![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
39 Cards in this Set
- Front
- Back
|
ALARA |
“As low as reasonably achievable” •Linear non-threshold: assumes that there is no minimum threshold of exposure necessary to achieve a biological effect. •It is the basis of radiation protection –It stresses that all radiation exposure (operator, staff, and patient) be kept as far below legal limits as possible |
|
|
Operator exposure |
Operators must stand in the control area behind protective barrier during exposure •A window (for viewing) having similar attenuation properties must me provided •Other provisions must be provided to maintain a line of communication with patient from behind the protective barrie |
|
|
Protective apparel and accessories |
Eyes and thyroid are highly sensible to radiation If the operator is required to remain in the exam room during the exposure, he/she must –Stand as far as practicable from the scattered radiation source –Wear appropriate protective apparel –Use personnel monitoring device Protective aprons, thyroid shields, and protective gloves –0.25 mm (Pb) to attenuate 97% of scattered radiation –Protective apparel MUST be hung properly to prevent cracking of material –Also allows putting the apparel on much easier |
|
|
Operator exposure |
Greatest threat is scatter radiation coming from patient •To a lesser degree, scatter radiation coming from tube x-ray table top, Bucky tray, or leakage radiation coming from tube housing •Irradiation only occurs when unit is activated Operators must stand in the control area behind protective barrier during exposure •A window (for viewing) having similar attenuation properties must me provided •Other provisions must be provided to maintain a line of communication with patient from behind the protective barrie |
|
|
Never hold patients!! |
All resources, means, devices, and other tools must be exhausted before a patient is held Guidelines for individuals who are occupationally exposed to radiation –Hold only in an emergency –NOT do be done routinely –Must wear appropriate shielding devices –Positioned so that no part of the operator's body will be struck by the useful beam –Must wear personnel monitoring device outside of the apron, collar level –Involve a parent is possible. Preferably the father Students shall not be permitted to hold patients
***Deliberate exposure of an individual for training or demonstration purposes is strictly forbidden |
|
|
Never hold patients!! |
All resources, means, devices, and other tools must be exhausted before a patient is held Guidelines for individuals who are occupationally exposed to radiation –Hold only in an emergency –NOT do be done routinely –Must wear appropriate shielding devices –Positioned so that no part of the operator's body will be struck by the useful beam –Must wear personnel monitoring device outside of the apron, collar level –Involve a parent is possible. Preferably the father Students shall not be permitted to hold patients
***Deliberate exposure of an individual for training or demonstration purposes is strictly forbidden |
|
|
Personnel monitoring |
Ionizing radiation cannot be sensed: cannot see, smell, hear, taste, or touch •Radiation detection devices are necessary to measure radiation levels or accumulated exposure (dose equivalent) to the individual •Radiation monitoring devices are ONLY to be worn on the job and stored in a safe place in the department (away from heat and radiation sources) •Monitoring devices DO NOT protect or shield the individual from exposure |
|
|
Types of monitoring devices |
1. Film badge 2. Thermoluminescent dosimeter (TLD) 3. Pocket dosimeter (PIC - pocket ionization chamber) 4. Optically stimulated luminescence dosimeter (OSL) |
|
|
Film badge |
Special, radiation-sensitive film placed in a lightweight plastic holder –Embedded filters screen out low level x- and gamma rays, as well as beta particles –The badge is returned after a designated period to be developed, assessed, and the accumulated dose recorded –Cannot be reused –Sensitive to doses 10mRem to 700 Rem |
|
|
TLD (Thermoluminescent dosimeter) |
Lithium fluoride crystals, hermetically sealed in light-tight holder –When crystals become ionized, they get into an excited state until the badge is read –The crystals are heated in a special measuring device that puts them back to their normal level. As they stabilize, light is emitted that is proportional to the amount of radiation in which they were exposed –Ideal for Nuclear Medicine –Sensitive to doses 10 mRem + |
|
|
Film badge positives and negatives |
(+) 1. Rugged and inexpensive 2. Permanent record
(-) 1. False reading produced by heat and pressure 2. + 25% error |
|
|
Film badge positives and negatives |
(+) 1. Rugged and inexpensive 2. Permanent record
(-) 1. False reading produced by heat and pressure 2. + 25% error |
|
|
TLD positives and negatives |
+) 1. + 9% error 2. Wide range of readings 3. reusable 4. Not heat sensitive (-) 1. Expensive 2. No permanent record 3. Increased sensitivity with use Must be replaced over time (they expire) |
|
|
Pocket ionization chamber. Also known as a direct reader pocket dosimeter (DRD) |
Ionization of air within the DRD is sensed and the electrical charges are stored –As the name suggest the DRD directly displays the dose reading for you to read, helping you to keep track of the dose you have received AS YOU WORK –Helps keep doses to the lowest limits. You can remove yourself from the area as those limits approach –Not exclusive. Must be used in addition to another monitoring device –Ideal for High Radiation Areas –Displays readings from 10 mRem |
|
|
PIC OR DRD |
(+) 1. Immediate readings 2. Reasonably accurate 3. Reusable 4. Small size
(-) 1. No permanent record 2. Must be periodically calibrated (zeroed) 3. Sensitive to mechanical shock 4. Subjective reading by reader 5. Limited dose range 6. Possible loss of info in the event of exposure past its maximum range |
|
|
OSL (optically stimulates luminescence dosimeter) |
Aluminum oxide crystals, hermetically sealed in light-tight holder –With optically stimulated luminescence, a tiny crystal traps and stores energy from exposure to ionizing radiation –The amount of exposure can be determined by shining a green light on the crystal and measuring the intensity of the blue light emitted –Sensitive to as low as 1mRem |
|
|
OSL positives and negatives |
(+) 1. + 1% error 2. Very sensitive 3. Reread 4. Reusable 5. Durable, water-resistant, heat resistant (-) 1. Expensive This is what we use for students |
|
|
Location of personal monitoring devices |
On collar outside of apron –Not on shirt pocket, pant pocket, belt loop, etc. –Worn under apron for certain circumstances –Reading of device considered whole-body dose –Devices are worn to assure limits are not exceeded –Changed out monthly or quarterly |
|
|
Reporting of overexposure |
Reported immediately to State Health Branch and X-ray Supervisors •Even if reading might be erroneous (wrong), protocol should be followed •Overexposure generally occurs –Cardiac cath lab –Special procedures –Careless portable work |
|
|
Who is monitored |
Persons who enter a high radiation area, which means any area in which there exists radiation at such levels that an individual could receive in any 1 hour, a dose to the whole body in excess of 100 mRem (at 30 cm)places like a nuclear plant •A radiation area means any area in which there exists radiation at such levels that an individual could receive in any 1 hour, a dose to the whole body in excess of 5 mRem (at 30 cm) this is us |
|
|
Maximum permissible dose equivalent (MPD)year |
Purpose is to keep the exposure of the occupationally exposed individuals well below a level which adverse effects are likely to be observed during the lifetime of the radiation worker •Although the risks are low, they increase with the dose received. Therefore, one should always observe ALARA |
|
|
Yearly dose limits |
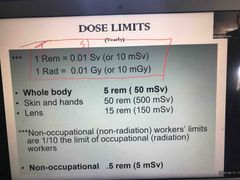
Back (Definition) |
|
|
Cumulative MPD |
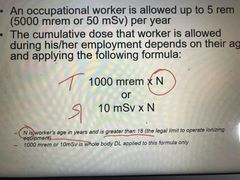
An occupational worker is allowed up to 5 Rem (5000 mRem or 50 mSv) per year •The cumulative dose that worker is allowed during his/her employment depends on their age and applying the following formula: 1000 mRem x N or 10 mSv x N |
|
|
Example of cumulative exposure |
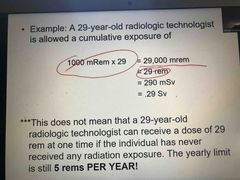
Back (Definition) |
|
|
Cardinal rule |
3 cardinal rules of radiation protection 1. Time 2. Distance 3. Shielding |
|
|
Cardinal rule |
3 cardinal rules of radiation protection 1. Time 2. Distance 3. Shielding |
|
|
Time |
–The dose rate to the patient is directly related to the dose rate and the duration (time) of the exposure –The operator exposure to scattered radiation is directly proportional to patient exposure |
|
|
Distance |
–The intensity of the radiation varies inversely as the square of the distance. It is obvious that the farther the person is from the x-ray source, the less radiation dose per unit time will be received |
|
|
Shielding |

Refers to different means used to stop radiation or prevent exposure from it –Most shielding devices will attenuate scatter radiation –Primary protective barrier: barrier that attenuate the useful or primary beam •1/16” of lead or equivalent •6.6 ft (79”) in height from the floor •Example: wall behind the chest unit –Secondary protective barrier: barrier used to attenuate scatter radiation •1/32” of lead or equivalent •Should extend from the primary barrier to the ceiling with at least ½” overlap |
|
|
Shielding continued |

Operator Station: the operator station at the control shall –be behind a protective barrier either in a separate room or –in a protective booth or –behind a shield that will intercept the useful and any radiation which has been scattered only once 2.Patient Observation and Communication: provisions shall be made for the operator to observe and communicate with the patient without leaving the shielded position at the control panel. When an observation window is used it must posses the same attenuation properties as the surrounding barrier
|
|
|
Examination of the pregnant or potentially pregnant patient |
A biological risk will always exist in which a radiologic examination is conducted. This is based on 3 assumptions: 1. There is always a small potential for adverse biological effects to occur following exposure to x-radiation 2. There is no threshold for such effects 3. Such effects are directly proportional to absorbed radiation dose |
|
|
10 day rule |
stated that it was “safe” to do abdominal and pelvic x-ray exams only during the 10 days following the onset of menstruation. We know much more today about radiation and pregnancy, and we know that substantial doses (~10 rad; more than is received from routine diagnostic medical x-ray exams) are necessary to cause birth defects or malformations. Since organogenesis starts 3 to 5 weeks post conception, it was felt that radiation exposure in early pregnancy couldn't result in malformation |
|
|
28 day ruleb |
now the focus is shifted to a missed period and the possibility of pregnancy. If there is a missed period, a female should be considered pregnant unless proved otherwise. The examination may proceed if the patient states she is not pregnant and has had a period within the last 28 days |
|
|
Signs posted in waiting room and examination room |
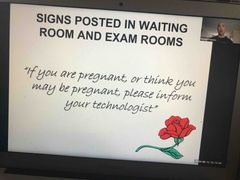
Back (Definition) |
|
|
Pregnant females question |
Question should be asked of all females of child-bearing age –Possibility and LKMP (last known menstrual period) •If Pregnant, referring physician should be notified –Postponed –Or if known, a limited study might be ordered •Shielding when possible •Exam should be kept to last trimester, or life and death circumstances |
|
|
Pregnancy continued |
Termination or interruption of pregnancy is never justified because of exposure of the embryo/fetus to a diagnostic x-ray examination •The risk to the embryo/fetus is considered to be negligible, or not significant, at 5 Rad or less when compared to other types of risks •Risks of malformation is significant at doses above 15 Rad. Most radiographic exams will never reach such levels. Therefore, malformation or termination of pregnancy will rarely be the cause of a radiologic procedure by itself |
|
|
Occupational pregnant woman |
As recommended by The National Council on Radiation Protection (NCRP)
•Exposure to the fetus shall be no greater than 0.05 Rem (50 mRem) in any month •And not to exceed 0.5 Rem (500 mRem) for the entire gestation period |
|
|
Notification to pregnant worker |
1. First trimester is most important as the fetus is most sensitive 2.In most cases, the actual dose received by the fetus is less than the dose received by the mother 3.At the present occupational dose equivalent limits, the risk to the unborn baby is considered small, although some experts will disagree 4.There is no need for women to be concerned with sterility or the ability to bear children 5.The NCRP recommendation that once pregnancy is known, exposure of the fetus shall be no greater than 0.05 Rem in any month 6.The NCRP recommendation of 0.5 Rem dose equivalent limit applies to the full 9 months of pregnancy |
|
|
Pregnant worker options |
1. Delay having children as long as one works around radiation 2.If pregnant, leave the job 3.Could be temporarily reassigned 4.Use protective aprons 5.Never hold patients 6.Do not perform portable and surgical x-ray exams 7.Do not assist in special and fluoroscopic procedures 8.Use two personnel monitoring devices: one outside at collar level, and the second inside at abdomen level 9.Stay out of the x-ray room and behind the protective barrier |

