![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
117 Cards in this Set
- Front
- Back
|
Normal Flora
|
Mo that establishes itself, has a permanent residence on or in specific locations of your body and doesn't usually cause disease in those locations under normal conditions
|
|
|
Opportunistic Flora
|
Normal flora moved to an abnormal location resulting in disease.
|
|
|
Transient Flora
|
Mo in the body or certain location for a short amount of time.
|
|
|
Origination of normal flora
|
Infant exposure & Internal
|
|
|
Infant exposure
|
Vaginal normal flora, 8-12hrs after birth begin to develope their external normal flora.
|
|
|
Internal
|
Food consumed, and breast milk. By 1yrs old normal adult-like flora has developed in the infant.
|
|
|
Normal Flora Body Sites
|
Skin, Mucous membranes, UR system, Mouth, GI Tract, & External urethra
|
|
|
Skin & mucous membranes
|
Staphylococcus aureus &
Staphylococucs epidermidis |
|
|
UR System
|
Staph a. , Staph e. , & Streptococcus pneumoniae
|
|
|
Mouth
|
Strep. mutans (tooth decay causing)
& Salivarius |
|
|
GI Tract
|
Escherichia coli & Lactobacillus
|
|
|
outer opening of Urethra
|
Staph. a, & Staph e.
|
|
|
Vagina
|
Candida albicans
|
|
|
Sterile sites
(HLKBLBSMBOTGSMII) |
heart circulatory system, liver, kidneys, bladder, lungs, brain spinal cord, muscles, bones, ovaries, testes, glands (pancreas, salivary), sinuses, middle & inner ear, and internal eye.
|
|
|
Sterile Fluids
(BUSSSA) |
Blood, urine, spinal fluid (CSF), saliva(prior to mouth entery), seemen, & amniotic fluid
|
|
|
Reservoirs
|
Natural host or habitat for pathogen
|
|
|
3 Main Types of Reservoirs
|
Type 1- Human, Type 2- Animal, Type 3- Non-living
|
|
|
Type 1 Human
Multiple types |
1. Symptomatic
2. Asymptomatic 3. Passive Carrier |
|
|
Symptomatic Reservoir
|
Signs ad symptoms of disease are displayed
ex. Chicken pox |
|
|
Asymptomatic Carriers
|
Somone who has recovered from the disease, but retains the organism in or on the body & continues to shed the organism.
Ex. Typhoid fever |
|
|
Passive Carrier
|
Nosocomial transfer (accidently occured). Hospital aquired infection.
|
|
|
3 Common Nosocomial infections
|
1. Urinary- catheters
2.Respiratory- equipment used 3. Post-op surgical incision- prevent infection |
|
|
Type 2- Animal
|
Zoonoses- disease from wild or domestic animals that can be given to humans.
Ex. Flu |
|
|
Type 3- Non-Living
|
Soil
Ex. Clostridium tetani (lives in soil) |
|
|
4 Modes of Transmition from reservoirs
|
Contact, Airborne, Vector, & Common vehicle
|
|
|
Contact is divided into 3 possibilities
|
Direct, in-direct, & droplet
|
|
|
Direct Contact
|
Shaking hands, kissing, etc.
from reservoir to host |
|
|
Indirect Contact
|
From reservoir to a fomite to a new host
fomite-inanimate obj. that can harbor or spread disease. ex. door knobs, sink handles |
|
|
Droplet Contact
|
From reservoir to air to new host. Less than 1 meter.
ex. Flu |
|
|
Airborne
|
From resevoir to air to new host. Greater than 1 meter.
Ex. TB, & Measles |
|
|
Vector
|
Carrier.
Ex. animal that carries a diseas. Biological- a bite.,Mosquitos, or feces-flys. |
|
|
Common Vehicle
|
Water, blood, food, and air.
|
|
|
Incidence
|
&of population infected in a particular location during a particular time period.
Ex. Spanish flu |
|
|
Prevalence
|
Current stats.
Ex % of peopole in OK, reported to have had the flu withing the last few weeks. |
|
|
Endemic
|
Native disease that prevails continuously in a geographical region.
Ex. Lyme disease |
|
|
Epidemnic
|
Many people in a certain given area having the disease. (outbreak)
Ex. Influenza |
|
|
Severity- 2 types
|
acute or chronic
|
|
|
Acute
|
Develops rapidly & lasts a short time.
Ex. Common cold |
|
|
Chronic
|
Develops slowly & lasts a long time, possibly a lifetime.
Ex. Leprosy, & TB |
|
|
Latent
|
Dorment, inactive
|
|
|
Primary Disease
|
One that develops in a healthy person
|
|
|
Secondary Disease
|
Individual that's a compromised host, has an impaired immune system.
|
|
|
5 Periods of developement of disease
|
1. Period of Incubation
2. Period of Prodromal 3 Period of Illness 4. Period of Decline 5. Period ofConvalescence |
|
|
Period of Incubation
|
Interval between time the infection is received & the 1st symptom appears.
|
|
|
Period of Prodromal
|
2nd phase of symptoms occur
|
|
|
Period of Illness
|
Manefest display fully developed. Ex. rash spread head to toe
|
|
|
Period of Decline
|
Declining of symptoms .Primary disease declining, immune system impaired,secondary could come.
|
|
|
Period of Convalescence
|
Healthy feeling but become asymptomatic carrier of the disease.
|
|
|
2 Types of Specific Routes
|
Mucous membranes & Parenteral
|
|
|
4 Types of Mucous Membranes
|
Respiratory Tract, GI Tract, Genitourinary Tract, & Eye
|
|
|
Respiratory Tract
|
Flu, common cold, measles, and TB
|
|
|
GI Tract
|
Food & water that has been contaminated.
Ex. Hep. A, Typhoid fever, Cholera, Polio, & Desentery |
|
|
Genitourinary Tract
|
STD's
Ex. Syphilus & UTI |
|
|
Eye
|
Conjuctivitis
|
|
|
Parenteral
|
Bite, wound, or injection
Ex. Rabies, Staph, MRSA, & Tetanus |
|
|
ID 50
|
Infectious dose that effects 50% of those exposed
|
|
|
LD 50
|
Lethal dose that kills 50% of those exposed
|
|
|
Cholera
|
In water, require to develope the disease. 1 trillion cells. Occurs in drought, it becomes concentrated. Flood causes the spreading of huge quantity of the disease.
|
|
|
Q Fever
|
Requires 1 cell to get the disease and kill.
|
|
|
Action of Penetration
|
Local or Systemic
|
|
|
Penetrate
|
Penetrate and access the cell, develope and enter the tissue.
|
|
|
Local
|
Remains in specific location.
Ex. Lesion |
|
|
Systemic
|
Spreads, invades into other systems of the body.
|
|
|
4 Types of Systemic Disease
|
1. Bacteremia
2. Septicemia 3. Toxemia 4. Viremia |
|
|
Bacteremia
|
Prescence of bacteria in the blood.
|
|
|
Septicemia
|
Prescence of bacteria in the blood and is reproducing, spreading & thriving in the blood. A killer.
|
|
|
Toxemia
|
Toxic in the blood
|
|
|
Viremia
|
Virus in the blood
|
|
|
How does it attach to the host?
|
Bacteria could attach by the capsule, common pilae, fimbriae, spikes and hooks (worms)
|
|
|
Supports the establishment of disease in the tissues
|
Virulent Factors
|
|
|
3 Virulent Factors
|
1. Exoenzymes
2. toxins 3. Antiphagocytic |
|
|
Exoenzymes
|
Virulance enhancing enzyme. Bacteria, fungi, protozoans, & multicellular produce exoenzymes. Extremely damaging.
Bacterial Exoenzymes |
|
|
Coagulase
|
Cause clotting of the plasma in the blood.
Ex. most common caused by Staphylococcus aeurius |
|
|
Kinases
|
Dissolves clots
Ex. Streptokinase & Staphylokinase |
|
|
Toxin
|
Specific chemical product of an mo.
|
|
|
Toxigenicity
|
Power to produce toxin.
|
|
|
Toxinoses
|
Diseases caused by toxins.
|
|
|
Intoxication
|
To ingest toxins.
|
|
|
Exotoxin
|
Body prduces antibodies, than antitoxins.
|
|
|
Antitoxin
|
Provides immunity to an exotoxin.
|
|
|
Taxoid
|
An altered exotoxin. Used in vaccines.
Ex. Tetanus, Diphtheria |
|
|
Characteristics of Exotoxins
|
1. In some gram (+) & some gram (-)
2. Toxic in small amounts 3. Secreted from living bacteria cell 4. Composed of protein 5. The toxin, not the mo, causses the disease . Specifically attack specific cell types |
|
|
Characteristics of Endotoxins
|
1. In all gram (-) bacteria
2. Toxic in large amounts 3. Released from dead or dying mo 4. Composition in cell wall, LPS is toxic 5. Goes systemic: effects-shock, fever lethargic 6. Pyrogenic (fever causing) ex. Salmonella typhi, Typhoid fever |
|
|
4 Types of Groupings
|
1. Neurotoxins
2. Enterotoxins 3. Hemotoxin 4. Cytotoxin |
|
|
Neurotoxins
|
Attacks nervous system
Chlostridium tetani- Tetanus Chlostridium botulinum- Botulism |
|
|
Enterotoxins
|
Attacks intestines
Ex. Vibrio cholerae- Cholera |
|
|
Hemotoxin
|
Attacks RBC
Ex. Staphylococcus aeurias- MRSA Streptococcus pyrogenes- Strep throat |
|
|
Cytotoxin
|
Attacks & kills cells
Ex. Diphtheria |
|
|
Phagoctes
|
protective cells to aid in destroying bad cells
|
|
|
leukocidins
|
1. Kill WBC's
2. Have huge capsules 3. Some can live inside phagocytes after ingestion Ex. Mycobacterium |
|
|
3 levels of defense
|
Thery are overlapping in case one fails to protect
|
|
|
1st line of defense
|
Resistance immunity. Barrier- any barrier that blocks the invasion of a part of entry. Non- specific
Physical barriers- skin, taers, coughing, sneezing (mucous membranes) Chemical barriers- lysozyme- found in tears, saliva, secretions, & can destroy cell walls of gram (+) Genetic barriers- resistance (pathogn can't invade) |
|
|
2nd line of defense
|
non-specific, inflammation, phagocytosis, & interferon
|
|
|
Whole blood
|
Formed elements and a fluid that they circulate in.
|
|
|
Leukocytes
|
WBC's - 2 groups: Granulocytes & Agranulocytes
|
|
|
Granulocyte
|
When stained, see large grains.
Ex. Netrophils (phagocytes)- used in process of phagocytosis. Also called Macrophage Eosinophil basophil Infections in the body are noted from the count of these WBC's |
|
|
Agranulocyte
|
Lack large granules.
Ex. Lymphocytes & Monocytes |
|
|
Lymphocytes
|
T -Cells (Thymus) & B-Cells ( Bone marrow)
|
|
|
Monocytes
|
Also a phagocyte
Macrophages |
|
|
Erythroctes
|
RBC's
|
|
|
Platelets
|
Thrombocytes
|
|
|
Plasma
|
Formed elements circulate in it. Contains clotting protein.
|
|
|
Serum
|
Not plasma. Has no clotting protein. Fluid that's left out that extrudes when a clot forms.
|
|
|
Lymph
|
Thick yellow fluid
|
|
|
Lymph Nodes
|
Clustered & drainage site located in armpit, intestijne, and Inguinal
|
|
|
Organs included in lymph system
|
Tonsils, MALT, GALT, Thymus, & Spleen
|
|
|
Interferon
|
Interferes with viral replication
|
|
|
Basic Process of Phagocytosis
|
1. Chemotaxis-Attraction towards/away a chemical
2. Complement- specialized enzyme for coding mo's Attract phagocytes 3. Phagocytes- ingest the mo's. Use their pseudopod 4. Digestion |
|
|
Inflammation
|
4 Symptoms of injury- Pain, redness, swelling, & warmth
|
|
|
Benefits to inflammation
|
Notice it & maintainence it. Destruction of the invader is occuring. it's kept local & isolated, repairs are occuring. Causes vasodiolation.
|
|
|
Vasodiolation
|
Increases the diameter of the vessels. These are opened pathway to allow phagocytes to enter to begin repair. Increases permeability
|
|
|
Hypothalamus
|
Controls body temperature.
|
|
|
Fever
|
Elevated core temperature
|
|
|
3rd line of defense
|
Specific, results in long term immunity.
Ex. T-cells, B-cells, antibodies |
|
|
Define normal flora & discuss the development of human normal flora.
|
Normal flora is when a mo establishes itself as a permanent resident in or on a specific location of the body and doesn’t usually cause disease in those locations under normal conditions. When normal flora moves to an abnormal location resulting in disease, it becomes opportunistic flora. Transient flora is when a mo is in the body or certain location for a short amount of time. The origination of normal flora is either from infant exposure or Internal. Infant exposure is from the normal flora in the vaginal area. The infants external flora begins to develop 8-12hrs after birth. Internal is from food or breast milk. By one years of age the baby has normal adult-like flora. There are several normal flora body sites. The skin and mucous membranes which contain Staphylococcus aureus & Staphylococcus epidermidis. The upper respiratory system has Staphylococcus aureus, Staphylococcus epidermidis, & Streptococcus pneumonia. The mouth contains Streptococcus mutans & Salivarius. The GI tract has Escherichia coli &Lactobacillus. The outer opening of the urethra has Staphylococcus aureus & Staphylococcus epidermidis. Finally, the vagina contains Candida albicans. These resident microbes remain on the outer surface without penetrating into sterile tissues or fluids.
|
|
|
In an organized proper manner, list toxins in table form.
|
Toxin Specific chemical product of a mo
Toxigenicity Power to produce toxin Toxinoses Diseases caused by toxins Intoxication To ingest toxins Toxemia Toxic in the blood Antitoxin Provides immunity to exotoxin Toxoid altered exotoxin, used in vaccines Ex. Tetanus & Diphtheria Endotoxin Bacterial intercellular toxin that's not ordinarily released Ex. Typhoid fever & Salmonella typhi Exotoxin A toxin that’s secreted & acts upon a specific cellular target Neurotoxin attacks nervous system Ex. Chlostridium tetani-Tetanus & Chlostridium botulinum- Botulism Enterotoxin attacks intestines EX. Vibrio cholera- Cholera Hemotoxin attack RBC’s Ex. Streptococcus pyrogenes- Strep throat & Staphylococcus aureus- MRSA Cytotoxin attacks & kills cells Ex. Diphtheria |
|
|
List & Discuss 2 types of toxins
provide drawing of cell wall to the endotoxin side when discussing the composition of endotoxin, LPS |
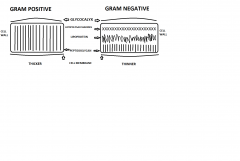
Exotoxins
1. In some gram (+) & some gram (-) 2. Toxic in small amounts 3. Secreted from living bacteria cell 4. Composed of protein 5. The toxin, not the mo, causses the disease . Specifically attack specific cell types Endotoxins 1. In all gram (-) bacteria 2. Toxic in large amounts 3. Released from dead or dying mo 4. Composition in cell wall, LPS is toxic 5. Goes systemic: effects-shock, fever lethargic 6. Pyrogenic (fever causing) ex. Salmonella typhi, Typhoid fever |

