![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
31 Cards in this Set
- Front
- Back
|
What is the order of the abdominal evaluation?
|
Look, listen, feel, percuss.
|
|
|
What organs are found in the left and right upper quadrants?
|

Liver, gallbladder, duodenum, spleen, stomach, pancreas.
|
|
|
Describe the topography of the abdomen in 2 ways.
|
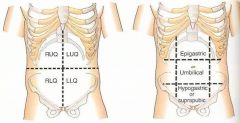
|
|
|
Describe the alimentary tract.
|
Starts at the mouth and ends at the anus; includes esophagus, stomach, duodenum, jejunum, ileum, colon, and sigmoid. Approx. 27 feet long. Functions to ingest and digest food, absorb nutrients, electrolytes and water, and excrete waste.
|
|
|
List organs in the abdomen according to quadrant.
|

|
|
|
What are you looking for when inspecting the abdomen?
|
Skin, shape (distention), symmetry, masses, scars, hernias, venous pattern, aortic pulsations.
|
|
|
Where do you auscultate the abdomen and for what?
|
First auscultate all four quadrants for bowel sounds. Then listen with bell for vascular sounds (bruits).
|
|
|
How should the abdomen be percussed?
|

First percuss around all four quadrants. Then percuss the liver.
|
|
|
If patient has pain in the abdomen, how should it be percussed?
|
Percuss away from the pain first, then get closer to the area of pain.
|
|
|
What is the normal liver span?
|
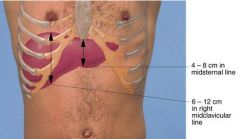
|
|
|
What do you assess when palpating the abdomen?
|
Assess structures (liver, spleen, kidney), rigidity, pain, organomegaly, guarding, rebound, and subcutaneous structures.
|
|
|
What is the finger "hook" technique used for?
|
To palpate the liver.
|
|
|
How is hepatomegaly measured?
|
It is measured in centimeters below costal margin. The findings of hepatomegaly should lead to an abdominal exam for fluid.
|
|
|
What is ascites?
|
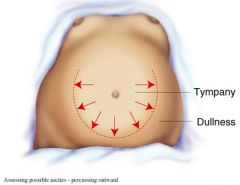
Free fluid in the peritoneal cavity. Most common cause is portal hypertension. Systons usually result from abdominal distention.
|
|
|
What is a fluid wave?
|
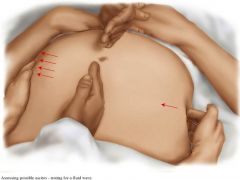
Used to determine ascites, occurs when one side of the abdomen is tapped and a fluid wave is felt on the opposite side.
|
|
|
How is ascites tested for when the patient is lying on their his/her side?
|
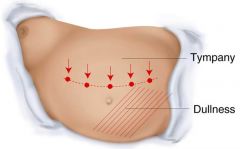
Test for shifting dullness; dullness shifts to the more dependent side and tympany shifts to the top.
|
|
|
How do you palpate the spleen?
|

|
|
|
How do you palpate the kidney?
|

|
|
|
What is rebound tenderness?
|
On palpation of the abdomen, press down slowly then remove your hands quickly. Watch the patient for signs of a distinct flinch upon brisk withdrawal of the examiner's hand, which signifies a positive test. Positive rebound tenderness implies peritoneal inflammation (peritonitis) and is indicative of an acute abdomen/perforation.
|
|
|
How do you palpate if the patient is ticklish?
|
Place his/her hand in between yours.
|
|
|
What is McBurney's sign?
|
Right lower quadrant tenderness halfway between the umbilicus and the ASIS (McBurney's point). Test for appendicitis.
|
|
|
What is Rovsing's sign?
|
Pain felt in the right lower quadrant with palpation of the left lower quadrant. Test for appendicitis.
|
|
|
What is the psoas sign?
|
An increase in pain from passive extension of the right hip joint that stretches the iliopsoas muscle, or flexing hip against resistance. Test for appendicitis, psoas muscle irritated by inflamed appendix.
|
|
|
What is the obturator sign?
|
Pain caused by passive internal rotation of the thigh. Test for appendicitis, obturator muscle irritated by inflamed appendix.
|
|
|
What is guarding?
|
An involuntary contraction of the abdominal muscles that is slightly slower and more sustained than the rapid, voluntary flinch exhibited by sensitive or anxious patients.
|
|
|
What is Murphy's sign?
|
Test for cholecystitis. A sharp increase in tenderness with sudden stop in inspiratory effort constitutes a positive Murphy's sign while doing the finger hook technique.
|
|
|
What does acute abdominal perforation lead to?
|

Peritonitis, a critical condition that needs surgery immediately. Dx is usually made by the presence of free air in the abdomen below the diaphragm.
|
|
|
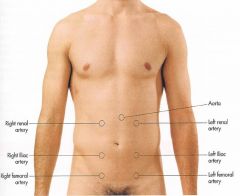
Why do we palpate for abdominal aortic pulsations?
|
Screen for abdominal aortic aneurysm (AAA). Any above 3 cm suggests AAA.
|
|
|
Why do we test costovertebral angle tenderness?
|
CVA tenderness (kidney punch) screens for pyelonephritis, an infection of the kidney and the ureters, the ducts that carry urine away from the kidney.
|
|
|
Where is referred kidney and ureter pain felt?
|
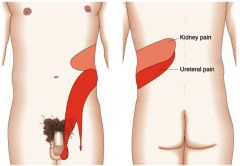
|
|

|

|

