![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
36 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Fracture definition |
Discontinuity of bone |
|
|
|
Categories of fractures According to CAUSE |
1. Pathological (bone weakened by pre-existing disease) 2. Stress fracture (repeated loading on normal bone) 3. Traumatic (low- or high-energy) |
|
|
|
Pathological fracture causes |
1. Metabolic disease 2. Infections (most commonly bacterial, never viral) 3. Malignancy (1ry or 2ry) |
|
|
|
Most common sources of 2ry bone malignancy |
Breast in females Prostate in males Lung, kidneys, and thyroid in both |
|
|
|
Categories of fractures According to LOCATION |
1. Epiphyseal (causes joint stiffness, difficult reduction, intra- or extra-capsular) 2. Diaphyseal (need stabilization/fixation 3. Metaphyseal (causes mal-union>non-union) 4. Growth plate fractures (Salter-Harris Classification) |
|
|
|
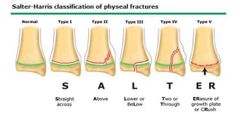
Salter-Harris Classification |
1. Shearing force parallel to growth plate, hypertrophic layer is affected, usually due to directtrauma 2. Shearing force with bending but the fracture only involves the metaphysis and maybe thegrowth plate 3. Shearing force with bending but the fracture only involves the epiphysis and maybe thegrowth plate 4. Shearing force with bending but the fracture involves the metaphysis, goes through thegrowth plate, and to the epiphysis 5. Perpendicular axial force, leads to crushing of growth plate and germinal layer, mostly due tofalling down will still standing |
For growth plate fractures |
|
|
Salter-Harris Classification Photo |
|
For growth plate fractures |
|
|
Categories of fractures According to STATUS OF SOFT TISSUE |
1. Closed fractures 2. Open fractures (communication through traumatic wound to surrounding environment) |
|
|
|
Gustilo and Andersen Classification |
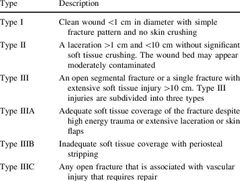
|
Classification of open wounds |
|
|
Open Fracture Management |
ATLS, Analgesia, Anti-tetanus, Antibiotics (upon arrival, 1st gen cephalosporines and penicillins), Adequate irrigation, Debridement (within 4-8 hrs) |
|
|
|
Categories of fractures According to MECHANISM OF INJURY |
1. Direct (Tapping, Crush, Penetrating) 2. Indirect (Traction, Angulation, Rotational, Compression, and Axial compression) |
|
|
|
Tapping Injury |
Small force on small area transverse fracture on long bones of legs and arms |
|
|
|
Crush injury |
Large force on large area Extensive soft tissue damage Transverse fracture or comminuted |
|
|
|
Penetrating injury |
Large force on small area Velocity is more important than mass Low- vs high-velocity |
|
|
|
Traction injury |
Transverse fracture Most common in patella, olecranon, and medial maleolus |
|
|
|
Angulation injury |
Transverse fracture or with triangular fragment Convexity under tension Concavity under compression |
|
|
|
Compression injury |
T or Y shaped fracture Common in femur and humerus |
|
|
|
Clinical features of fractures |
*pain, loss of function, deformity *abnormal mobility and crepitations *neurovascular injury *X-ray findings |
|
|
|
Management of fracture patients |
1. Life: ATLS 2. Limb: decompression if tgere is compartment syndrome 3. Wound: if open (tetanus, antibiotics, irrigation) 4. Fracture *always prevent further soft tissue damage, analgesia, decrease incidence of fat embolism and shock |
|
|
|
Management of fracture by |
1. Reduction (open, or closed) 2. Immobilization (traction, cast, externral/internal fixation) 3. Rehabilitation |
|
|
|
Treatment Reduction |
Metapheseal bone can accept more deformity (~20°) than diaphyseal bone (~10°), has better remodeling |
|
|
|
Treatment Fixation |
Screws: absolute stability/must not cross growth plate (in pediatrics) K-wires: no absolute stability/can cross growth plate |
|
|
|
Healing calender |
Child + Upper Limb (standard) = 3weeks Lower limb x2 Adult x2 Greenstick fracture x2 Smoker x2 Consolidation (more callus formation) x2 Remodeling (translucent canal) x2 Transverse fracture x1.5 (oblique fracture has better healing) |
|
|
|
Complications of fractures |
1. Bone healing abnormalities (non-, mal-, and delayed union, AVN) 2. Infections 3. Pulmonary problems (PE, ARDS) 4. Soft tissue injury (arterial and nerve injuries, compartment syndrome) 5. Bleeding disorder 6. Other: complex regional pain syndrome (CRPS) , osteoarthritis, and myositis ossificans |
|
|
|
Pediatric VS Adult Skeleton |
1. Presence of growth plate (londitudinal growth) and perichondral plate (bone thickness) 2. Thick periosteum (prevents dislocatiom of fracture) 3. More cancellous bone (less propagation of fracture) 4. More radiolucent on X-ray (cartilagenous>ossified bone) (may underestimate fracture) 5. Tensile strength of ligaments>bone (bone is injured more) |
|
|
|
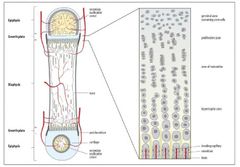
Layers of Growth Plate |
1. Germinal: most important, 1st near epiphysis 2. Proliferative 3. Hypertrophic: weakest due to increased size of cells so less cell numbers, and more fluid and less connections between cells 4. Zone of provisional calcification |
|
|
|
Layers of Growth Plate PHOTO |
|
|
|
|
Prognostic factors of growth plate fractures |
1. Severity of fracture (Salter-Harris Classification)(higher class has worse prognosis) 2. Age (younger is worse prognosis) 3. Physis injured (contribution to growth potential) 4. Anatomic type of fracture 5. Treatment 6. Displacement in same plane of motion (better prognosis) |
|
|
|
Contribution to growth potential |
The higher the growth potential the better prognosis Lower limb: around the knee (distal femur and proximal tibia) Upper limb: away from the elbow (proximal humerus and distal radius) |
|
|
|
Epiphysial Plate (Growth Plate) |
Hyaline cartilage plate in metaphysis at each end of a long bone, it is the part where new bone growth takes place Found in children and adolescents, and is replaced by epiphyseal line in adults |
|
|
|
Common sites of fractures in pediatric age groups |
INFANTS: diaphysis (1st ossification) TODDLERS: metaphysis ADOLESCENTS: epiphysis |
|
|
|
Upper limb fractures Most common mechanism of injury |
Falling on outstretched hand |
|
|
|
Upper limb fractures Mechanism of injury reflects |
1. Extent of soft tissue injury (which affects bone healing) 2. Displacement of fracture |
|
|
|
Upper limb fractures Displacement depend on: |
1. Mechanism of injury 2. Muscle pulling |
|
|
|
Upper limb fractures On Physical Exam |
1. If there is a visible deformity: most likely the fracture is displaced 2. Assess distal neurovascular bundles (radial, ulnar, and median nerves, and radial and ulnar vessels) 3. Stiffness occurs in fractures near joints |
|
|
|
Upper limb fractures Displacement of fractures |
Always distal piece in relation to proximal piece 1. Translation: medially/laterally 2. Angulation: vulgus/varus or anterior/posterior 3. Rotation: assessed by x-ray including joints above and below, or by assessing thickness of cortex |
|

