![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
47 Cards in this Set
- Front
- Back
|
What is responsible for the first heart sound (S1)?
|
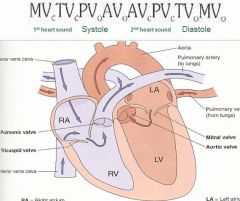
Closure of AV valves (tricuspid and mitral).
|
|
|
What is responsible for the second heart sound (S2)?
|
Closure of semilunar valves (aortic and pulmonic).
|
|
|
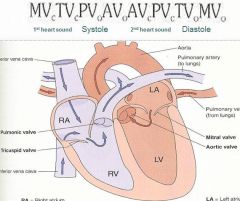
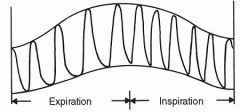
Describe the cardiac pressure curve through systole and diastole.
|
|
|
|
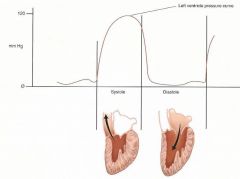
Describe what S3 is?
|
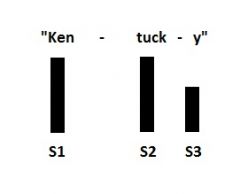
An extra heart sound (pathologic) which represents ventricular filling and is caused by volume overload (congestive heart failure). Can be normal in youth, athletes and pregnant women. Timing of sounds has same rhythm as "Kentucky".
|
|
|
Describe what S4 is?
|
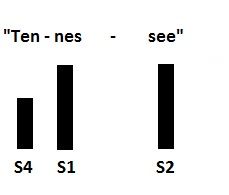
An extra heart sound (pathologic) which represents atrial contraction and is caused by a stiff left ventricle. Timing of sounds has same rhythm as "Tennessee".
|
|
|
What is a summation gallop?
|
It signifies an S3 and S4.
|
|
|
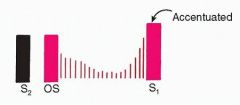
What would you expect to hear for a physiologic splitting of S2? How would you hear it the best?
|
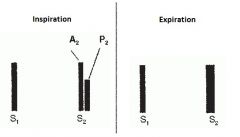
Detected at 2nd or 3rd left intercostal space (pulmonic listening point). Accentuated by inspiration, disappears on expiration. Abnormal if heard on expiration.
|
|
|
What is physiologic splitting of S1 due to? Where would you auscultate to hear it?
|
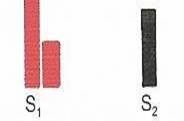
Tricuspid and mitral valves not closing simultaneously. Mitral component is louder than the tricuspid component. Heard best at tricuspid listening point (left lower sternal border) and does not vary with respiration. Not pathological.
|
|
|
Describe the location of the cardiac auscultatory points? How do auscultate them?
|
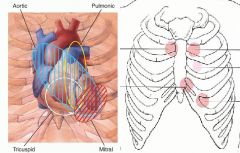
Listen to all auscultatory points with the diaphragm of the stethoscope, then listen with the bell at the tricuspid and mitral listening points.
|
|
|
What is an ejection click?
|
Opening sound of the aortic or pulmonic valve due to pathology. High pitched sound heard best with the diaphragm in early systole.
|
|
|
What is a systolic click?
|
Midsystolic click due to mitral valve prolapse. High pitced sound heard with the diaphragm at LLSB, frequently followed by a ejection murmur.
|
|
|
What is an opening snap?
|
Opening sound of mitral valve (rarely tricuspid) indicating pathology. High pitched sound heard best with the diaphragm in early diastole.
|
|

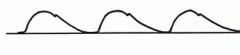
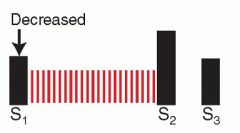
What kind of murmur is this?
|
Midsystolic murmur.
|
|

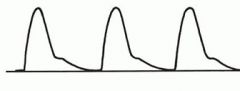
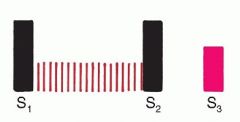
What kind of murmur is this?
|
Holosystolic murmur.
|
|

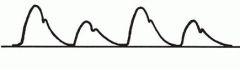
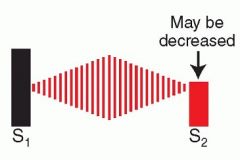
What kind of murmur is this?
|
Late systolic murmur.
|
|
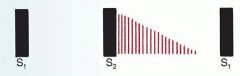
What kind of murmur is this?
|
Early diastolic murmur.
|
|
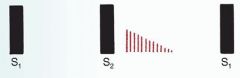
What kind of murmur is this?
|
Mid diastolic murmur.
|
|

What kind of murmur is this?
|
Late diastolic murmur.
|
|

What kind of murmur is this?
|
Crescendo murmur.
|
|
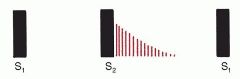
What kind of murmur is this?
|
Decrescendo murmur.
|
|

What kind of murmur is this?
|
Crescendo-decresendo murmur.
|
|

What kind of murmur is this?
|
Plateau murmur.
|
|
|
List different qualities that a murmur can have.
|
Blowing:sounds like air rusing out.
Harsh:like sandpaper over wood. Rumble: large tires over cut strips in a highway. |
|
|
Where can aortic murmurs radiate to?
|
Carotids or apex if loud enough.
|
|
|
Where can mitral murmurs radiate to?
|
Left axilla.
|
|
|
Where can tricuspid murmurs radiate to?
|
Right lower sternal border.
|
|
|
Where can pulmonic stenosis murmur radiate to?
|
Left neck or shoulder if loud enough.
|
|
|
Describe the grading of systolic murmurs.
|
Grade 1: Very faint, heard after listener has “tuned in”, not heard in all positions.
Grade 2: Quiet, but readily heard, not necessarily in all positions. Grade 3: Moderately loud, heard in all positions to varying extent. Grade 4: Loud with a palpable thrill. Grade 5: Very loud, with thrill, heard with stethoscope in partial contact with chest. Grade 6: Very loud, with thrill, can be heard with stethoscope off the chest or with the naked ear. |
|
|
What postion can you put a patient in to better hear a aortic murmur?
|
Have them exhale and lean forward.
|
|
|
What postion can you put a patient in to better hear a mitral murmur?
|
Left lateral decubitus postion.
|
|
|
What kind of maneuver can you use to affect venous return to the heart to help identify heart sounds?
|
Standing/squatting and valsalva maneuver. Standing and the strain phase of valsalva decrease left ventricular volume and vascular tone (from decreased venous return to heart and decreased arterial blood pressure). Squatting and release of valsalva increase left ventricular volume and vascular tone (from increased venous return to heart, and increased arterial blood pressure peripheral vascular resistance).
|
|
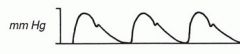
What kind of arterial pulse wave is this?
|
Normal pulse wave.
|
|
What kind of arterial pulse wave is this?
|
Small, weak pulse wave. May be caused by decreased stroke volume (hypovolemia or severe aortic stenosis), or increased peripheral resistance (congestive heart failure or exposure to cold).
|
|
What kind of arterial pulse wave is this?
|
Large, bounding pulse wave. May be caused by increased stroke volume or decreased peripheral resistance (anemia, aortic regurgitation, arteriovenous fistulas or patent ductus arteriosus), or increased stroke volume because of slow heart rate, or decreased compliance of the aortic walls (aging or artherosclerosis).
|
|

What kind of arterial pulse wave is this?
|
Bisferiens pulse wave. Caused by aortic regurgitation (with or without stenosis) or even hypertrophic cardiomyopathy.
|
|
What kind of arterial pulse wave is this?
|
Pulsus alternans pulse wave. Indicates left ventricular failure and is usually accompanied by a left-sided S3.
|
|
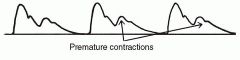
What kind of arterial pulse wave is this?
|
Bigeminal pulse wave. Normal beat alternating with a premature contraction.
|
|
What kind of arterial pulse wave is this?
|
Paradoxical pulse wave. Systolic pressure decreases by more than 10 mm Hg during inspiration. It is found in pericardial tamponade, constrictive pericarditis, and obstructive lung disease.
|
|
|
What would you hear with a mitral regurgitation? What is the mechanism?
|
Harsh, holosystolic sound heard at the apex. When the mitral valve fails to close fully in systole, blood regurgitates from left ventricle to left atrium, causing a murmur. This leakage creates volume overload on the left ventricle, with subsequent dilatation. Several structural abnormalities cause this condition, and findings may vary accordingly.
|
|
|
What would you hear with a tricuspid regurgitation? What is the mechanism?
|
Blowing, holosystolic sound heard at the lower left sternal border. When the tricuspid valve fails to close fully in systole, blood regurgitates from right ventricle to right atrium, producing a murmur. The most common cause is right ventricular failure and dilatation, with resulting enlargement of the tricuspid orifice. Either pulmonary hypertension or left ventricular failure is the usual initiating cause.
|
|
|
What would you hear with a ventricular septal defect? What is the mechanism?
|

Harsh, holosystolic sound heard at the 3rd-5th left interspaces. A ventricular septal defect is a congenital abnormality in which blood flows from the relatively high-pressure left ventricle into the low-pressure right ventricle through a hole.
|
|
|
What would you hear with a innocent/physiologic murmur? Why?
|

Low grade murmur head at 2nd-4th left interspaces. Innocent murmurs result from turbulent blood flow, probably generated by ventricular ejection of blood into the aorta from the left and occasionally the right ventricle. Common in children and yound adults.
Physiologic murmur is due to temporary increase in blood flow in predisposing conditions such as anemia, pregnancy, fever, and hyperthyroidism. |
|
|
What would you hear with a aortic stenosis? What is the mechanism?
|
Often harsh (may be musical at apex), crescendo-decresendo sound heard at right 2nd interspace. Significant aortic valve stenosis impairs blood flow across the valve, causing turbulence, and increases left ventricular afterload. Causes are congenital, rheumatic, and degenerative; findings may differ with each cause. Other conditions mimic aortic stenosis without obstructing flow: aortic sclerosis, a stiffening of aortic valve leaflets associated with aging; a bicuspid aortic valve, a congenital condition that may not be recognized until adulthood; a dilated aorta, as in arteriosclerosis, syphilis, or Marfan's syndrome; pathologically increased flow across the aortic valve during systole can accompany aortic regurgitation.
|
|
|
What would you hear with a hypertrophic cardiomyopathy? What is the mechanism?
|

Harsh sound heard at the 3rd and 4th interspace. Massive ventricular hypertrophy is associated with unusually rapid ejection of blood from the left ventricle during systole. Outflow tract obstruction of flow may coexist. Accompanying distortion of the mitral valve may cause mitral regurgitation.
|
|
|
What would you hear with a pulmonic stenosis? What is the mechanism?
|

Often harsh , crescendo-decrescendo sound heard at the 2nd and 3rd left interspaces. Pulmonic valve stenosis impairs flow across the valve, increasing right ventricular afterload. Congenital and usually found in children. In an atrial septal defect, the systolic murmur from pathologically increased flow across the pulmonic valve may mimic pulmonic stenosis.
|
|
|
What would you hear with a aortic regurgitation? What is the mechanism?
|

Blowing decrescendo heard at 2nd-4th left interspaces. The leaflets of the aortic valve fail to close completely during diastole, and blood regurgitates from the aorta back into the left ventricle. Volume overload on the left ventricle results. Two other murmurs may be associated: (1) a midsystolic murmur from the resulting increased forward flow across the aortic valve and (2) a mitral diastolic (Austin Flint) murmur, attributed to diastolic impingement of the regurgitant flow on the anterior leaflet of the mitral valve.
|
|
|
What would you hear with a mitral stenosis? What is the mechanism?
|
Decrescendo low-pitched rumble and an opening snap heard at the apex. When the leaflets of the mitral valve thicken, stiffen, and become distorted from the effects of rheumatic fever, the mitral valve fails to open sufficiently in diastole. The resulting murmur has two components: (1) middiastolic (during rapid ventricular filling) and (2) presystolic (during atrial contraction). The latter disappears if atrial fibrillation develops, leaving only a middiastolic rumble.
|

