior superior iliac spine (ASIS)
|
|
|
Tensor fasciae latae insertion
(2409) |

|
iliotibial tract, which connects to the femur
|
|
|
Semitendinosus origin
(2409) |
|
ischial tuberosity (inferior medial aspect)
|
|
|
Semitendinosus insertion
(2409) |
|
proximal, medial shaft of tibia at pes anserinus tendon (along with sartorius and gracilis)
|
|
|
Biceps femoris origin
(2409) |
|
long head
- ischial tuberosity (inferior and medial aspects, common with semitendinosus) short head - lateral lip of linea aspera of femur |
|
|
Biceps femoris insertion
(2409) |
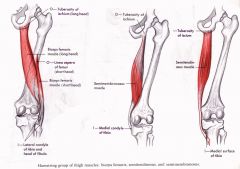
|
head of fibula
|
|
|
Tibialis anterior origin
(2409) |
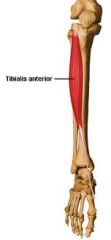
|
- lateral condyle of tibia
- proximal, lateral surface of tibia and interosseous membrane |
|
|
Tibialis anterior insertion
(2409) |
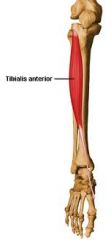
|
- medial cuneiform and
- base of first metatarsal |
|
|
Peroneus (Tertius) longus origin
(2409) |
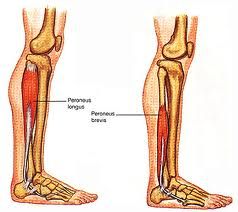
|
- head of fibula and
- proximal 2/3 of lateral fibula |
|
|
Peroneus (Tertius) longus insertion
(2409) |
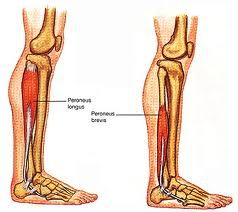
|
- base of first metatarsal and
- medial cuneiform |
|
|
Prime movers for scapular elevation
(2409) |
- trapezius (upper fibers)
- levator scapulae |
|
|
|
Prime movers for scapular adduction (retraction) and downward rotation
(2409) |
- rhomboid major
- rhomboid minor |
|
|
|
Prime movers for scapular adduction (retraction)
(2409) |
- trapezius (middle fibers)
- rhomboid major |
|
|
|
Prime movers for finger abduction
(2409) |
- dorsal interossei
- abductor digiti minimi |
|
|
|
Prime movers for finger adduction
(2409) |
- palmar interossei
|
|
|
|
Prime movers for thumb MCP and IP extension
(2409) |
- extensor pollicis brevis
- extensor pollicis longus |
|
|
|
Prime movers for thumb abduction
(2409) |
- abductor pollicis longus
- abductor pollicis brevis |
|
|
|
Prime movers for thumb adduction
(2409) |
- adductor pollicis (oblique and transverse heads)
|
|
|
|
Prime movers for trunk rotation
(2409) |
- external obliques (obliquus externus abdominis)
- internal obliques (obliquus internus abdominis) |
|

