![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
114 Cards in this Set
- Front
- Back
|
1st & 2nd Line of Defense
|
Non-specific
|
|
|
3rd Line of Defense
|
Specific, results in long term immunity.
Ex. T-Cells, B-Cells, & Antibodies (Ab) |
|
|
Antigens
|
Chemical substances, usually a non-self invader
|
|
|
Body recognizes______.
|
antigenic surface determinants.
|
|
|
Origin of Immune System
|
Fetus 2mnths after conception; stem cells develope in the bone marrow with variety of stem stem cells.
2 Types: Ex. Erythropoietic- RBC's Ex. Lymphopoietic- Lymph node site |
|
|
Dual System of________.
|
Immunity
|
|
|
CMI ( Cellular Mediated Immunity)
|
Involves T-cells(advcd. life span, more than half circulating), Lymphokines & Interleukins.
|
|
|
Lymphokines
|
Protein produced by lymphoblasts; relates to 2nd level, & increases efficiency of phagocytosis.
|
|
|
Interleukins
|
Produced by WBC's, influences activity of other WBC's.
|
|
|
CMI's are found in 4 Classes of T-Cells:
|
1. Helper T-Cells
2. Supressor T-Cells 3.Cytotoxic T-Cells (Killer T-Cells) 4. Delayed-hypersensitivity (Memory T-Cells) |
|
|
Helper T-Cells
|
Signal to produce more T-cells.
|
|
|
Supressor T-Cells
|
Reduce production of T-cells.
|
|
|
Cytotoxic T-cells (Killer T-Cells)
|
Destroy antigens
|
|
|
Delayed- hypersensitivity (Memory T-Cells)
|
Destroy future,reappearing non-self foreign antigens, resulting in long term immunity.
|
|
|
_____ & ______ aid in B-Cell production & reduction.
|
Helper T-Cells & Supressor T-Cells
|
|
|
B-Cells remain in ______.
|
Lymphoid tissue, called plasma cells.
They go through many adaptations; end result is production of antibodies. |
|
|
Humeral Immunity
|
Rises from our B cells
|
|
|
Antibody
|
Globulin groups of protein
|
|
|
Immunoglobulins "aka" ___.
|
Antibodies
|
|
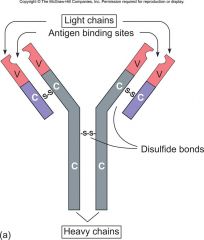
Antibody Structure
(Essay Question) |
Derived from B-cells, part of the humeral immunity & the structure is 4 chains of protein, connected by disulfide bonds. There are contrast regions & variable regions. Constant remains constant & variable changes. The antigen binding site or idiotypic binding site.
|
|

5 Groups of Immunoglobulins (Ig)
|
1. IgG- Monomer
2. IgM- Pentamer (Monster/ penta-5) 3. IgA- Dimer (spend your dimes at IGA) 4. IgD- Monomer 5. IgE- Monomer |
|
|
IgG
|
Monomer; single sub unit, most abundant. Generally everywhere. Crosses walls of vessels& placenta. Principle component in 2ndary response.
|
|
|
IgM
|
Pentamer; 5 put together, too large to fit through tissue (a monster) Principle component of primary response & is important in 2ndary response. Has no where to go but in the circulatory system.
|
|
|
IgA
|
Dimer; Contained in tears, saliva & breastmilk
|
|
|
IgD
|
Monomer- Don't know what it does. Involved in immune response.
|
|
|
IgE
|
Monomer; Great role with allergic response. Ellergic
|
|
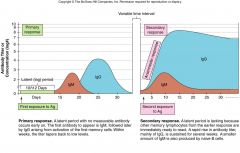
Primary & 2ndary Antibody Response
(Essay Question) |
Body will develope antibody to the antigen. 1st exposure to antigen-primary response- IgM arrives first (huge in the circulatory system) followed by IgG. Once IgG experiences that primary, after a variable time interval, the 2ndary exposure to antigen- IgM will still arrive 1st, but IgM will arrive more rapidly and at a higher level of concentration.
|
|
|
Surface determinants
|
Pathogens can have several antigenic surface determinants. It's a chemaical communication. The body memorizes these determinants & has seen them before.
|
|
|
2 Types of Im
|
Innate & Aquired
|
|
|
Innate
|
what you were born with, your genetic make-up.
. |
|
|
Particular people who don't have innate immunity:
|
Native Americans- Without innate immunity to small pox.
Polynessians- Without innate immunity to measles |
|
|
Aquired
|
after you were born, usually not inherited.
|
|
|
2 groups of Aquired Im
|
Long term Im & Short term Im
|
|
|
Longterm Im
|
Naturally active aquired Im. Direct exposure to the disease
Ex. Measles & Mumps |
|
|
Artificial Aquired Active Im through ____.
|
vaccination
1st generation vaccines; |
|
|
3 Groups of Whole cell
|
Whole cell, Whole Virus, & Whole Toxin
|
|
|
Whole Cell
|
Killed, inactivated, safer, but could be less effective. Many side effects
Ex. Typhoid Fever |
|
|
Whole Virus
|
Ex. Rabies ( Pasteur 1985)
|
|
|
Whole Toxin
|
Tetanus
|
|
|
Attenuated Vaccinations
|
Not killed, it's alive, but weakened. Antibody created quickly with more quantity.
Ex. Polio Vaccine (1954) Sabin- Oral Polio Vaccine ( created 1-2yrs later) |
|
|
Short term Im
(Part of Essay question) |
Naturally aquired Passive Im. Can occur from mother to child via placenta transfer and after birth via breastmilk.
|
|
|
Artificial Aquired Passive Im
Part of Essay Question) |
Injected into the body due to exposure to the disease
|
|
|
Gamma globulin
|
Several types available. Hep. A & Hep. B Must have vaccination for both.
|
|
|
Hepatitus A
(use in essay Q) |
Foodborne
|
|
|
Hepatitus B
(Use in Essay Q) |
Bloodborne
|
|
|
ISG ( Immune Serum Globulin)
(Essay Q) |
Created from horse serum, caused lots of adverse reactions, now usr ISG ( Immune Serum Globulin). Used to treat Hep. A. Is collected from the pool of blood of 1,000 blood donors.
|
|
|
SIG (Specific Immune Globulin)
(Essay Q) |
Pooled from serum from convalescing pt's who had the disease. Used to treat Hep. B. Contain higher specific antibodies.
|
|
|
Vaccine
|
Suspension of Mo's that will induce Im when introduced into the pt. Provides specific Im, defense, & resistance. They are a preventative maintenance, not a cure.
|
|
|
Sub unit Vaccinations
|
Genetically engineered antigenic protein from the Mo's cell not the whole cell.
|
|
|
Acellular
|
Using the whole cell, Using antigenic fragments of the cell.
|
|
|
Anti-idiotypic
|
Harmless. Antigen from Mo that mimics an antibody.
|
|
|
Serology
|
Branch of Immunology & deals with in vitro testing.
|
|
|
In Vitro
|
Remove blood into a test tube for diagnostic testing. Antibody/antigenic properties. If there's surface determinants, then you've been exposed. Test can reveal what has invaded you and how to treat it.
|
|
|
5 Different groups of Serilogical Testing Methods
|
1. Agglutination Tests
2. Percipitation Tests 3. Complement Fixation 4. Immunoflourescence 5. Immunoassays |
|
|
Agglutintation Tests
|
Will show visible clumping.
1. Measure antibody level 2. Looking for highest dilution that gives antibody reaction Looking for high titer levels. Titer tests can tell if you have had the disease or vaccine. |
|
|
Percipitation Tests
|
Will show bands
|
|
|
Complement Fixation
|
Looking for Lysin
|
|
|
Immunoflourescence
|
Uses dye, Flourochrome
|
|
|
Immunoassays
|
2 groups: RIA & ELISA
|
|
|
Radioimmunoassay (RIA)
|
Radioactive labeling
|
|
|
Enzyme Linked Immuno Sorbent (ELISA)
|
Uses enzymes and dyes to detect antibody complexes.
|
|
|
Immunopathology
|
Study of disease associated with accesses or difficiencies with the immune response.
|
|
|
2 Groups of Antigens
|
Exogenous & Endogenous
|
|
|
Exogenous
|
Outside the body. Ex. Pollen
|
|
|
Endogenous
|
Inside the body from self tissue called autoimmunities.
|
|
|
Gell & Coombs hypersensitivity
|
Classification of allergic responses
|
|
|
Allergys
|
Exaggerated immune response to an allergen(substance that promotes or provokes an allergic response)
|
|
|
Type 1
|
After 2nd contact, specific B(lymphocyte)-Cells react within 30min or less with the allergen. Invades IgE & histamine. Is immediate. 2 varriations based on local & astymic.
|
|
|
Atrophy
|
Local & chronic
Ex. Pollen allergy (Hay fever) |
|
|
Anaphylaxis
|
Systemic & acute, explosive.
Ex. Anaphylactic shock(airway obstruction) |
|
|
Epinephrine
|
Antihistamine
|
|
|
Type 2
|
Antibody mediated. After 2nd contact with specific B-Cells. Is within hrs or days. Involves IgG, IgM, & Compliment.
Ex. Type & cross-match. Hymolitic disease of a newborn.Rh factors of mom(-) and baby(+) don't match. Mom's body sees the baby Rh(+) as an invader and wants to destroy it. |
|
|
RhoGam
|
Gamuglobulate given with 1st pregnancy to moms with an (-) Rh factor at 24wks, to prevent any issues.
|
|
|
Type 3
|
After 2nd contact with specific B-cells, reacts within hrs or days and involves IgG,IgA, IgM & complement. Immune complex is trapped & causes chronic inflammation.
2 Types of syndromes: Systemic- Serum Sickness Local- Arthus reaction |
|
|
Autoimmunities
|
Non-self molecule auto antigenis the unrecognized self tissue & would form T-cells that are synthesized to antibodies. Antibodies are produced to unrecognized auto antigens.
Ex. SLE- Systemic Lupus Erythematosus RA- Rheumatoid Arthritis |
|
|
Type 4
|
T-Cell mediated; Cytotoxin T-cells react with in 1 to many days or months. Response to self tissue or transplanted tissue.
|
|
|
Self tissue response
|
delayed allergic response
|
|
|
Tuberculin test, Transplanted tissue
|
Host would reject the transplant
|
|
|
Graft
|
time frame within 2 weeks(14 days), body will reject the graft.
|
|
|
Graft vs. Host disease
|
Graft begins to reject,
bone marrow transplant- rejection can occur from 3mnths to 10mnths |
|
|
Tissue typing
|
Major histocompatibility complex (MHC) or known as Human Leukocyte Antigen Complex (HLA)- Identify pt. tissue and type the tissue
|
|
|
Transplantation tissue grfts has______ &______.
|
Privileged tissue & Privileged Sites
|
|
|
Privileged tissue
|
Tissue safe from rejection
ex. pig valves |
|
|
Privileged sites
|
Sites where antibodies do not circulate.
Ex. Cornea & Brain |
|
|
4 Basic Types of Grafts
|
1. Autograph
2. Isograft 3. Allograft 4. Xenograft |
|
|
Autograph
|
Burn victims (face, ears) remove skin off same person from a large surface area. Some MHC
|
|
|
Isograft
|
Balanced, from identified twin(don't tissue type). If older, affected by disease or health MHC can change.
|
|
|
Allograft
|
Most common type. Individuals of same species. Does require tissue type testing. Human to human. Will need immunosupressives.
Ex. Ayclosparin A, Steroid, Prednisone |
|
|
Xenograft
|
Graft between 2 different species, Organs from animal. Can be temporary. Artificial as well.
|
|
|
2 Groups of Immunodificiency Diseases
|
1. Primary
2. Secondary |
|
|
Primary
|
Disease that is genetic. Born with it. B-cell defect (Ab) lacks the body to produce antibodies.
Ex. Agammaglobulinemia (deficit of B-cells) Di George Syndrome- (Deficit in T-cells) With out a Thymus. B & T-Cell deficit- No immune system at all. Fatal without transplant or live in a speacial facility. |
|
|
Secondary
|
Aquired after birth. Damage to the immune system.
Ex. Aids ( Aquired immunodificiency Syndrome)- T-Helper cells are the main target. Cause opportunistic infections, & cancer. |
|
|
Tumor
|
New growth of abnormal cells, caused by mytosis gone wild.
|
|
|
Types of Tumors
|
Benign, Malignant, Metstasize
|
|
|
Local
|
Considered Benign
|
|
|
Malignant
|
Cancerous
|
|
|
Mestastasize
|
Goes Systemic
|
|
|
Neoplasm
|
Another name for cancer
|
|
|
Oncology
|
Medical specialty regarding the study of cancer
|
|
|
Theory for Cancer
|
Basic Mechanism Theory of Transformation of cancer.
|
|
|
Oncogene
|
Cancer gene
|
|
|
Anti Oncogene
|
The tumor suppressing gene & regulates tumor suppression & the protein oncogene.
|
|
|
Proto- oncogene
|
Regulates start of mytosis
|
|
|
Genetic disruption occurs
|
Oncogene takes control, over-riding the stop of mytosis, resulting in immortalization.
|
|
|
Immortalization
|
Non-stop cell division of new growth of a tumor(abnormak cells) , and then goes systemic.
|
|
|
Genetic disruptions (systemic)
|
How viruses play in this: Some viruses cause cancer. There are DNA & RNA viruses NOT BOTH!!
|
|
|
RNA ( Retroviruses)
|
Some contain an enzyme called revostranscriptase, & uses it to synthesize it's nucleic acid in the host.
Ex. T-cell leukemia |
|
|
DNA Virus
|
HPV ( Human Papillomavirus)- May cause cervical cancer
|
|
|
Immune Surveillance
|
Patrolling cells for particular abnormal cells. After locating them they will begin to destroy abnormal cells, unless we have antigen modulation. ( can shed determinants)
|
|
|
3 Types of Abnormal cells
|
Cytotoxic T-Cells
NK's ( Natural Killers) LAK ( Lymphokine Activated Killers) |
|
|
Essay 1. Compare & Contrast Primary & Secondary Antibody Response. Draw and explain drawing.
|
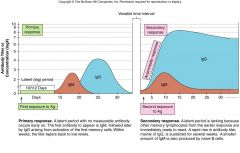
Body will develope antibody to the antigen. 1st exposure to antigen-primary response- IgM arrives first (huge in the circulatory system) followed by IgG. Once IgG experiences that primary, after a variable time interval, the 2ndary exposure to antigen- IgM will still arrive 1st, but IgM will arrive more rapidly and at a higher level of concentration
|
|
|
Essay2.
Draw, Label & Explain antibody structure and include discussion on all immunoglobulin classes. (monomer, variable, Constant) |
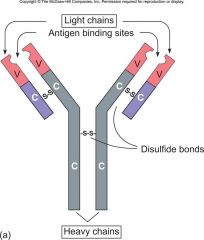
Derived from B-cells, part of the humeral immunity & the structure is 4 chains of protein, connected by disulfide bonds. There are contrast regions & variable regions. Constant remains constant & variable changes. The antigen binding site or idiotypic binding site.
5 Groups of Immunoglobulins (Ig) 1. IgG- Monomer;single sub unit, most abundant. Generally everywhere. Crosses walls of vessels& placenta. Principle component in 2ndary response. 2. IgM- Pentamer (Monster/ penta-5) 5 put together, too large to fit through tissue (a monster) Principle component of primary response & is important in 2ndary response. Has no where to go but in the circulatory system. 3. IgA- Dimer (spend your dimes at IGA) Contained in tears, saliva & breastmilk 4. IgD- Monomer; Don't know what it does. Involved in immune response. 5. IgE- Monomer; Great role with allergic response. Ellergic |
|
|
Essay 3.
List format, the basic mechanism of transfer theory of cancer. |
Oncogene - Cancer gene
Anti-oncogene - The tumor suppressing gene & regulates tumor suppression & the protein oncogene. Proto- oncogene- Regulates start of mytosis Genetic disruption occurs; Oncogene takes control, over-riding the stop of mytosis, resulting in immortalization. Immortalization - Non-stop cell division of new growth of a tumor(abnormak cells) , and then goes systemic. There are DNA & RNA viruses NOT BOTH!! RNA ( Retroviruses) - Some contain an enzyme called revostranscriptase, & uses it to synthesize it's nucleic acid in the host. Ex. T-cell leukemia DNA Virus - HPV ( Human Papillomavirus)- May cause cervical cancer Genetic disruptions (systemic) |
|
|
Essay 4.
Passive Immunity in regard to artificially aquired passive immunity as discussed in lecture. ( Hep. A,B,C, SIG, treatment) |
Longterm Im- Naturally active aquired Im. Direct exposure to the disease
Ex. Measles & Mumps Artificial Aquired Active Im through vaccination 1st generation vaccines; 3 Groups of Whole cell Whole Cell -Killed, inactivated, safer, but could be less effective. Many side effects Ex. Typhoid Fever Whole Virus- Ex. Rabies ( Pasteur 1985) Whole Toxin- Tetanus Naturally aquired Passive Im. Can occur from mother to child via placenta transfer and after birth via breastmilk Artificial Aquired Passive Im- Injected into the body due to exposure to the disease ISG ( Immune Serum Globulin) Created from horse serum, caused lots of adverse reactions, now usr ISG ( Immune Serum Globulin). Used to treat Hep. A. Is collected from the pool of blood of 1,000 blood donors. SIG (Specific Immune Globulin) Pooled from serum from convalescing pt's who had the disease. Used to treat Hep. B. Contain higher specific antibodies. |

