![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
88 Cards in this Set
- Front
- Back
|
A liver biopsy shows large hepatocytes filled with finely granular, homogeneous, pale cytoplasm |
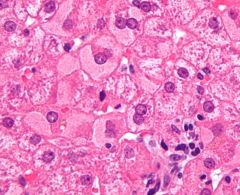
Hepatitis B: causes hepatocellular cytoplasm to fill with HBsAg, fine granular, dull eosinophilic, "ground glass" appearance |
|
|
Headaches, nausea, tremulousness, sweating BP: 200/120 standing 190/110 supine Increase urinary Vanillylmandelic acid excretion CT: Right sided adrenal mass on CT scan Which one is the embryological origin of thyroid cells in this disease? |
Description indicates pheochromocytome, usually associated with MEN syndromes: MEN 1: Pth, Pan, Pit MEN 2A: M.C.Th, Pheo, Pth MEN 2B: M.C.Th, Pheo, Muc. Neuromas Chromaffin cells and parafollicular cells (c-cells) of the thyroid originate from neural crest |
|
|
Phenoxybenzamine description |
Non selective, irreversible a1, a2 adrenergic antagonist that reduces the number of receptors available for norepinephrine binding |
|
|
Mechanism of actions of Thiazolidinediones Pioglitazone, Rosiglitazone |
Decrease insulin resistance by binding to PPARy, alter gene expression and protein synthesis, can result in a delayed in action to several days Up regulates: Glut 4: increase glucose uptake Adiponectin: increase insulin response of adipocytes |
|
|
Mechanism of action of Sulfonylureas 1 generation: tolbutamide, chlorpropamide 2 generation: Glyburide, glimepiride, glipizide |
Increase insulin release from the pancreatic B cells Close K+ channel in B cell, insulin release via increase Ca++ influx |
|
|
Mechanism of action of Biguanides: Metformin |
Non competitive inhibitor of mitochondrial glycerol 3 phosphate dehydrogenase, important for maintaining hepatic redox state. Inhibition of this enzyme causes a significant reduction in hepatic glucose production |
|
|
Hyperthyroidism radioactive therapy 131 I Which substances can decrease the uptake by competitive inhibition? |
Perchlorate and Pertechnetate ions absorbed into the thyroid gland via Na- Iodide symporter |
|
|
15 year old caucasian male with gait instability, frequent falls, kyphoscoliosis, per caves, lower extremity ataxia, impaired position and sensation (dorsal column degeneration) |
Autosomal recessive, mutation chromosome 9, increase number of trinucleotide repeats, Friederich Ataxia, patient most likely will die of cardiomyopathy, also complicated with DM |
|
|
Baby with poor feeding, weakness, constipation, complete loss of extremity muscle tone, vaccines up to date, nutrition fruit and honey. Which test you would ask for? |
Stool for bacterial toxins, looking for C. botulinum spores In adults the same disease can results for consumption of canned foods |
|
|
Patient receives a liver transplant. 1 week after the surgery develops desquamating skin rash, bloody diarrhea, multiple ulcerations of intestinal mucosa. What is the cause? |
(GVHD) Graft vs host disease mediated by T- lymphocytes of the donor tissue that are sensitized against MHC antigens of recipient. Skin, liver and intestine are commonly involved. |
|
|
When a transplant rejection is Hyperacute? |
Within minutes, pre existing recipient antibodies react to donor antigen (type II reaction), activate complement Widespread thrombosis of graft vessels- ischemia/ necrosis Graft must be removed |
|
|
When a transplant rejection is Acute? |
Weeks to months, Cellular: CTL's activated against donor MHC's Humoral: similar to hyper acute, except antibodies develop after transplant Vasculitis of graft vessels wit dense interstitial lymphocytic infiltrate Prevent/ reverse with immunosuppresants |
|
|
When a transplant rejection is Chronic? |
Months to years Recipient T cells perceive donor MHC as recipient MHC and react against donor antigens presented Cellular and humoral Irreversible. T cell antibody- mediated damage Heart atherosclerosis, Lung bronchiolitis obliterans, Liver vanishing bile ducts, Kidney vascular fibrosis, glomerulopathy |
|
|
Oral lesions scraping cells with intranuclear inclusions. |
Herpes simplex virus type 1, Enveloped double stranded DNA, gingivostomatitis |
|
|
What are the types of urinary incontinency, etiology and symptoms? |
Stress: loss of urethral support, IAB pressure exceeds urethral sphincter pressure, due to coughing, sneezing, laughing, lifting Urge: Detrusor overactivity, sudden, overwhelming or frequent need to empty the bladder Overflow: Impaired detrusor contractility, bladder outlet obstruction, constant involuntary dribbling and incomplete emptying. |
|
|
Which one is the most important mediator of coronary vascular dilation? |
Nitric oxide, large arteries, pre arteriolar vessels, synthesized from argininine and O2 by endothelial cels, causes vascular smooth muscle relax ion by a guanylate cyclase mediated cGMP second messenger system. Adenosine, a product of ATP metabolism, acts as vasodilatory in small coronary arterioles |
|
|
Southern Blot, Northern Blot, Western Blot, Southwestern |
DNA, RNA, Protein, DNA binding protein |
|
|
Cardiac tissue conduction velocity, faster to slower |
Purkinje system, Atrial muscle, Ventricular muscle, AV node Park At Ventura Avenue |
|
|
What is the Kozak sequence? |
Play a role in the initiation of translation (mRNA binding to ribosomes), a mutation 3 bases upstream from the start codon (AUG) in this sequence is associated with thalassemia intermedia. |
|
|
Causes of lactic acidosis |
1) Enhanced metabolic rate (seizures, exercise) 2) Reduced oxygen delivery (cardiac or pulmonary failure, shock, tissue infarction) 3) Diminished lactate catabolism due to hepatic failure or hypo perfusion 4) Decreased oxygen utilization (cyanide poisoning) 5) Enzymatic defects in glycogenolysis or gluconeogenesis |
|
|
How decrease oxidative phosphorylation in septic shock increases anion gap? |
In septic shock there is an impaired tissue oxygenation, leading to the shunting of pyruvate to lactate after glycolysis, increasing the lactic acid formation |
|
|
Name the causes of reversible cell injury (with O2) |
1) ATP depletion 2) Cellular/mitochondrial swelling (decrease ATP-> decrease activity of NA/K pump) 3) Nuclear chromatin clumping 4) Decrease glycogen 5) Fatty change 6) Ribosomal/Polysomal detachment (decrease 7) protein synthesis) 8) Membrane blebbing |
|
|
Name the causes of irreversible cell injury |
1) Nuclear pyknosis, karyorrhexis, karyolysis 2) Plasma membrane damage ( degradation of phospholipid) 3) Lysosomal rupture 4) Mitochondrial permeability / vacuolization Phospholipid- containing amorphous densities within mitochondria |
|
|
How you can enhance morphine tolerance? |
Activation of NMDA receptors by glutamate, increasing phosphorylation of opioid receptors and increasing nitric oxide levels NDMA blockers like ketamine, block the actions of glutamate and decrease morphine tolerance |
|
|
What is the mechanism of erythroblastosis fetalis? |
Most common due to maternal sensitization to Rh during a prior pregnancy with an Rh(D)+ fetus. In subsequent Rh(D)+ pregnancies, maternal anti-Rh(d) IgG antibodies cross the placenta and cause fetal hemolysis Clinical findings: anemia, jaundice, generalized edema (hydrops fetalis), nucleated erythrocytes, extramedullary hematopoiesis. |
|
|
What is Infectious dose ID50%? Name microorganisms that can cause diarrhea with small inoculum |
Corresponds to the minimum number of organisms required to cause disease in 50% of affected individuals Shigella (10-500 cells), Campylobacter jejuni (500 cells), E.Histolytica (1-10 organisms), Giardia lamblia (1-10 organisms) |
|
|
When you use chi square? |
To test the association between 2 categorical variables, patients are divided in 2 groups based on exposure, and the number of patients that experience each outcome is recorded in 2x2 table. |
|
|
When you use two sample zest and two sample t test? |
To compare 2 group of means, not categorical variables, ex. fibrinogen levels as numerical values mg/dL instead of categorically |
|
|
When you use analysis of variance (ANOVA)? |
To compare the means of 2 or more groups. Ex. ANOVA analysis could be used to assess for differences in mean blood pressure among 3 sample populations grouped by exercise status (never exercise, occasionally, frequently) |
|
|
What is the mechanism of the statins? |
Inhibit conversion of HMG-CoA to mevalonate (a cholesterol precursor) Causes hepatocytes to increase their LDL receptor density as a means of increasing their uptake of circulating LDL * LDL decreases, HDL increases, Triglycerides decreases |
|
|
What are the side effects of statins? |
Hepatotoxicity (increase LFT's) rhabdomyolysis (esp with fib rates and niacin) |
|
|
What is the bile acid resins mechanism of action? Cholestyramine, colestipol, colesevelam) |
Prevent intestinal reabsorption of bile acids; liver must use cholesterol to make more *LDL decrease, HLD increase, TGL increase |
|
|
What are the side effects of bile acid resins? |
GI disconfort Decrease absorption of fat soluble vitamins Cholesterol gallstones |
|
|
What is the mechanisms of action of Niacin (B3) as a lipid lowering agent? |
Inhibit lipolysis in adipose tissue; reduces hepatic VLDL synthesis *LDL Decrease, HDL increase, TGL decrease |
|
|
What are the side effects of Niacin used as a lipid lowering agent? |
Red, flushed face, which is decreased by aspirin or long term use. Hyperglycemia (acanthosis nigricans) Hyperuricemia (exacerbates gout) |
|
|
What is the mechanism of action the Cholesterol absorption blockers? Ezetimibe |
Prevent cholesterol absorption at small intestinal brush border *LDL decrease, HDL no change, TGL no change |
|
|
What are the side effects of Cholesterol absorption blockers? Ezetimibe |
Rare, increase LFT's, diarrhea |
|
|
What is the mechanisms of action of the fib rates? Gemfibrozil, clofibrate, benzafibrate, fenofibrate |
Upregulate LPL Increase TG cleareance Activates PPARa to induce HDL synthesis * LDL decrease, HDL increase, TGL decrease a lot |
|
|
What are the side effects of fibrates? |
Myositis (increase risk with statins) Hepatotoxicity (increase LFT's) cholesterol gallstones (esp with bile acid resins) |
|
|
Describe the main characteristics of the Primary Hyperaldosteronism |
Cause: Adrenal hyperplasia or aldosterone secreting adrenal adenoma (Conn syndrome) Hypertension, hypokalemia, metabolic alkalosis, LOW PLASMA RENIN. Normal Na+ due to aldosterone escape = no edema May be bilateral or unilateral Tx: Surgery to remove the Tu and or spironolactone |
|
|
Describe the main features of the Secondary Hyperaldosteronism |
Cause: Renal perception of low intravascular volume results in an overactive renin- angiotensin system Due to Renal artery stenosis, CHF, cirrhosis, nephrotic syndrome. HIGH PLASMA RENIN Tx: Spironolactone (K+ sparing, aldosterone agonist) |
|
|
What is the mechanism of action of Methotrexate? |
Folic acid analog that inhibits dihydrofolate reductase, decrease dTMP, decrease DNA, and protein synthesis |
|
|
What are the side effects of Methotrexate? |
Myelosuppression (reversible with leucovorin (folinic acid)) Macrovesicular fatty change in liver Mucositis Teratogenic Stomatitis |
|
|
Why is important the bacterial growth pattern "Serpentine cords" in Mycobacterium Tuberculosis? |
Secondary to the presence of a cord factor a mycoside (2 mycolic acid), establish virulence through neutrophil inhibition, mitochondrial destruction and release of TNF |
|
|
A patient experience blurred vision after ingest several tablets of diphenhydramine, why? |
H1 receptor blockers decrease the activity of this receptor increasing the proportion of inactive H1 receptors (reverse blockade) 1st generation antihistaminics (Clorpheniramine, diphenhydramine) have antimuscarinic, anti a adrenergic, anti serotonergic properties Anticholinergic: pupillary dilation (blurry vision) muscarinic, dry mouth, urinary retention, constipation. |
|
|
Patient with V/Q defect that does not match a ventilation defect in the lungs? |
Deep vein thrombosis that cause a pulmonary embolism |
|
|
Most common cause of fetal hydronephrosis |
Inadequate recanalization of the ureteropelvic junction, the junction between the kidney and the ureter |
|
|
Role of lysosomal enzymes for abscess formation |
Digest the offending pathogens, and tissue debris, chemotactically summon additional neutrophils or macrophages to the area. Occasionally the enzymes will also damage the surrounding parenchyma, setting the stage for abscess formation |
|
|
Chloroquine is the Tx of choice for uncomplicated malaria, it eliminates susceptible erythrocytic forms of all Plasmodia species, why adding Primaquine is needed? |
To treat P.vivax, P ovale in roder to eradicate the intrahepatic stages of these 2 malarial species and prevent relapsing. |
|
|
What is the leukemia related with Trisomy of 21? |
Acute lymphoblastic leukemia Acute myelogenous leukemia |
|
|
Patient with "right hand clumsiness", decrease sensation over the 5th finger, flattened hypothenar eminence, which nerve is injured and where? |
Ulnar nerve injury "claw hand" deformity, can be injured either near the medial epicondyle of the humerus or in Guyon's canal near the hook of the hamate and pisiform bone in the wrist |
|
|
Damage of which nerve will result in wrist drop? |
Radial nerve provides sensory innervation to the skin of the posterior arm, forearm, and dorsal lateral hand, motor innervation to all of the extensor muscles of the upper limb below the shoulder. |
|
|
Site of action of: 1) Acetazolamide 2) Mannitol 3) Furosemide 4) Hydrochlorothiazide 5) Amiloride 6) Spironolactone |
1) Proximal tubule 2) Descendind limb of Henle's loop 3) Thick ascendinf limb of Henle's loop 4) Distal convoluted tubule 5) Collecting duct (Na+ channel blocker) 6) Collecting duct (Aldosterone receptor antagonist) |
|
|
Patient with DM1, uncontrolled voiding without any sensation of a full bladder , chronic kidney disease, gastroparesis, why? |
DM1 can cause overflow incontinence due to inability to sense a full bladder and incomplete emptying. Post void residual testing with ultrasound or catheterization can confirm inadequate bladder emptying |
|
|
Describe the permeability of the nephron to H2O by section |
1) Proximal tubule, descending limb of Henle loop- HIGH 2) Ascending limb of Henle loop, early convoluted tubule- NON 3) Late distal convoluted tubule, collecting duct system- ADH VARIABLE |
|
|
Patient newly dx with seizures, fever, skin rash, T38.9C, confluent erythema 60% of the body, generalized lymphadenopathy, symmetrical facial swelling, what is the diagnosis? |
DRESS syndrome 2-8 weeks after exposure to a drug, anticonvulsivants, allopurinol, sulfonamides, antibiotics Affected organs: Liver (hepatomegaly, jaundice), kidney (acute interstitial nephritis), lung (cough, dyspnea) Labs: Eosinophilia, atypical lymphocytosis, elevated ALT Improve with suspension of the drug |
|
|
Patient with fatigue (slow onset), stools pale gray Liver biopsy: dilated bile canaliculi wit green brown plugs and yellowish green accumulations of pigment within the hepatic parenchyma. What is the relationship of this syndrome and osteomalacia? |
DIgestive disorders such as cholestasis can cause malabsorption and nutritional deficiencies, of the fat soluble vitamins, one of them Vit D |
|
|
Why Chron's disease is associated with oxalate kidney stones? |
Impaired bile acid absorption in the terminal ileum leads to loss of bile acids in feces with subsequent fat malabsorption. Lipids then bind Ca++ and the resulting soap complex is excreted. Free oxalate is absorbed and forms urinary calculi |
|
|
E.coli grown on a lactose containing medium up-regulate the production of the enzymes B-galactosidase and galactoside permease Which of the following best explains the synchronous production of both enzymes in response to lactose? |
Bacterial mRNA can be polycistronic, one mRNA codes for several proteins mRNA is the bacterial lac operon, wich codes for the proteins necessary for lactose metabolism, transcription, translation, all regulated by a single promoter, operator |
|
|
Describe the mechanisms: 1) Alcohols 2) Chlorhexidine 3) Hydrogen peroxide 4) Iodine |
1) Disruption of cell membranes, denaturation of proteins 2) Disruption of cell membranes, coagulation of cytoplasm 3) Produces destructive free radicals that oxidize cellular components 4) Halogenation of proteins- nucleic acids |
|
|
What is reassorment? Which virus can do this? |
Exchange of entire genome segments Orthomyxoviruses (Influenza) Rotaviruses |
|
|
What are the cells most susceptible to ischemia in the SNC? |
1) Pyramidal cells of the hippocampus 2) Neocortex and the Purkinje cells of the cerebellum The hippocampus is the first area damaged during global ischemia |
|
|
Mechanism of action of Biphosphonates |
Chemical structure similar to pyrophosphate and attach to hydroxyapatite binding sites on bony surfaces to inhibit bone resorption by mature osteoclasts |
|
|
Patient with blurred vision while cutting trees, T38.9C, BP:100/70 mm/hg, pulse: 120/min, reps: 22/min. PE: Flushed skin and dry oral mucosa Pupils dilated and non reactive to light Dx and tx? |
Jimson Weed (datura stramonium) poisoning, also called "Gardener mydriasis) Belladona alkaloids (anticholinergic properties) Jimson weed and Atropine poisoning are similar Can be reverted with cholinesterase inhibitors (physostigmine) |
|
|
Hepatic angiosarcoma is associated with the exposure to: |
Arsenic, Throrotrast, polyvinyl chloride Tu cells express CD31, an endothelial cell marker |
|
|
3 month male, neurological abnormalities, impaired tetrahydrobiopterin synthesis. Which neurotransmitter is deficient in this patient? |
Serotonin, because BH4 is a cofactor used by hydroxyls enzymes in the synthesis of tyrosine, dopa, serotonin, NO. Serotonin is synthesized from tryptophan, initial step is catalyzed by enzyme uses BH4 as a cofactor Dihydrobiopterin reductase deficiency causes defective regeneration of BH4 and is an uncommon cause of PKU. |
|
|
1) Dorsal pancreatic bud structures 2) Ventral pancreatic bud structures |
1) Body, tail, most of the head 2) Wirsung (major pancreatic duct) Failure of the dorsal and ventral pancreatic buds to fuse leads to pancreas divisum. Accessory duct drain the majority of the pancreas |
|
|
Activity related joint pain and periodic morning stiffness, firm nodules over the distal interphalangeal joints |
Osteoarthritis Be aware that for Ddx rheumatoid arthritis typically affects the metacarpophalangeal and proximal inerphalangeal joints |
|
|
Metabolic alkalosis Features: High blood pH, bicarbonate, pCO2 When is saline responsive? When is saline unresponsive? |
Saline responsive: Vomiting/nasogastric suctioning and thiazide/loop diuretic use cause volume and Cl- depletion (low urine chloride) Saline unresponsive: Hyperaldosteronism (high urine chloride) |
|
|
Mechanism of action of fenoldopam |
Parenteral agent, seective D1 receptor agonist Causes arteriolar dilation and natriuresis Improve renal perfusion, used for hypertensive crisis |
|
|
Clinical presentation for organophosphate poisoning (excessive CHOLINERGIC STIMULATION) |
D: Diarrhea- Diaphoresis U: Urination M: Miosis B: Bronchospasm- Bronchorrhea- Bradycardia E: Emesis L: Lacrimation S: Salivation Also muscular excitation, only symptom that atropine cannot reverse |
|
|
Atropine side effects (ANTI CHOLINERGIC- MUSCARINIC ANTAGONIST) |
Hot as a hare Dry as a bone Red as a beet Blind as a bat Mad as a hatter |
|
|
Hydrocephalus presentation |
Irritability, poor feeding, increased head circumference, enlarged ventricles on CT Long term sequelae of hydrocephalus: lower extremity spasticity due to stretching of periventricular pyramidal tracts, visual disturbances, and learning disabilities |
|
|
Haemophilus Influenza requires X (hemantin) and V (NAD+) factors for growth |
Growing with S.Aureus demonstrate the satellite phenomenon where this bacteria produce needed X and V factors for H. Influenza |
|
|
What do you use when ultrasound is inconclusive for acute cholecystitis? |
Nuclear medicine hepatobiliary scanning (cholescintigraphy) |
|
|
Primary hyperaldosteronism 1) Sodium 2) Potassium 3) Bicarbonate |
Primary hyperaldosteronism 1) Normal 2) Low 3) High |
|
|
Dx test for cryptococcus neoformans |
India ink staining in the CSF Mucicarmine staining of lung tissues and bronchoalveolar washings |
|
|
Menstrual cycle |
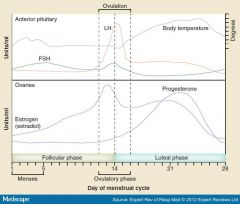
|
|
|
MHC II |
APC for interaction with T-lymphocytes Failure to acidify lysosomes would lead to to deficient expression of MHC II bound to foreign antigen and subsequent lack of interaction between APC's and T-cells |
|
|
TH1 1) Immunity 2) Function 3) Secretion 4) Results IL-12 stimulates the differentiation into TH1, without this = mycobacterial infections, Tx:IFN-y |
TH1 1) Cell mediated 2) Activate macrophages and cytotoxic T- cells 3) IL-2, IFN-y, lymphotoxin B 4) Cytotoxicity, delayed hypersensitivity |
|
|
TH2 1) Immunity 2) Function 3) Secretion 4) Results IL4 promotes the differentiation from naive |
1) Humoral (antibody- mediated) 2) Activate B-cells, promote class switching 3) IL-4, 5, 10, 13 4) Secretion of antibodies |
|
|
Atropine intoxication, can be emulated by? |
Tricyclic antidepressants (amitriptyline) |
|
|
Cardiac output |
CO= Stroke volume x Heart rate CO= O2 consumption/ arteriovenous O2 difference |
|
|
Antifungals mechanism of action 1) Cell wall 2) Cell membrane 3) DNA&RNA synthesis |
1) Echinocandins (caspofungin, micafungin) inhibits glucan from cell wall 2) Triazoles (Keto,fluco,itra,vori) inhibit ergosterol synthesis Polyenes (Anfot B, nystatin) Bind ergosterol molecules in fungal cell membranes, creating pores and lysis Allylamines (terbinafine) synthesis ergosterol [squalene epoxidase] 3) Pyrimidines (Flucytosine) converted to 5-fluoracil within the fungal cell and interferes with RNA and protein synthesis |
|
|
Patient with lump in neck, grow slowly, smoker, biopsy reveals abnormal cells with t(14:18) chromosomal translocation |
Follicular lymphoma (B lymphocytes) translocation between chromosomes 14 and 18 which causes Bcl-2 over expression (protoncogene) |
|
|
Causes of pure red cell aplasia |
Thymoma, lymphocytic leukemias, parvovirus B19 infection |
|
|
Avidly Bromodeoxyuridine uptake, what does it mean?! |
High number of tumor cells in S phase, that are present, high grade, poor prognosis |
|
|
Diminished relaxation of cricopharyngeal muscles during swallowing results in increased intraluminal pressure in the oropharynx. What happens if the mucosa herniate through a zone of muscle weakness in post hypo pharynx? |
I form a Zenker diverticulum, presents in elderly patients with oropharyngeal dysphagia, halitosis, regurgitation , recurrent aspiration |

