![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
84 Cards in this Set
- Front
- Back
|
Muscle precursor
|
1.) Precursor a tissues and cells are MESODERM; loosely organized connective tissue AKA mesenchyme
|
|
|
Mesoderm vs mesenchyme
|
1.) USUALLY, mesenchyme is a mesoderm derivative HOWEVER, mesenchyme may also be derived from ectoderm (neural crest cells).
2.) Mesenchymal connective tissue is a type of undifferentiated loose connective tissue. 3.) Mesenchyme referes to the MORPHOLOGY of the embryonic cells (i.e. mesenchymal cells can migrate very easily) 4.) Mesenchyme is contains a substance matrix of loose aggregate of reticular fibrils and unspecialized cells, which retain the ability to develop into connective tissues. 5.) Cells in the mesoderm layer of the embryo are called MESOBLAST CELLS. |
|
|
Somites (3 subdivisions)
|
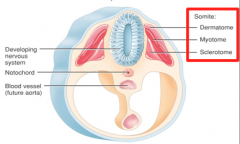
1.) Dermatome: develops into skin
2.) Myotome: develops into muscle 3.) Sclerotome: develops into bone 4.) The first two start out as dermatomyotomes, skeletal muscles arise from this. |
|
|
Myotomal somite derivates
|
1.) There are 38 in total
2.) 4 occipital myotomes: form the pharynx, upper neck, and occipital region. 3.) 8 cervical myotomes: form the neck and shoulders muscles. 4.) 12 thoracic myotomes: form the muscles of the upper extremities, breast, and abdominal wall. 5.) 5 lumbal myotomes: form the muscles of the lower extremities. 6.) 5 sacral and 4-5 coccygeal myotomes: form the muscles of the lower pelvis and gluteal region. |
|
|
Mesoderm changes as it moves laterally across the embryo.
|
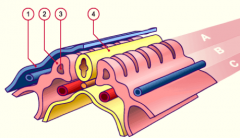
(A) Skeletal musculature arises from the paraxial mesoderm
(B) intermediary mesoderm (C) lateral plate mesoderm 1.) ectoderm 2.) Somite 3.) Somitocoel 4.) Neural tube Other myoblasts formt eh cardiogenic and myocardial plates. |
|
|
Skeletal muscle formation
|
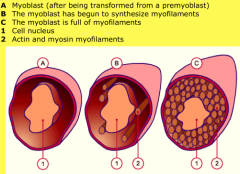
1.) PREMYOBLASTS: the first specific and determine cells of myogenesis.
2.) Premyoblasts are transformed into MYOBLASTS (vai a change in gene expression) at the site of the future muscle. 3.) Myoblasts synthesize myosin myofilaments and actin. 4.) Myoblasts fuse into multicellular MYOTUBES (syncytium), with nuclei that lie in the middle of each cell. 5.) By the end of embryonic development the nuclei move to the periphery and myotubes have lengthened, and striations are recognizable. |
|
|
The pharyngeal arches
|
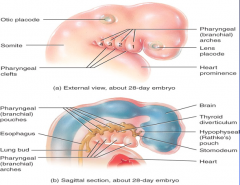
1.) 5 pairs
2.) Consist of ectoderm, mesoderm, and endoderm as well as blood vessels, cranial nerves, cartilage, and muscle tissue. 3.) The skeletal and musculature portion of the pharynx and face are derived from these. 4.) ***The nerves are ALREADY present prior to muscle formation (unlike innervation of the extremities). |
|
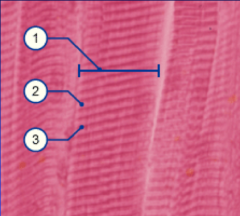
Longitudinal skeletal muscle (histo.)
|
1.) Myofibril
2.) I-band (light) 3.) A-band (dark) |
|
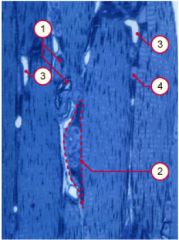
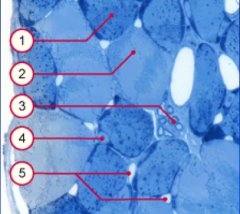
Histogenesis of muscle tissue
|
1.) Myelinated axon
2.) neuromuscular junctions 3.) capillaries 4.) muscle fiber nucleus 5.) At the end of the embryonic period, nuclei move into the periphery of the myotubes below the basal membrane. 6.) Neuromuscular junctions appear around 6 weeks on the myotubes and myotubes fuse, resulting in the characteristic striations. 7.) Myotubes are innervated polyneurally (by many neurons) on different portions of their surfaces. After both, these extra connections are lost and become mononeural. |
|

Histology of adult skeletal muscle (transverse section)
|
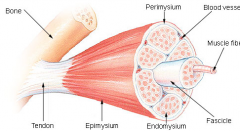
F = fascicle
En = endomysium (blood vessel, nerves, and lymphatics are found here, reticulin fiber and some collagen) P = perimysium (around fascicle, large vessels and nerves, collagen) E = epimysium (collagenous sheath) |
|
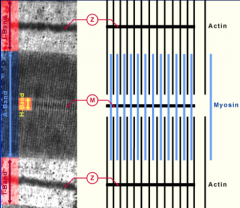
Sarcomeres (histo.)
|
.
|
|
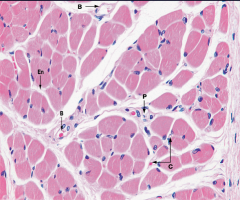
Blood supply to skeletal muscle
|
B = blood
En = endomysium P = perimysium C = capillaries 1.) Each muscle finer is in contact with 1-3 capillaries, which run along the fiber |
|
Red (fast twitch) and white (slow twitch) skeletal muscle fibers
|
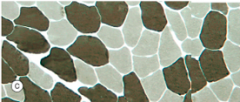
1.) Red muscle fiber: smaller diameter, but MORE myoglobin.
2.) White muscle fiber: large diameter 3.) Myelinated axons 4.) Muscle fiber nucleus 5.) Capillaries |
|
|
Cardiac muscle development
|
1.) Derived from lateral splanchnic mesoderm surrounding the heart tube, cardiac myoblasts differentiate from the primordial myocardium.
2.) Do not fuse like skeletal muscle, but rather remain as individual cells in fiber formation. 3.) These cells are connected to one another via adhering junctions (intercalated disks). 4.) Nuclei are centrally located, 1-2 per cell. 5.) Later in embryonic development, specialized bundles of muscle cells develop, with a large diameter and few myofibrils, to become the Purkinje fibers. 4.) Cell become branched |
|
|
Intercalated disks
|
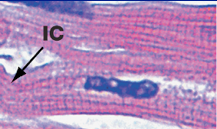
1.) Made up of 3 types of adhering junctions
2.) fascia adherens: anchor sites for actin and connect sarcomeres. 3.) Macula adherens (desmosomes): bind intermediate filaments together, joining the cells together so that they don't separate during contraction. 4.) Gap junctions: allow action potentials to spread between cardiac cells by allowing ions to pass between cells. |
|
|
Smooth muscle contraction
|

1.) Crisscrossed contractile proteins, rather than striated like skeletal muscle, anchor into the focal densities in the cytoplasm or on the cell membrane.
2.) Contraction results in a shortening of the cell from spindle shaped to globular. 3.) Can be regulated by signaling through a second messenger system. 4.) Usually found in viscera, where it is arranged in sheets and can be used to change the diameter of the lumen. 5.) Innervated by the ANS, smooth muscle has its own rhythmic contraction, but can be stimulated by stretch signals via gap junctions. 6.) Maintains a high force of contraction with little ATP use, compared to skeletal muscle. |
|
|
Smooth muscle development
|
1.) Starts out very dense, but cells become tapered at each end, with a single nucleus, and NO striations.
2.) Develop from splanchnic mesenchyme around the primordial gut. 3.) As they develop into sheets or bundles, they receive INDEPENDENT autonomic innervation. |
|
|
Bone and cartilage development
|
1.) Condensation of mesenchymal cells into bone and cartilage models.
2.) Mesenchymal cells differentiate into chondroblasts and osteoblasts. 3.) Intramembrane ossification: Sheet-like layers of bone form directly within the mesenchyme. (intra = within) 4.) Endochondral ossification: bone forms within the HYALINE cartilage that developed from the mesenchyme. (endo = into) |
|
|
Cartilage histogenesis
|
1.) Develops from the mesenchyme, cells differentiate into chondroblasts, which secrete cartilaginous fibrils and extracellular matrix while collagenous and/or elastic fibers are deposited in the intracellular matrix.
2.) 3 types of cartilage Hyaline: in joints, most widely distributed. Fibrocartilage: in intervertebral discs Elastic: in auricle of ear |
|
|
Bone histogenesis
|
1.) Mesenchymal cells differentiate into osteoblasts
2.) Compact bone: provides weight-bearing strength and is found in the shaft of long bones. 3.) Spongy bone: growth occurs here, found mostly at the ends of long bones. |
|
|
Classification of bones by shape
|
1.) Long bones: longer than they are wide, subjected to most of the load during daily activities (i.e. femur).
2.) Short bones: as wide as they are long. Their primary function is to provide support and stability with little to no movement. (i.e. carpals) 3.) Flat bones: principal function is either extensive protection or the provision of broad surfaces for muscular attachment. (i.e. skull bones) 4.) Irregular bones: varying shapes 5.) Sesamoid: a bone embedded within a tendon. (i.e. patella) |
|
|
Bone cell types (3)
|

1.) OsteoBlasts: build bone (upregulated by calcitonin)
2.) OstroClasts: break down bone (c looks like pac man) (upregulated by parathyroid hormone) 3.) Osteocytes: form from osteoblasts, maintain equilibrium in fully formed bone. (trapped in bone) |
|
|
Intramembranous bone formation
|
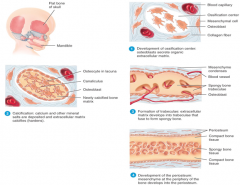
Direct ossification of mesenchymal models
1.) Ossification centers develop, osteoblasts serete extracellular matrix. 2.) Calcification: Ca2+ and other minerals deposit in the extracellular matrix, which hardens. 3.) Trabeculae form: form extracellular matrix, fuse to form spongy bone 4.) Periosteum develops: mesenchyme at the edge of the bone become the periosteum. |
|
|
Endochondral bone formation
|
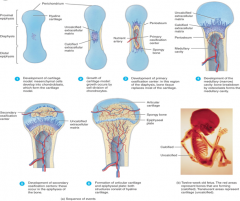
1.) Cartilage model forms; mesenchymal cells develop into chondroblasts, which form the model.
2.) Growth by cell division of the chondrocytes. 3.) Primary ossification center develops: in the diaphysis, bone tissue begins to replace cartilage. 4.) Medullary cavity develops: osteoclasts break down the inside of the bone as it grows outwards to form a cavity. 5.) Secondary ossification: Occur in the epiphyses of bones. 6.) Articular cartilage and epiphyseal plates form, which are both made of hyaline cartilage. |
|
|
Parts of a bone
|

1.) Proximal and distal epiphysis: heads of bones
2.) Metaphysis: between the epiphysis and the diaphysis, contains the growth plate. (meta = middle) 3.) Diaphysis: shaft of bone. |
|
|
Bone growth in length
|

|
|
|
Bone growth in width
|
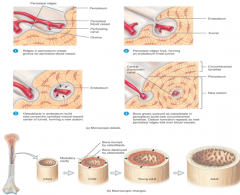
|
|
|
Compact bone structure
|
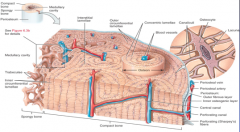
1.) Osteocytes grow in concentric lamellae around blood vessels in central canals (Haversian canals), connected by horizontal vessels (Volkmann canals).
2.) Osteocytes are trapped in the lacuna ("lake") of the bone, and communicate with each other via projections through small channels called canaliculi. |
|
|
Spongy bone structure
|

1.) Trabeculae form the spongy bone
2.) Also made up of concentric lamella and osteocytes. 3.) Lined by osteoblasts and osteoclasts. |
|
|
Bone healing
|
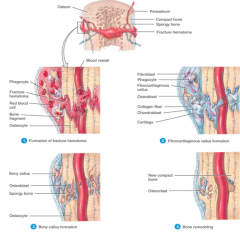
1.) Formation of fracture hematoma (but only if the ends are near each other).
2.) Fibrocartilaginous callus formation via fibroblasts, osteoblasts begin rebuilding the ends together 3.) Bony callus forms around the break site. Osteoblasts get trapped in the newly formed bone and become osteocytes. 4.) Wider areas of the healed bone are degraded by osteoclasts, bone remodeling. |
|
|
Bone blood supply
|
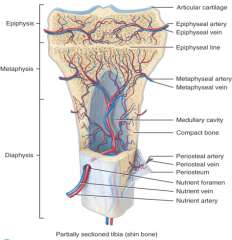
1.) Nutrient arteries/veins enter/exit the bone via a nutrient foramen.This supplies the diaphysis of the bone.
2.) The metaphyseal arteries/veins supply the metaphysis of the bone. 3.) The epiphysis is suppled by the epiphyseal arteries/veins. 4.) Nerves also follow the blood vessels. |
|
|
Development of the cranium
|
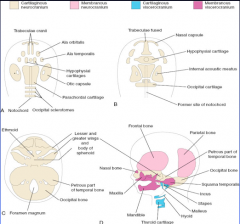
1.) Starts as cartilage, the chondrocranium
2.) SOme of the paired cartilages fuse after 7 weeks 3.) By 20 weeks some of the cartilage is replaced by bones. 4.) After birth the remaining cartilaginous portions of the cranium are called fontanelles. |
|
|
Factors involved in bone growth and remodeling
|
1.) Vit D : Mainly absorbed through sunlight, but also by absorption from diet. Help maintain blood Ca2+ levels be increasing absorption in intestines. Lack of fit D results in soft, brittle bones (Rickets).
2.) Calcium is required for growing bones and remodeling 3.) Phosphorus is required for growing bones and remodeling 4.) Magnesium, fluoride, and manganese are required in small amounts for remodeling 5.) Vit A: stimulates osteoblast activity 6.) Vit C: required for collagen synthesis 7.) Vit K and B12: required for synthesis of bone protein. 8.) Human growth hormone: promotes bone growth indirectly by upregulating IGF production. 9.) IGF: stimulates osteoblasts, cell division in the epiphyseal plate and periosteum, and synthesis of proteins required for bone growth. 10.) Thyroid hormone (T3 and T4): stimulate osteoblast. 11.) Insulin: increases synthesis of bone proteins. 12.) Sex hormones (estrogens and androgens): increase osteoblast activity and synthesis of bone extracellular matrix during growth spurt of the teenage years, but after puberty when levels of these hormones stabilize bone growth stops. Bone growth is specific to sex, i.e. females grow wider pelvises. |
|
|
Osteoporosis
|

1.) Loss of bone mass via demineralization.
2.) Bones become weaker and more fragile. 3.) Results from increased osteoclast activity. 4.) Potential treatment is to inhibit activity of osteoclasts |
|
|
Calcium homeostasis
|
![1.) The main regulating factor is parathyroid hormone.
2.) Ca2+ receptors detect changes in blood [Ca2+] and increase cAMP production in response.
3.) cAMP upregulates parathyroid hormone gene transcription.
4.) PTH secretion increases
...](https://images.cram.com/images/upload-flashcards/72/56/51/2725651_m.png)
1.) The main regulating factor is parathyroid hormone.
2.) Ca2+ receptors detect changes in blood [Ca2+] and increase cAMP production in response. 3.) cAMP upregulates parathyroid hormone gene transcription. 4.) PTH secretion increases 5.) PTH increases blood [Ca2+] by activating osteoclasts to reabsorb bone more quickly. 6.) This is a negative feedback loop. |
|
|
Compound (open) bone fracture vs simple fracture
|
1.) Compound: the broken end of the bone protrudes through the skin
2.) Simple: the fracture does not break the skin. |
|
|
Commuted fracture
|

1.) The bone is splintered, crushed, or broken into piece at the site of impact, with small fragments between the 2 main pieces.
|
|
|
Greenstick fracture
|

1.) A partial fracture in which one side of the bone break and the other side bends.
2.) Occurs in children whose bones have not fully ossified. |
|
|
Impacted fracture
|
1.) One end of the fractured bone is driven forcefully into the other end of the bone.
|
|
|
Pott fracture
|

1.) Fracture of the distal end of the lateral fibula, with serious injury to the distal tibial articulation.
|
|
|
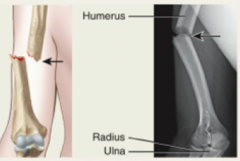
Colles' fracture
|

1.) Fracture of the distal end of the radius in which the distal fragment is displaced posteriorly.
|
|
|
Mechanical stress of bone tissue
|
1.) Bone becomes stronger across lines of stress via increased deposition of mineral salts and production of collagen fibers by osteoblasts.
2.) High impact intermittent strain has a greater effect on deposition. 3.) Mechanical stress results from the pull of gravity or skeletal muscle on bones. |
|
|
Myofibril contractile proteins
|
1.) Myosin: thick filaments, in all 3 muscle types. Convert chemical energy form ATP to mechanical energy by pulling cellular structures to produce a force for movement. Made up of 2 light and 2 heavy chains, the heads of the heavy chain bind actin and hydrolyze ATP.
2.) Actin: alpha-helical thin filaments, each molecule has a myosin binding site. Associated with tropomyosin and troponin. |
|
|
Excitatory contraction coupling
|

1.) Membrane depolarization opens L-type Ca2+ channels (long-lasting voltage gated channel).
2.) Mechanical coupling between L-type Ca2+ channels and the Ca2+ release channel causes the Ca2+ release channel to open. 3.) Ca2+ exits the sarcoplasmic reticulum via the Ca2+ release channel and activates troponin C, leading to muscle contraction. 4.) Ca2+ entering the cell can also activate L-type Ca2+ channels, rather than a membrane depolarization, which can in turn activate Ca2+ release channels. This pathway is more important to cardiac muscle rather than skeletal muscle. |
|
|
Sarcoplasmic reticulum
|
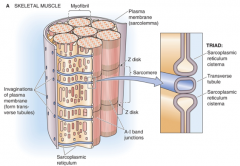
1.) Transverse (T) tubules: invaginations of the muscle cell that form radially projecting tubules, which penetrate the muscle fibers and myofibrils at the A and I bands of the sarcomere.
2.) The T tubules associate with 2 cisternae, specialized regions of the sarcoplasmic reticulum. The combination of these 3 pieces is called the triad. |
|
|
Muscle contraction
|
1.) ATP binds to the myosin head, causing it to dissociate from the actin filament.
2.) ATP is hydrolyzed, causing the myosin head to return to its resting conformation. 3.) Cross-bridge formation, myosin head binds to a new position on the actin filament. 4.) Inorganic phosphate release changes the myosin head conformation resulting in the power stroke. 5.) ADP is released. |
|
|
Phosphocreatine as an energy source
|
1.) Adequate for replenishing ATP pools, but can't sustain energy needs for contracting muscle for more than 10 seconds.
2.) Long-term, sustained ATP regeneration comes from respiration (aerobic or anaerobic). 3.) Muscle do not store ATP. |
|
|
Calsequestrin and cal reticulin
|
1.) Ca2+ binding proteins
2.) buffer the [Ca2+] increase in the sarcoplasmic reticulum during re-uptake of Ca2+ after contraction. 3.) Calsequestrin is the principle Ca2+ binding protein in skeletal muscle, although present in cardiac and smooth muscle. 4.) Calreticulin is ubiquitous 5.) Have up to 50 Ca2+ binding site. |
|
|
Growth and regeneration of skeletal muscle
|
1.) Muscle fibers can't divide, but can sometimes be replaced individually by new muscle fibers from satellite cells.
2.) Satellite cells are muscle cell precursors that can fuse with each other to form new fibers. 3.) However, major muscle damage can't be overcome. |
|
|
Isotonic contraction
|
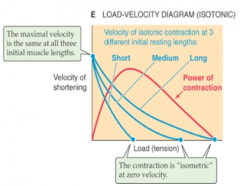
1.) Holding a muscle contraction i.e. lifting a weight and holding it in place.
2.) The speed of muscle shortening during contraction is much higher for lighter objections. 3.) Also, longer muscles can develop a greater tension than short muscles. |
|
|
Motor units
|
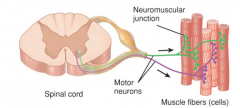
1.) Functional unit of a muscle
2.) Consists of a motor neuron and the muscle fiber it controls 3.) The number of fibers innervated by one motor neuron can vary, but when stimulated it initiates an impulse that causes all of the fibers to contract simultaneously. 4.) Motor units with more muscle fibers can contract more forcefully than those with less fibers. |
|
|
Motor unit recruitment
|
1.) Process of increasing the number of active motor units.
2.) The weakest motor units are recruited first, and progressively stronger units add on if more force is necessary. 3.) An excitatory stimulus will generate a larger EPSP in motor neurons with smaller cell bodies, which is why the smaller motor units take less effort to recruit and larger motor units take longer (size principle). |
|
|
Neuron pool
|

1.) The group of all motor neurons innervating a single muscle
|
|
|
Muscle contraction and summation
|
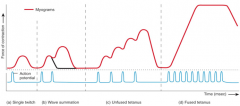
1.) A muscle TWITCH is a brief contraction of all the muscle fibers in a motor unit in response to a single action potential.
2.) Wave summation is the increased strength of contraction that occurs when a second stimulus arrives BEFORE the muscle fibers has completely relaxed from the previous stimulus. 3.) Multiple-fiber summation allows the force developed by the while muscle to be relatively constant over time. 4.) The CNS can activate motor units asynchronously, so that some units relax while others develop tension, thus keeping the force even when individual fibers are not stimulated to tetanus. 5.) Smooth, non-tetanic contraction is essential to fine motor control. |
|
|
Isotonic vs isometric
|
1.) Isometric: attachment points are immobile, thereby fixing the muscle length. Stimulus causes an increase in tension, but not in muscle length.
2.) Isotonic: One of the 2 attachment points is mobile, and the force tends to pull this mobile pint away from the fixed point. Stimulation causes shortening as tension increases. |
|
|
Slow oxidative, fast oxidative-glycolytic, and fast glycolytic fibers
|

1.) Slow oxidative fibers (red): Used for endurance, aerobic respiration. Smallest fiber diameter, largest myoglobin content, and have many mitochondria. Use ATP up slowly, contract slowly, highly fatigue resistant, lowest amounts of creatine kinase and glycogen stores. Recruited first.
2.) Fast oxidative-glycolytic fibers (pink): used for both aerobic and anaerobic respiration. Intermediate in diameter with a large amount of myoglobin and many mitochondria. Use up ATP fast, contract quickly, moderate resistance to fatigue, and a moderate amount of creatine kinase and glycogen storage. Recruited second. 3.) Fast glycolytic fibers (white): Used for aerobic respiration. Largest fiber diameter, smallest amount of myoglobin, few mitochondria. Use up ATP fast, contract quickly, fatigue quickly, highest amount of creatine kinase and glycogen storage. Recruited last. |
|
|
Joint (def.)
|
1.) Also called an articulation or arthrosis
2.) Def: point of contact between 2 bone, bone and cartilage, or bone and teeth. |
|
|
Joint classification; structural and functional
|
1.) Structural: based on anatomical characteristics
(a) Fibrous: No joint cavity and no movement, held together by dense irregular connective tissue (b) Cartilaginous: No joint cavity , held together by cartilage (c) Synovial: Have a joint (synovial) cavity and are held together by dense irregular connective tissue of an articular capsule or ligaments 2.) Functional: based on the type and degree of movement. (a) Synarthrosis: immovable joint (syn = together) (b) Amphiarthrosis: Slightly movable joint (amphi = either or, i.e. movable and immovable) (c) Diarthrosis: Freely moveable joint, all are synovial. |
|
|
Synovial Joint
|
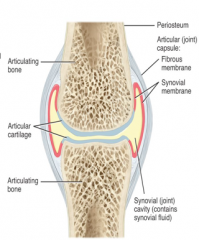
Includes:
1.) Articulating cartilage on the ends of the bones in the joint 2.) Synovial membrane around the joint 3.) Synovial cavity with fluid 4.) 2 bones 5.) Dense irregular connective tissue or ligament capsule |
|
|
Types of synovial joints (6)
|
1.) Plane joint (bi- or triaxial)
2.) Pivot joint (uniaxial) 3.) Hinge joint (uniaxial) 4.) Condyloid joint (biaxial) 5.) Saddle joint (biaxial) 6.) Ball-and-socket joint (triaxial) |
|
|
Planar joint
|
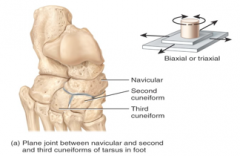
|
|
|
Pivot joint
|
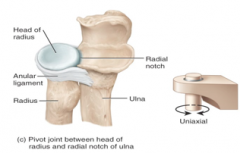
|
|
|
Hinge joint
|
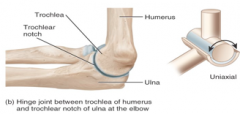
|
|
|
Condyloid
|
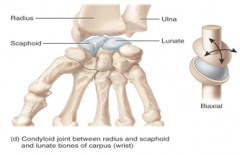
|
|
|
Saddle joint
|
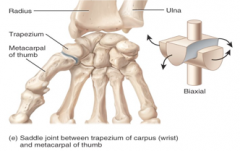
|
|
|
Ball-and -socket joint
|
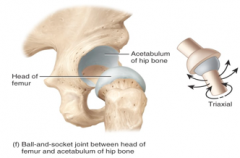
|
|
|
Fibrous joints
|
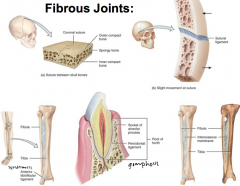
1.) No cavity, with bones held very close together by dense irregular connective tissue. Do not permit movement.
2.) 3 types: (a) Sutures (b) Syndesmoses (c) interosseous membranes |
|
|
Fibrous joint - suture
|

1.) sutur = seam
2.) Occur only between bones of the skull 3.) Composed of a dense layer of irregular connective tissue 4.) The irregular, interlocking edges of the sutures gives them added strength and reduces the risk of fracture 5.) Immovable (adults) or slightly moveable (children) 6.) Important role in shock absorption in the skull 7.) Synostosis: joint in which 2 bones completely fuse together (os- = bone), falls under synarthrosis |
|
|
Fibrous joints - syndesmosis
|

1.) syndesmo = band or ligament
2.) Limited movement is permitted by the dense irregular connective tissue bundle. 3.) Greater distance between the articulating surfaces and more dense irregular connective tissue than sutures |
|
|
Fibrous joint - interosseous membrane
|

1.) A large sheet of dense irregular connective tissue
2.) Binds neighboring bones 3.) Permits slight movement |
|
|
Cartilaginous joints types (2)
|
1.) Synchondroses
2.) Symphyses (symphysis) |
|
|
Cartilaginous joint - synchondroses
|
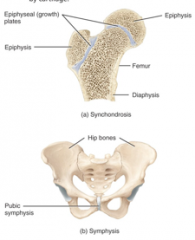
The connecting tissue in the joint is hyaline cartilage. Immovable joint. Eventually, replaced by bone (i.e. growth plates).
|
|
|
Cartilaginous joint - Symphyses (symphysis)
|

1.) The ends of the articulating bones are covered with hyaline cartilage, but they are connected to each other by a flat disc of fibrocartilage.
2.) All symphyses are midline structures 3.) Slightly movable |
|
|
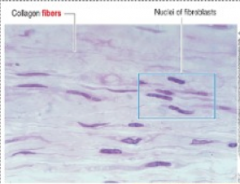
Dense regular connective tissue (histo.)
|

|
|
|
Fibrous connective tissue (histo.)
|
|
|
|
Synovial joints (histo.)
|

|
|
|
Epiphysis (histo.)
|
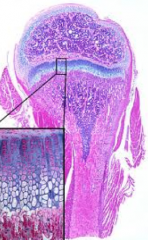
|
|
|
Articular cartilage and synovial membrane (synovium)
|
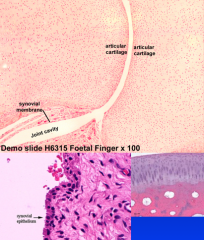
|
|
|
Bursa and tendon sheaths
|
1.) Provide padding and joint lubrication
2.) NOT located in the joint 3.) Tendon sheath: bursa around a tendon, that reduces friction for the tendon that slide through it 4.) Bursa: Fluid filled sack, synovial-like fluid |
|
|
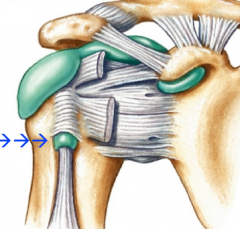
Shoulder joint
|
Unique because the "ball" of the joint is larger than the "socket" of the joint
|
|
|
Elbow joint
|
1.) Ball and socket - ulnar-humurous
2.) Pivot - radial-humurous |
|
|
Hip joint
|
1.) Ball and socket
2.) Fovea on head of femur where an intra-joint ligament attaches to the head of the femur |
|
|
Knee joint
|
1.) Patella slides over knee joint
2.) Hinge joint 3.) Minisus |
|
|
Atlanto-axial joint
|
1.) Atlas: holds the occipital condyles of the skull.
2.) Axis: the atlas pivots around this |

